Polypharmacy Risk Calculator
Your current medication count affects your risk of serious side effects. This tool estimates your risk based on published medical research.
When you take a new medication, your doctor doesn’t just look at your current symptoms. They’re also reading your past. Your medical history isn’t just background noise-it’s a roadmap that tells them exactly how your body might react to a drug. And sometimes, that roadmap leads straight to dangerous side effects you never saw coming.
Why Your Past Medications Matter More Than You Think
If you’ve had a bad reaction to one drug, you’re far more likely to react badly to another-even if it’s from a different class. That’s not guesswork. Studies show patients with a history of adverse reactions to one medication have a 30-40% higher chance of reacting to similar ones. For example, someone allergic to penicillin has an 8-times higher risk of reacting to cephalosporins, even though they’re technically different antibiotics. This isn’t coincidence. It’s cross-reactivity: your immune system or liver enzymes still remember the old trigger.
And it’s not just allergies. If you’ve ever had nausea, dizziness, or a rash after taking a drug, that’s data. That’s a warning sign your body didn’t handle it well. Yet, a 2022 Johns Hopkins study found that only 35% of electronic health records properly flag these past reactions when doctors write new prescriptions. That means nearly two out of three patients are being prescribed meds without their history being fully considered.
Polypharmacy: The Silent Killer in Your Medicine Cabinet
Taking five or more medications at once? You’re not alone. But you are at serious risk. According to the British Heart Foundation’s 2023 report, people on five to nine drugs have twice the risk of a bad reaction compared to those on fewer. If you’re on ten or more? Your risk jumps over threefold. That’s not a typo. It’s a statistical earthquake.
Each extra pill adds 7-10% more risk. Why? Because drugs don’t just work on their own-they interact. Warfarin, a blood thinner, mixed with common NSAIDs like ibuprofen, can cause dangerous bleeding. That combination alone sends 34,000 Americans to the ER every year. And if you’re taking antidepressants, statins, or diabetes meds on top of that? The chances of something going wrong climb even higher.
And here’s the kicker: most of these interactions are preventable. But only 18% of patients who qualify for a full medication review-where a pharmacist or doctor goes through every pill you’re taking-actually get one. That’s not just a gap in care. It’s a gap in safety.
Your Kidneys and Liver Are the Gatekeepers
Think of your liver and kidneys as bouncers at a club. They decide what drugs get in, how long they stay, and when they kick them out. If they’re damaged, the party doesn’t stop-it just gets messy.
Chronic kidney disease cuts your body’s ability to clear drugs by 50-75%. That means a standard dose of a blood pressure pill or painkiller can build up to toxic levels. The American Medical Association says 40% of commonly prescribed medications need dose changes in people with kidney problems. But a 2021 JAMA audit found that in nearly half of cases, doctors don’t adjust the dose-even when the patient’s kidney function is clearly documented.
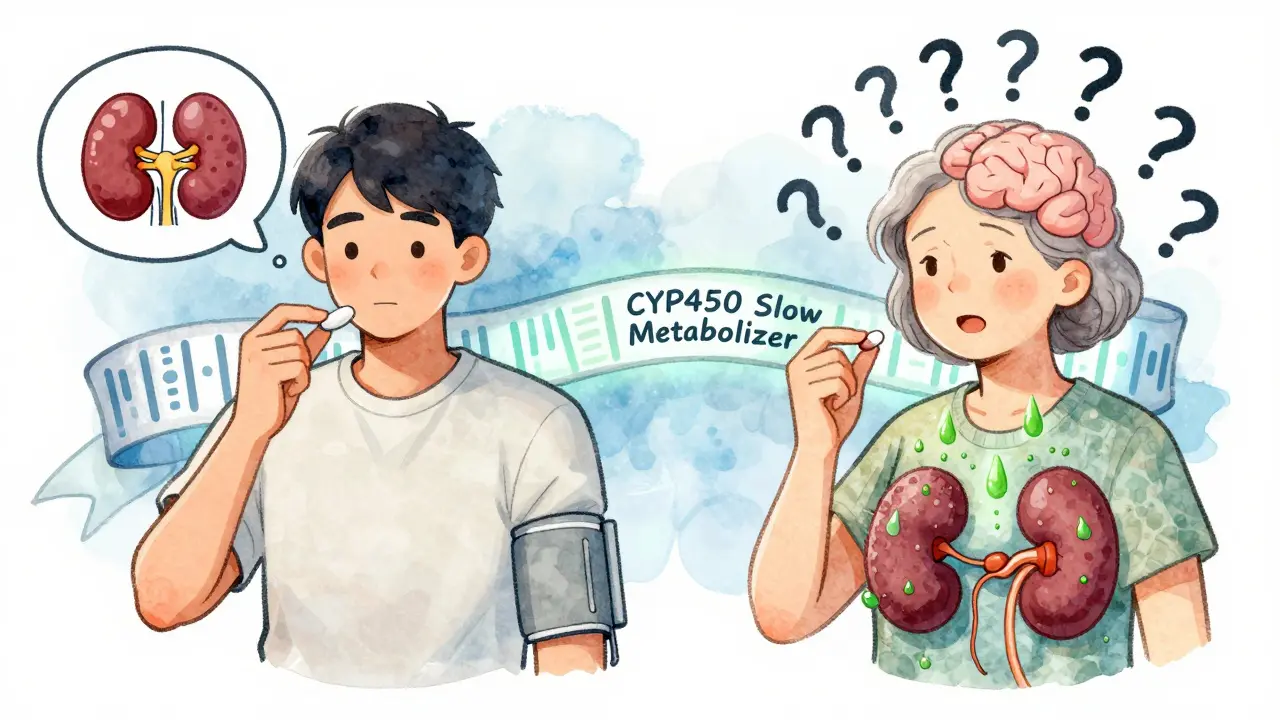
Same goes for your liver. Genetic differences in CYP450 enzymes (the ones that break down meds) can make some people process drugs 30% slower-or 500% faster. That’s why two people taking the same dose of the same drug can have wildly different outcomes. One feels fine. The other ends up in the hospital.
Age Isn’t Just a Number-It’s a Risk Factor
If you’re over 65, your body doesn’t handle drugs the way it used to. Your liver slows down. Your kidneys filter less. Your fat-to-muscle ratio changes. All of that alters how drugs move through you.
Older adults experience 3-5 times more adverse reactions than younger people. And it’s not just about volume. It’s about sensitivity. A dose that’s safe for a 40-year-old might be dangerous for a 75-year-old. Yet, many prescriptions are still written using the same standards for everyone.
And then there’s cognition. If you’ve got memory issues, dementia, or even just trouble remembering to take pills on time, your risk of a medication error jumps dramatically. One 2008 study found impaired cognition carried a 13-times higher odds of a preventable error. That’s not just forgetfulness. That’s a medical emergency waiting to happen.
Gender Isn’t a Bonus Field on a Form-It’s a Biological Variable
Women are more likely to have bad reactions to medications. Not because they’re “sensitive.” But because most drug trials were done on men.
Between 2010 and 2020, only 22% of participants in cardiovascular drug trials were women. That means dosing guidelines were built on male physiology. Women metabolize drugs differently. They have less body water, more body fat, and different hormone levels. The result? Older women experience adverse reactions at least 50% more often than men.
And it’s not just hormones. Women are more likely to be prescribed multiple medications-often for conditions like depression, anxiety, or chronic pain-that overlap in side effects. That’s not because they’re sicker. It’s because their symptoms have historically been misunderstood or under-treated. Now, they’re paying the price with more side effects.

Cost Is a Hidden Medical History
Did you skip a dose because the prescription was too expensive? You’re not alone. One in four patients in the U.S. doesn’t take their meds as prescribed because of cost. But here’s what most people don’t realize: skipping doses isn’t harmless. It’s dangerous.
A 2022 study of over 12,000 Medicare patients found that people who intermittently stop and restart meds have a 28% higher risk of side effects when they start again. Why? Because your body forgets how to handle the drug. When you restart without slowly building back up, your system gets overwhelmed. That’s how a simple blood pressure pill turns into a fall, a hospital stay, or worse.
And when you skip meds, your doctor doesn’t know. They see your blood pressure is high, so they increase the dose. You get more side effects. You skip again. The cycle keeps going. No one’s connecting the dots.
Your History Can Mimic Disease
Medications don’t just cause side effects-they can look like diseases. Beta-blockers can hide a racing heartbeat during internal bleeding. Steroids can mask pain from a ruptured ulcer. Antidepressants can cause tremors that look like Parkinson’s. Diuretics can cause confusion that looks like dementia.
The Merck Manual says this clearly: when a patient develops new symptoms, doctors should always ask: Could this be a drug reaction? Too often, they don’t. A 2023 PatientsLikeMe survey found that 62% of people with multiple chronic conditions had side effects that their doctors initially misdiagnosed as something else. That’s not incompetence. It’s a failure to look at the full picture.
What Can You Do?
You can’t change your past. But you can make sure it’s not working against you.
- Keep a written list of every medication you’ve ever taken-including over-the-counter pills, supplements, and herbal remedies-and note any reaction you had.
- Bring that list to every appointment. Don’t assume your doctor already knows.
- Ask: “Could this new drug interact with anything I’ve taken before?”
- If you’re on five or more meds, ask for a medication review. Pharmacists can spot overlaps and redundancies you might miss.
- Get your kidney and liver function checked regularly if you’re over 60 or have chronic conditions.
- If you can’t afford your meds, tell your doctor. There are often cheaper alternatives, patient assistance programs, or generic versions.
There’s new tech out there too-like genetic testing that checks how your body breaks down drugs. The FDA approved YouScript in 2023, which looks at 27 gene-drug interactions. It can cut side effects by 34% for people with the right genetic profile. But only 5.7% of U.S. clinics use it. Why? Cost. Lack of awareness. Lack of training.
Until that changes, the most powerful tool you have is your own history. Write it down. Share it. Fight for it. Because in the world of medication safety, your past isn’t just information. It’s protection.
What If I Don’t Remember All My Past Medications?
You don’t need to remember every pill you ever took. Start with the last five years. Focus on anything you took for more than a month, especially if you had side effects. Check old pill bottles, pharmacy receipts, or your insurance portal. Many insurers let you download your prescription history. If you’re unsure, ask your pharmacist-they have access to your full record.
Can I Trust My Doctor to Know My History?
Not always. Electronic records are full of gaps. A 2023 Institute for Safe Medication Practices report found that on average, each hospital admission had 3.2 missing or incorrect medication history items. That’s not rare. That’s standard. You are your own best advocate. If something feels off, speak up. If your doctor dismisses your concerns, ask for a second opinion.
Is It Too Late to Change My Medication List?
No. Deprescribing-carefully stopping meds that aren’t helping or are causing harm-is a proven strategy. A 2023 Cochrane Review of 14 trials showed structured medication reviews reduced adverse reactions by 22% in people on multiple drugs. It’s not about cutting everything. It’s about removing what’s unnecessary, risky, or redundant. Talk to your doctor or pharmacist about a review. It’s safer than staying on meds that might be hurting you.
Do Genetic Tests Really Help?
For some people, yes. If you’ve had repeated bad reactions to meds with no clear cause, genetic testing can reveal why. For example, if you’re a slow metabolizer of statins, you’re at higher risk for muscle damage. A simple test can show that. But it’s not for everyone. It’s most useful if you’re on multiple meds, have unexplained side effects, or have a family history of drug reactions. Ask your doctor if it’s right for you.
Why Don’t More Doctors Use This Info?
Time. Training. Technology. Most doctors have 10-15 minutes per patient. Digging through decades of medical history isn’t built into that clock. Many weren’t trained in pharmacogenomics. And systems don’t always alert them when a patient has a red flag. It’s a system problem-not a doctor problem. That’s why your role matters. Bring the data. Ask the questions. Push for the review.








Jamie Allan Brown
February 1, 2026 AT 11:42Been there. Took statins for years, ended up with muscle pain so bad I could barely climb stairs. Doctor brushed it off as 'just aging.' Turns out I'm a slow CYP3A4 metabolizer. Got tested after a near-miss ER trip. Life changed. If you're on more than three meds and feel off, ask for pharmacogenomics. It's not sci-fi-it's science.
Also, never assume your EHR is accurate. My record listed 'penicillin allergy' as 'possible'-until I dug up my 12-year-old hospital discharge papers. Now they flag it like a bomb.
Bring your own list. Always.
Naomi Walsh
February 3, 2026 AT 04:06How is this even a topic anymore? Anyone with half a brain knows polypharmacy is a disaster waiting to happen. The medical-industrial complex thrives on overprescribing. You think your 'doctor' is looking out for you? They're incentivized to write scripts, not audit them. And don't get me started on the FDA-more like 'Fooling Dumb Americans.'
Genetic testing? Only useful if you can afford $1,200 and your insurer doesn't classify it as 'experimental.' Meanwhile, grandma's on 11 drugs because no one bothered to deprescribe. This isn't medicine. It's corporate bingo.
Lu Gao
February 3, 2026 AT 19:06Yessss!! 😍 I literally just had my pharmacist do a med review last week and she caught 3 duplicate prescriptions AND a dangerous interaction between my antidepressant and that OTC sleep aid I thought was 'harmless.' 🤯
Also, if you're over 60 and on more than 5 meds, ASK FOR A REVIEW. It's free through Medicare Part D. Seriously. Do it. Your liver will thank you. 💪💊
Angel Fitzpatrick
February 4, 2026 AT 09:16They don't want you to know this, but every single drug interaction is tracked by a secret AI in the Pentagon that's used to predict which patients will 'fail' and need to be deprioritized in healthcare.
Why? Because Big Pharma and the CDC are working with insurers to reduce 'high-risk' populations. That's why your doctor doesn't adjust doses-even when your labs scream it. They're told not to. The CYP450 enzyme data? It's not just genetic-it's classified. I've seen the redacted memos.
And the 'YouScript' test? It's a placebo. They only use it on people who already have insurance. The rest of us? We're cannon fodder.
Write down your meds. Burn the paper. Don't trust the system. It's rigged.
Chris & Kara Cutler
February 4, 2026 AT 10:02STOP SKIPPING MEDS!! 🚨 I saw my mom do this with her blood pressure pills-'I'll just take it when I feel it.' Then she fell, broke her hip, and spent 6 months in rehab. Don't be her. Get the cheap generics. Use pill organizers. Talk to your doc. Your life is worth more than $5.
Also-YES to the list. I keep mine on my fridge with magnets. My whole family uses it. 🧠❤️
Rachel Liew
February 4, 2026 AT 20:07i just wanted to say thank you for writing this. my grandma passed last year and i think a lot of it was because no one ever looked at her whole med list. she was on 8 things and no one ever asked if she could afford them or if they were even helping.
i started keeping a notebook now for my mom. we write down every pill, even the ones from the gas station. it feels small, but it feels right.
you’re not alone in this. 💙
Lisa Rodriguez
February 4, 2026 AT 21:34As a pharmacist, I see this every single day. Patients come in with 12 meds, no idea what half of them are for, and their doctor hasn't reviewed it in 3 years.
Here’s the truth: most of those meds aren’t actually needed anymore. Deprescribing isn’t dangerous-it’s safer than staying on them. We’ve had patients come off 4 drugs and feel better than they have in a decade.
And yes, your kidney/liver numbers matter. If your eGFR is under 60, your painkillers need adjusting. Period. If your doctor doesn’t know that, find a new one.
Bring your list. Ask the questions. You’re not being annoying-you’re saving your life.
Lilliana Lowe
February 6, 2026 AT 06:06While the sentiment is laudable, the article exhibits a concerning conflation of correlation with causation-particularly regarding gender-based pharmacokinetics. The 50% higher adverse reaction rate among women is not inherently biological; it is a statistical artifact of underpowered trials and non-standardized dosing protocols. The solution is not to pathologize female physiology but to demand gender-balanced clinical trial design with pharmacokinetic stratification. Also, the mention of YouScript is misleading-it is not FDA 'approved' for clinical use, merely cleared under 510(k) as a decision-support tool. Precision medicine is not a magic bullet; it is a framework requiring systemic reform, not anecdotal empowerment.
Melissa Melville
February 6, 2026 AT 11:41So let me get this straight… we’re supposed to trust a system that gave us Vioxx, thalidomide, and now opioid epidemics… but we’re supposed to just ‘bring a list’ and it’ll be fixed? 😂
My aunt took a drug that made her hallucinate for 3 weeks. Doctor said ‘it’s just stress.’ Turns out it was a drug interaction she’d had before… in 2008. Her record said ‘allergic to penicillin’ but not ‘had psychotic episode with amoxicillin.’
Yeah. We’re all just supposed to be superheroes now. Good luck with that. 🙃