MAOI-Opioid Safety Checker
Check Your Medication Combination
This tool checks if your MAOI and opioid combination is safe based on FDA guidelines and clinical evidence.
Combining opioids with MAOIs isn’t just risky-it’s potentially fatal. This isn’t a theoretical warning. It’s a documented cause of death, with over 120 confirmed cases of serotonin syndrome linked to this mix since 2010, and nearly 90 people dying from it in the U.S. alone between 2015 and 2022. If you’re taking an MAOI for depression and your doctor suggests an opioid for pain, stop. Don’t take it. Ask again. Because this interaction doesn’t just cause side effects-it can shut down your nervous system in hours.
What Are MAOIs and Why Do They Clash with Opioids?
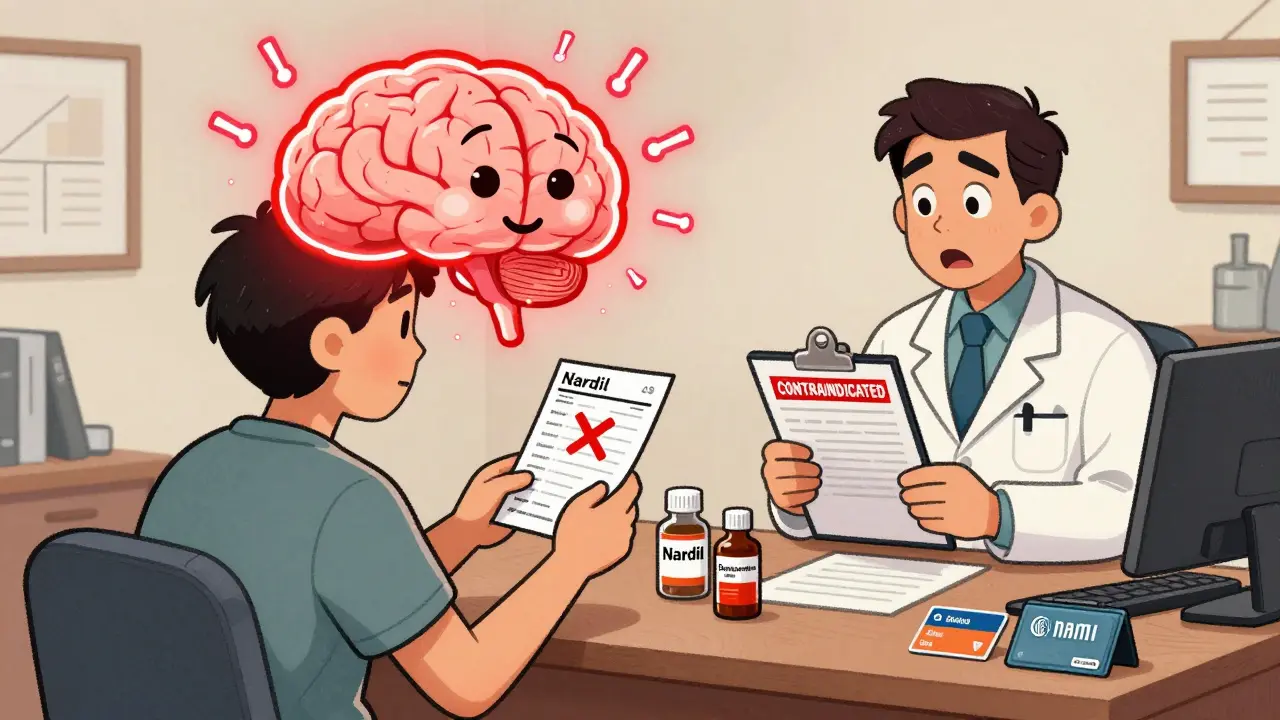
MAOIs-monoamine oxidase inhibitors-are older antidepressants like phenelzine (Nardil), tranylcypromine (Parnate), and isocarboxazid (Marplan). They work by blocking the enzyme that breaks down serotonin, norepinephrine, and dopamine. That’s why they help with depression: more of these mood-lifting chemicals stay active in your brain.
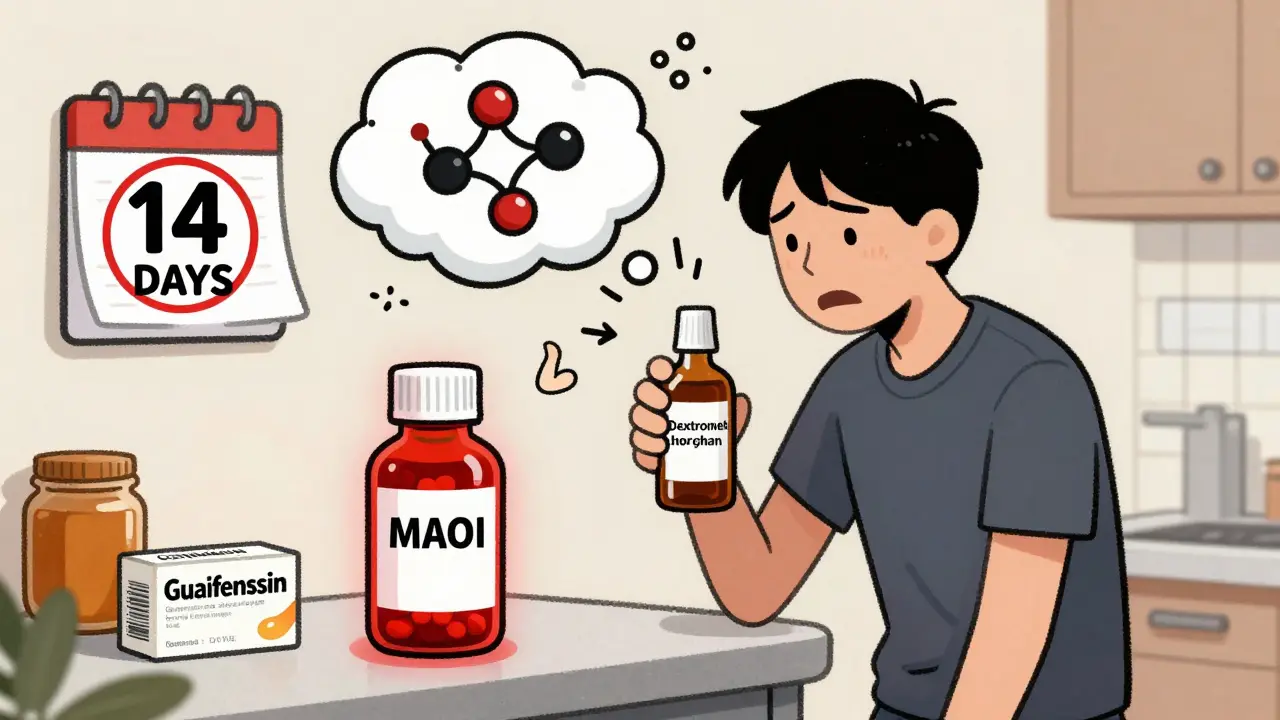
But here’s the problem: some opioids do the same thing-only they push it over the edge. Tramadol, meperidine, methadone, and even dextromethorphan (found in cough syrup) increase serotonin levels by either releasing it or stopping its reuptake. When you combine them with an MAOI, your brain gets flooded. Serotonin doesn’t just rise-it explodes. That’s serotonin syndrome.
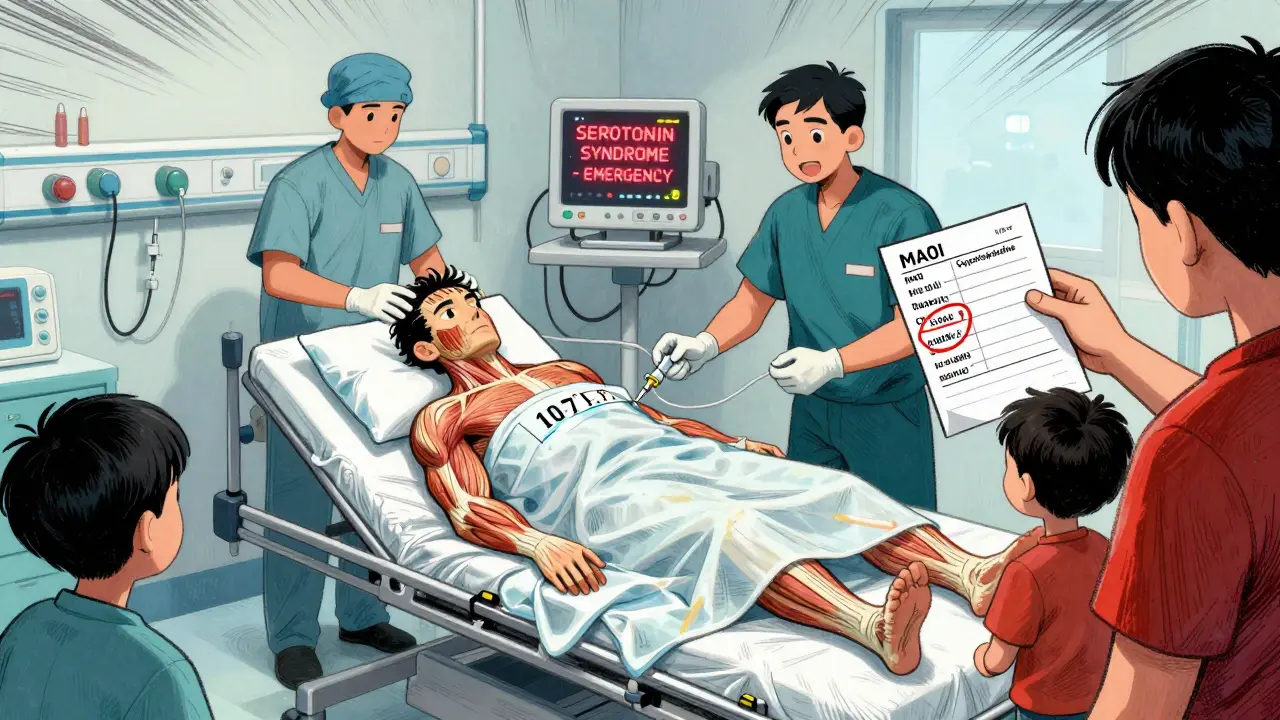
Think of it like two people pouring gasoline on the same fire. One is the MAOI, blocking the drain. The other is the opioid, turning on the tap. The result? Overheating, muscle rigidity, seizures, high blood pressure, and sometimes death.
The Opioids That Are Most Dangerous
Not all opioids are equally risky. Some are outright banned with MAOIs. Others are dangerous enough that doctors avoid them like landmines.
- Meperidine (Demerol): The worst offender. Over 37 deaths were directly linked to this combo between 1960 and 2010. It’s so dangerous the FDA and American Psychiatric Association call it absolutely contraindicated.
- Tramadol: Often mistaken as "safe" because it’s not classified as a narcotic. But it’s responsible for over half of all serotonin syndrome cases linked to MAOIs. A Reddit user on r/antidepressants described being hospitalized for 72 hours after taking tramadol for a toothache while on phenelzine-body temperature hit 107.1°F.
- Methadone: Used for pain and addiction treatment. It has multiple mechanisms that increase serotonin and can trigger life-threatening reactions even at standard doses.
- Tapentadol (Nucynta): Another sneaky one. Purdue Pharma was sued in 2021 for not clearly warning about this interaction.
- Morphine, oxycodone, hydromorphone: Lower risk-but still risky. They don’t directly release serotonin, but they can still push the system over the edge, especially in sensitive individuals.
Even "mild" opioids like codeine or hydrocodone aren’t completely safe. The risk isn’t always obvious, and your doctor might not know the full picture.
What Happens When You Mix Them?
Serotonin syndrome doesn’t sneak up. It hits fast. Symptoms usually appear within 1 to 2 hours after taking the opioid, and can escalate to death in under 12 hours.
Signs to watch for:
- High body temperature (over 104°F)
- Muscle rigidity-so tight you can’t move or breathe
- Shivering or tremors
- Confusion, agitation, hallucinations
- Rapid heart rate, high blood pressure
- Sweating, dilated pupils
- Seizures
One anesthesiologist in a medical forum recalled two near-fatal cases: one patient on Parnate given Demerol after surgery spiked to 240/140 blood pressure and needed a 12-hour drip to control it. Another, on Nardil, developed full serotonin syndrome after a dental procedure and required cooling blankets and a drug called cyproheptadine to survive.
These aren’t rare outliers. The FDA’s adverse event database has over 400 reports of this interaction since 2015. And 20.8% of those cases ended in death.
How Long Should You Wait After Stopping an MAOI?
If you’re switching from an MAOI to an opioid, you can’t just stop one and start the other the next day. MAOIs permanently disable enzymes. Your body needs time to grow new ones.
For irreversible MAOIs like Nardil or Parnate: wait at least 14 days after your last dose before starting any opioid with serotonergic activity. This isn’t a suggestion-it’s a medical requirement. The FDA’s labeling for selegiline patches confirms this timeline.
For reversible MAOIs like moclobemide (Aurorix): a 24-hour washout is usually enough. But even then, caution is advised. There are still case reports of serotonin syndrome with moclobemide and tramadol.
And if you’re going the other way-stopping an opioid to start an MAOI? Wait 7 to 10 days after your last opioid dose. Some opioids linger in your system longer than you think.
What Pain Relief Is Safe If You’re on an MAOI?
You don’t have to suffer. There are safe alternatives.
- Buprenorphine: At low doses (0.2-0.4 mg sublingual), it’s been used safely in over 140 MAOI-treated patients without a single case of serotonin syndrome.
- Acetaminophen (Tylenol): No interaction. First-line for mild to moderate pain.
- NSAIDs: Ibuprofen, naproxen-safe as long as you don’t have kidney or stomach issues.
- Physical therapy, nerve blocks, acupuncture: Non-drug options that work well for chronic pain.
What’s NOT safe? Avoid tramadol, tapentadol, methadone, meperidine, dextromethorphan, and any opioid you’re unsure about. Even if your pharmacist says "it’s fine," double-check with your psychiatrist or a specialist in psychopharmacology.
Why Do These Mistakes Keep Happening?
You’d think this would be common knowledge by now. But it’s not.
A 2022 study in JAMA Internal Medicine found that 4.3% of people on MAOIs were still prescribed contraindicated opioids within 14 days of starting the drug. That’s over 11,000 dangerous prescriptions every year in the U.S. alone.
Why? Because:
- Primary care doctors often don’t know the patient is on an MAOI.
- Patients don’t tell them-because they think "it’s just an antidepressant."
- Tramadol is still marketed as "non-narcotic," leading doctors to underestimate its danger.
- Emergency rooms don’t always ask about psychiatric meds when someone comes in with high fever and muscle stiffness.
Even worse: a 2022 study in the Annals of Emergency Medicine found that 31% of ER doctors didn’t know tramadol is contraindicated with MAOIs.
What’s Being Done to Stop This?
Technology is helping. Electronic health records now have hard stops. Epic Systems blocked over 8,400 dangerous prescriptions in 2021. But 1,207 of them were overridden-because someone clicked past the warning.
The FDA updated MAOI medication guides in January 2023, listing 12 contraindicated opioids by name. The European Medicines Agency now requires mandatory training for prescribers in the EU.
A new digital tool called SerotoninSafe, approved by the FDA in 2023, integrates with hospital systems to give real-time alerts. In a pilot at Johns Hopkins, it cut prescribing errors by 76%.
But the biggest protection is still you.
What You Need to Do Right Now
If you’re on an MAOI:
- Make a list of every medication you take-including over-the-counter cough syrups and supplements.
- Check if any contain tramadol, methadone, dextromethorphan, or tapentadol.
- Carry a wallet card from NAMI (National Alliance on Mental Illness) listing your contraindicated drugs. 78% of users who carry one say it’s saved them from a dangerous mix.
- Tell every doctor, dentist, and pharmacist you see-even for a minor procedure.
- If you’re scheduled for surgery, bring your MAOI prescription bottle and tell the anesthesiologist.
If you’re prescribed an opioid while on an MAOI:
- Ask: "Is this safe with MAOIs?"
- Ask: "What’s the risk of serotonin syndrome?"
- Ask: "Can we use acetaminophen or buprenorphine instead?"
- If they say "it’s fine," get a second opinion.
This isn’t about being paranoid. It’s about survival. People have died because someone assumed a painkiller was "harmless." Don’t let that be you.
What to Do in an Emergency
If you or someone you know shows signs of serotonin syndrome after mixing an opioid and MAOI:
- Call 911 immediately.
- Do not wait to see if it gets better.
- Tell emergency responders: "I’m on an MAOI and took an opioid. I think I have serotonin syndrome."
- Keep the person cool. Remove excess clothing.
- Do not give any more medication unless instructed by medical personnel.
Hospitals like Massachusetts General have protocols ready: cyproheptadine (12mg), benzodiazepines for seizures, and aggressive cooling. Time is critical.
Can I take tramadol if I’m on an MAOI?
No. Tramadol is one of the most dangerous opioids to combine with MAOIs. It’s responsible for over half of all serotonin syndrome cases linked to this interaction. Even low doses can trigger a life-threatening reaction within hours. Never take tramadol while on an MAOI, even if your doctor says it’s "safe."
How long after stopping an MAOI can I safely take an opioid?
For irreversible MAOIs like Nardil or Parnate, you must wait at least 14 days after your last dose. For reversible MAOIs like moclobemide, a 24-hour wait is usually sufficient-but only under medical supervision. Never assume the drug is "out of your system" just because you feel fine.
Is buprenorphine safe with MAOIs?
Yes, at low doses (0.2-0.4 mg sublingual), buprenorphine has been safely used in over 140 patients on MAOIs without triggering serotonin syndrome. It’s now the preferred opioid for pain relief in this group. But always start low and monitor closely under medical supervision.
What if I accidentally took an opioid while on an MAOI?
If you’ve taken even one dose of tramadol, meperidine, methadone, or dextromethorphan while on an MAOI, seek emergency medical help immediately. Do not wait for symptoms. Serotonin syndrome can progress from mild discomfort to death in under 12 hours. Call 911 or go to the nearest ER and say exactly what you took and when.
Are newer MAOIs safer with opioids?
The transdermal selegiline patch has lower brain penetration, so it carries less risk than oral MAOIs-but it’s still not risk-free. No MAOI is completely safe with serotonergic opioids. The FDA and American Psychiatric Association still warn against combining any MAOI with meperidine, tramadol, methadone, or dextromethorphan-even patches.
Can I use over-the-counter cough medicine with an MAOI?
Many cough syrups contain dextromethorphan, which is just as dangerous as tramadol when combined with MAOIs. Always check the label. Safe alternatives include guaifenesin-only products or honey-based remedies. Never assume "over-the-counter" means "safe."
Final Takeaway
This isn’t a "maybe dangerous" situation. It’s a known killer. The science is clear. The deaths are documented. The warnings are in black box labels and FDA guidelines. Yet people still die because someone didn’t ask the right question.
If you’re on an MAOI, treat every opioid as a potential threat until proven otherwise. Keep your medication list updated. Educate your providers. Carry your warning card. And if something doesn’t feel right-trust your gut. Your life depends on it.