When you pick up a generic pill from the pharmacy, you expect it to work just like the brand-name version. But what happens when that pill sits on a shelf for months-or years? Not all generics are created equal when it comes to stability and shelf life. While the active ingredient might be the same, small differences in how it’s made, packaged, or stored can lead to real safety risks. Many people assume expiration dates are just bureaucratic footnotes. They’re not. They’re the line between a medicine that works and one that could harm you.
What Does Stability Even Mean?
Stability isn’t just about whether a pill still looks the same. It’s about whether it still does what it’s supposed to do. The FDA defines it clearly: a product must keep its chemical strength, physical form, and safety profile throughout its shelf life. That means no loss of potency, no toxic breakdown products, no clumping, no mold, and no change in how it’s absorbed by your body. For a tablet, that might mean it doesn’t crumble. For a liquid antibiotic, it means the active ingredient doesn’t break down into something dangerous. For an inhaler, it means each puff delivers the exact same dose. These aren’t theoretical concerns. In 2020, the FDA found that 17.3% of generic levothyroxine products-used to treat thyroid conditions-had stability issues not seen in the brand-name version, Synthroid. The culprit? Poor moisture protection during manufacturing. That’s not a small difference. For someone relying on that drug to regulate their metabolism, even a 5% drop in potency can cause fatigue, weight gain, or heart problems.How Do They Test This Stuff?
Pharmaceutical companies don’t just guess how long a drug lasts. They run tests-lots of them. The global standard is set by the International Council for Harmonisation (ICH), especially guideline Q1A(R2). These tests follow strict rules:- Chemical stability: Measured using HPLC to track how much of the active ingredient breaks down over time. If more than 0.1% of unknown impurities form, the product fails.
- Physical stability: Does the tablet still dissolve properly? Does a liquid stay clear? For nanoparticle drugs like those used in cystic fibrosis treatments, particles must stay under 200 nanometers. If they clump up, they can’t reach the lungs.
- Microbiological stability: No mold, no bacteria. Non-sterile products must have fewer than 100 colony-forming units per gram. Sterile ones? They must be virtually germ-free, with a safety level of 1 in 1 million chances of contamination.
- Functional stability: For inhalers, injectables, or patches, the delivery system must still work. A metered-dose inhaler must deliver 90-110% of the labeled dose every time.
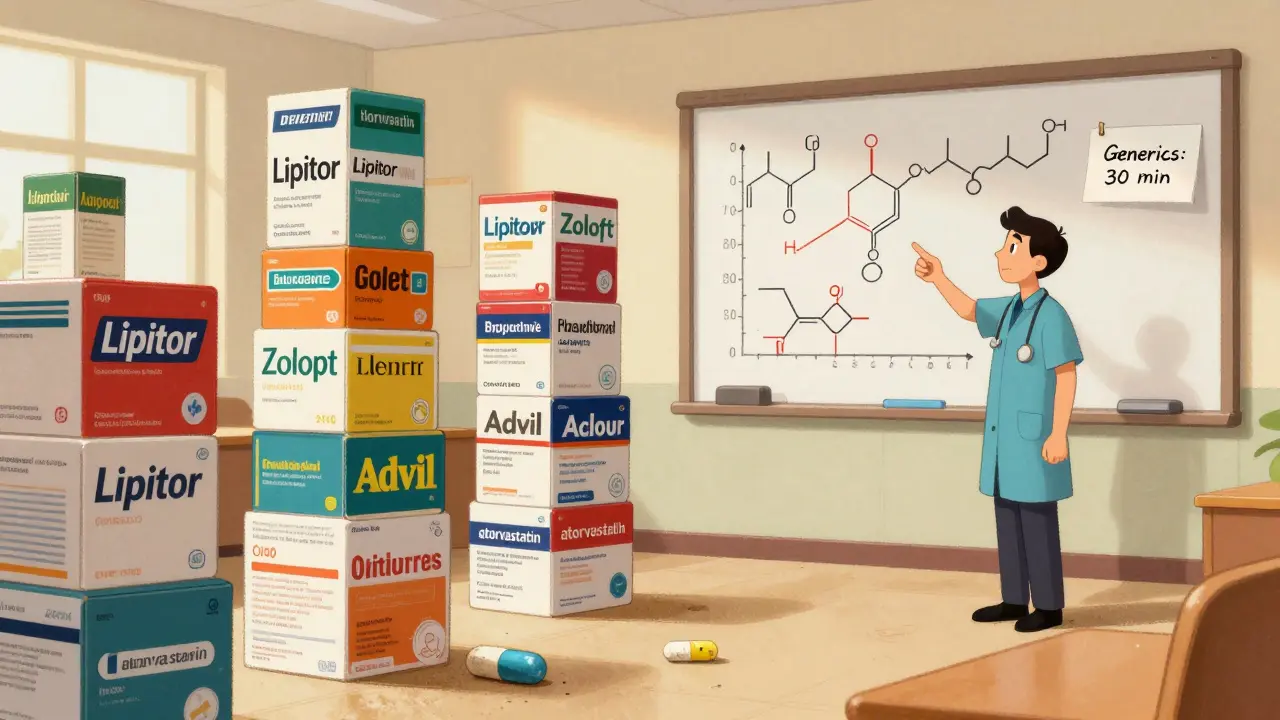
Why Do Generics Often Fail?
Brand-name drugs go through years of clinical trials and stability testing before approval. Generics? They’re required to prove bioequivalence-meaning they work the same way in the body. But they’re not required to repeat the full stability studies. That’s where things get risky. Generics use different excipients-fillers, binders, coatings-that aren’t always as stable. One company might use a cheaper moisture-absorbing agent that doesn’t protect as well. Another might use a different drying process that leaves microscopic cracks in the tablet. These aren’t visible. They don’t show up in bioequivalence tests. But over time, they let in air, moisture, or light-and that’s when degradation begins. A 2022 study by the Parenteral Drug Association found that 62.7% of stability professionals had experienced a product recall in the past five years. The top reason? Microbial growth in preservative systems. Why? Water activity changed. A tiny shift in humidity during storage, or a packaging flaw, and suddenly bacteria grow. That’s not just a quality issue. It’s a patient safety issue.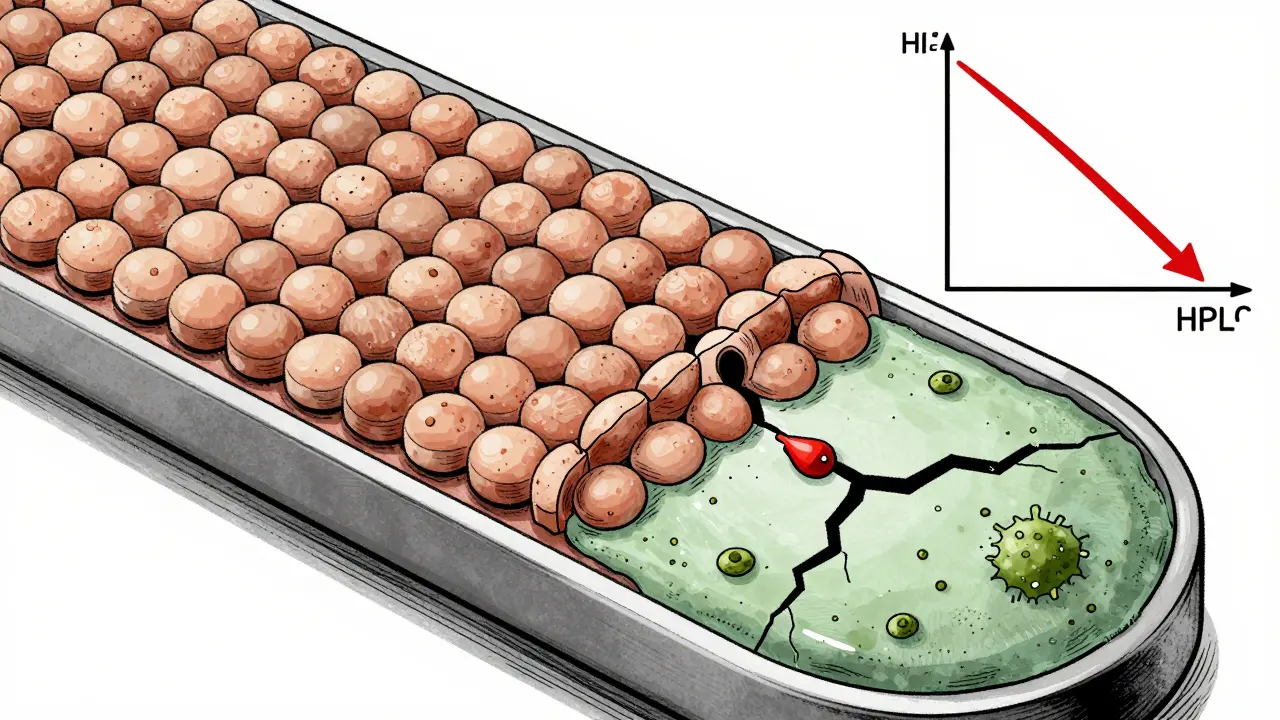
Storage Isn’t Optional-It’s Law
Even the most stable drug will fail if stored wrong. The FDA mandates exact storage conditions on labels: “Store at 15-30°C.” Not “room temperature.” Not “keep in a cool place.” Those vague terms get companies cited during inspections. In fact, 80% of FDA Form 483 observations in stability programs are about poor documentation. Think about it: if your medicine is supposed to be kept at 25°C, but your bathroom cabinet hits 32°C in summer, you’re accelerating degradation. That’s why some people report their generic blood pressure meds “don’t work anymore”-they’ve been sitting above the safe range for months. In low-income countries, the problem is worse. The WHO found that 28.7% of medicines fail stability tests because of poor supply chains-no refrigeration, no climate-controlled warehouses. In high-income countries? Only 1.2% fail. That’s not a difference in quality control. It’s a difference in infrastructure.What’s Changing in 2026?
The rules are slowly catching up to science. The ICH Q12 guideline, effective since late 2023, lets companies make changes to their manufacturing process after approval-without restarting full stability studies-if they can prove stability isn’t affected. That’s a big shift toward flexibility. The FDA is also testing Continuous Manufacturing Stability Testing (CMST), which can cut shelf-life determination time by 40%. Instead of waiting for batch after batch to age, they monitor real-time data from production lines. This isn’t sci-fi-it’s already working in pilot programs. But the biggest shift? Predictive modeling. Companies like Amgen and Merck are using risk-based tools to predict degradation patterns using AI and machine learning. In trials, they cut shelf-life determination time by 30%. The problem? Regulators still don’t fully accept these methods. Until they do, most companies stick to the slow, expensive, traditional way.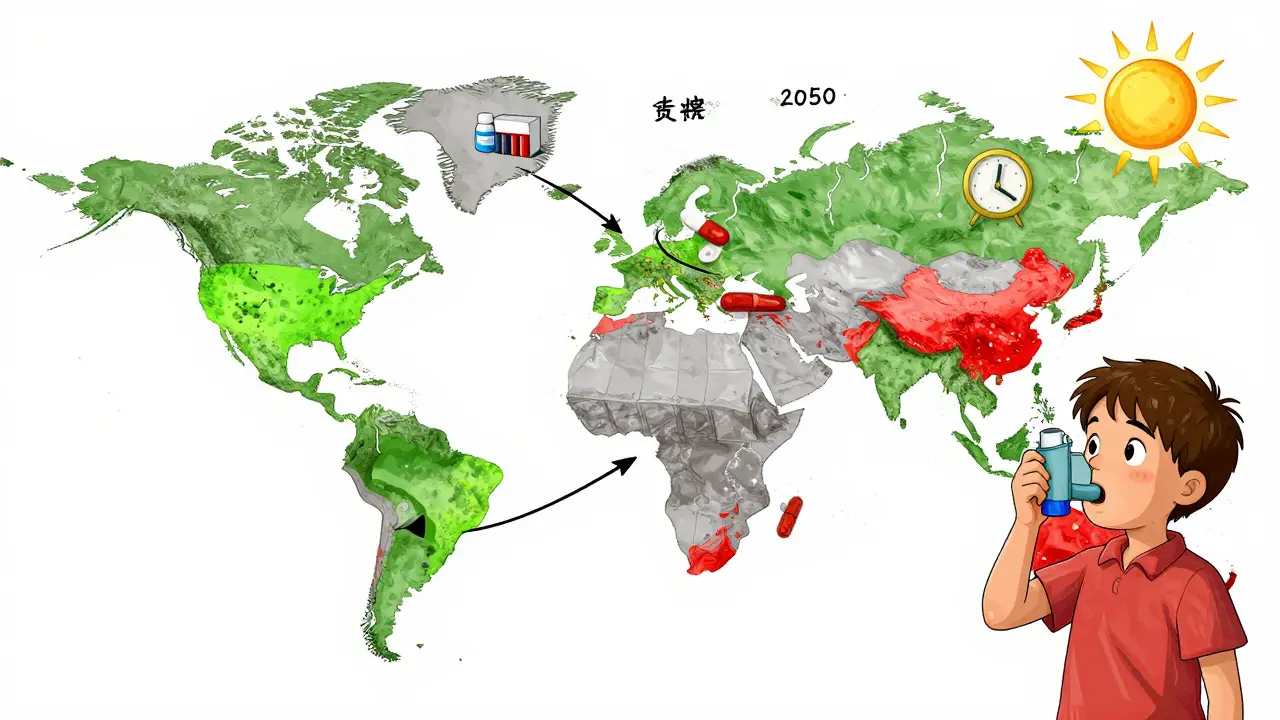
What Should You Do?
As a patient, you can’t test your meds. But you can protect yourself:- Check the expiration date. Don’t use pills past that date-even if they look fine.
- Store them right. Keep them in a cool, dry place. Not the bathroom. Not the car. A bedroom drawer is better.
- Watch for changes. If a tablet changes color, smells odd, or crumbles easily, don’t take it. Return it.
- Ask your pharmacist. If you’re switching from brand to generic, ask if there are known stability issues with that batch.
What’s at Stake?
This isn’t just about money. It’s about trust. When a drug fails, it’s not just a financial loss. It’s a broken promise. A child with asthma gets a weaker inhaler. An elderly person’s blood pressure spikes because their pill lost potency. A patient develops an infection from a contaminated liquid antibiotic. The global stability testing market is worth over $2.8 billion-and growing. That’s because the stakes are higher than ever. Climate change is making storage harder. By 2050, rising temperatures could shorten average drug shelf life by nearly 5 months. That’s not a future problem. It’s already happening in warehouses that aren’t climate-controlled. The science exists. The standards exist. What’s missing is consistent enforcement-and public awareness. Generics save billions. But they’re only safe if they stay stable. And that’s not automatic. It’s engineered. It’s tested. It’s monitored. And if any part of that chain breaks, the medicine doesn’t just stop working. It becomes a risk.Can expired generic drugs still be safe to use?
It’s not recommended. While some drugs may retain potency past their expiration date, there’s no guarantee. Stability testing is done up to the labeled date only. After that, degradation can accelerate unpredictably. For critical medications like insulin, heart drugs, or antibiotics, using expired generics can be dangerous. Even if it looks fine, chemical breakdown or microbial growth may have occurred.
Why do some generic drugs have shorter shelf lives than brand-name versions?
It’s usually because of differences in excipients, packaging, or manufacturing processes. Brand-name companies invest heavily in optimizing stability over years. Generic manufacturers focus on proving bioequivalence, not long-term durability. A cheaper coating, a less effective desiccant, or a different drying method can reduce shelf life-even if the active ingredient is identical.
How do I know if my generic drug has stability issues?
You won’t always know until something goes wrong. But signs include visible changes: discoloration, crumbling, odd smells, or clumping in liquids. If you notice these, stop using the medication and contact your pharmacist. You can also check FDA Drug Safety Communications for recalls related to specific generic drugs. If your medication suddenly doesn’t seem to work as well, stability could be the cause.
Is accelerated stability testing reliable for predicting real-world shelf life?
It’s useful, but not foolproof. Accelerated tests use high heat and humidity to speed up degradation. But some degradation pathways only happen at normal temperatures. For example, polymorphic transitions-where a drug’s crystal structure changes-can be missed in accelerated tests. That’s why long-term studies are still required. Regulatory agencies allow limited extrapolation, but only if long-term data shows minimal change.
Are there any regulations requiring generic drug manufacturers to test for stability?
Yes. Both the FDA and EMA require stability data for all approved drugs, including generics. The FDA’s 21 CFR 211.166 and EMA’s 2001/83/EC directive mandate scientifically valid studies. However, the scope of testing can be reduced if the generic is similar to a previously approved product. This flexibility increases risk if the differences in formulation aren’t fully understood.
Can climate change affect the shelf life of medications?
Absolutely. A 2022 MIT study projected that by 2050, rising global temperatures could reduce average drug shelf life by 4.7 months due to more frequent warehouse temperatures exceeding 30°C. This is already happening in parts of the U.S., Australia, and Southeast Asia. Medications stored in non-climate-controlled distribution centers are at higher risk of degradation, especially in low-income regions where refrigeration is unreliable.







Sonal Guha
January 12, 2026 AT 00:37TiM Vince
January 12, 2026 AT 22:14gary ysturiz
January 13, 2026 AT 14:40Jessica Bnouzalim
January 14, 2026 AT 19:57Bryan Wolfe
January 15, 2026 AT 00:09Sumit Sharma
January 15, 2026 AT 21:00Lawrence Jung
January 17, 2026 AT 14:29Christina Widodo
January 18, 2026 AT 11:33Prachi Chauhan
January 18, 2026 AT 21:54Katherine Carlock
January 19, 2026 AT 02:09Sona Chandra
January 20, 2026 AT 07:54Jennifer Phelps
January 21, 2026 AT 16:28beth cordell
January 23, 2026 AT 09:15Lauren Warner
January 23, 2026 AT 23:20gary ysturiz
January 25, 2026 AT 05:38