Beers Criteria Medication Risk Checker
Check Your Medications for Age-Related Risks
The Beers Criteria lists 56 medications that pose unacceptable risks for people over 65. This tool checks if your medications are on the list.
Based on the 2023 American Geriatrics Society guidelines. Always consult your doctor before stopping any medication.
Risk Assessment
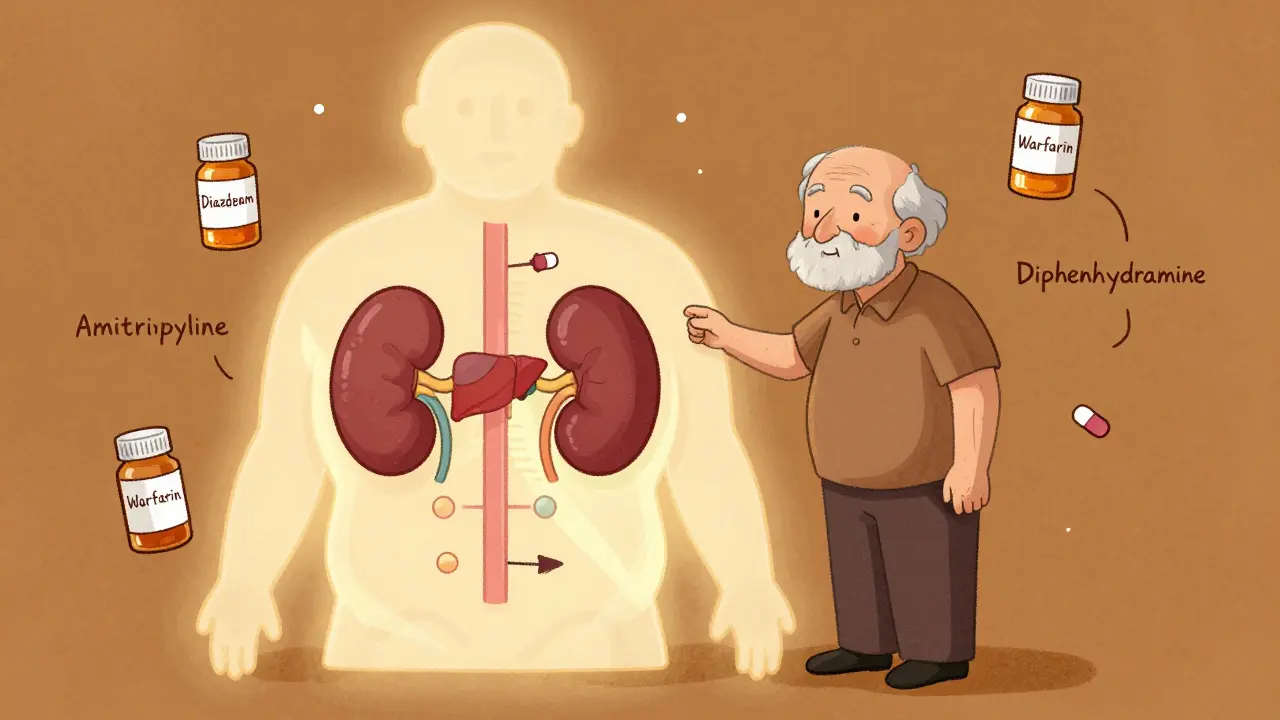
As people age, their bodies change in ways that make medications behave differently - and often more dangerously. What was a safe dose at 40 might cause confusion, falls, or hospitalization at 75. This isn’t about being frail or weak. It’s about biology. Your liver processes drugs slower. Your kidneys filter them less efficiently. Your brain becomes more sensitive to sedatives. These aren’t minor tweaks. They’re major shifts that turn common prescriptions into hidden risks.
Why Older Adults React Differently to Medications
By age 65, the human body starts losing key functions that keep medications in check. Total body water drops by about 15% between ages 25 and 80, while body fat increases significantly. This changes how drugs spread through the body. Water-soluble drugs like lithium or digoxin become more concentrated, raising the risk of toxicity. Fat-soluble drugs like diazepam or amitriptyline linger longer in fatty tissues, leading to prolonged effects - sometimes for days after the last dose. Kidney function declines too. After age 40, glomerular filtration rate (GFR) drops by roughly 0.8 mL/min/1.73m² every year. That means drugs cleared by the kidneys - like antibiotics, blood pressure meds, and painkillers - stick around longer. A standard dose of a drug like ciprofloxacin or metformin can build up to dangerous levels in an older adult, even if they take it exactly as prescribed. The liver also slows down. Blood flow to the liver decreases by 20-40% between ages 25 and 65. That reduces the body’s ability to break down drugs like propranolol, verapamil, and warfarin. Lower liver activity means higher drug levels in the bloodstream. It’s not just about slower metabolism - it’s about drugs staying active longer than intended. Then there’s the brain. Older adults are far more sensitive to central nervous system depressants. A dose of diazepam that causes mild drowsiness in a 30-year-old can trigger severe confusion, memory loss, or even delirium in someone over 75. At the same plasma concentration, older adults experience 50% more sedation and cognitive impairment. That’s not a side effect - it’s a direct result of aging brain chemistry.Common Medications That Become Riskier with Age
Some drugs are simply not safe for older adults - even at low doses. The Beers Criteria, updated in 2023 by the American Geriatrics Society, lists 56 medications that pose unacceptable risks for people over 65. Here are a few that stand out:- Diphenhydramine (Benadryl): An anticholinergic that causes confusion, urinary retention, and constipation. A 2023 University of Florida study found it causes delirium 4.2 times more often in patients over 75 than in younger adults.
- Benzodiazepines (Valium, Xanax, zolpidem): These sleep and anxiety meds increase fall risk by 2-3 times. Zolpidem causes next-day impairment in 80% of people over 65.
- NSAIDs (ibuprofen, naproxen): Even short-term use raises the risk of stomach bleeding and kidney damage. Older adults are 5 times more likely to have a GI bleed from NSAIDs than younger people.
- Warfarin: Blood thinners like this require 20-30% lower doses in older adults. Yet, 35% of seniors on warfarin experience unstable INR levels - compared to just 15% of younger patients.
- Amitriptyline: This antidepressant causes urinary retention in men with enlarged prostates 3-4 times more often than newer alternatives.
These aren’t rare cases. In fact, a 2019 study by Dr. Dima Qato found that 42% of older adults were taking at least one medication on the Beers Criteria list. And 15% of them suffered an adverse event directly tied to it.
Polypharmacy: When More Meds Mean More Danger
Nearly half of adults over 65 take five or more prescription drugs every month. That’s called polypharmacy. And it’s not just about the number of pills - it’s about interactions. Each additional medication increases the chance of a harmful drug interaction by 10-15%. A person taking blood pressure pills, a statin, an antidepressant, a painkiller, and a sleep aid might not realize that the combination is causing dizziness, confusion, or low blood pressure. One study showed that 68% of older adults reported dizziness or falls linked to their medications. Another found that 54% experienced memory problems or confusion. Many assume these are normal signs of aging - but they’re often drug-induced. Take the case of an 82-year-old woman prescribed the same blood pressure dose her doctor uses for 50-year-olds. Within weeks, she developed orthostatic hypotension - a sudden drop in blood pressure when standing. She fell, fractured her hip, and spent months in rehab. Her doctor didn’t adjust the dose because he wasn’t trained to think about age-related changes in pharmacokinetics.
What Doctors Should Do - And Often Don’t
The standard advice - “start low and go slow” - still holds. But too many providers still prescribe adult doses to older patients. The CDC estimates that 50-60% of medication-related hospitalizations in seniors are preventable. That’s not just a medical failure - it’s a systemic one. Experts recommend three key actions:- Review every medication every 3-6 months. Ask: Is this still needed? What’s the benefit? What’s the risk?
- Use the STOPP/START criteria. STOPP identifies inappropriate prescriptions. START identifies medications that should be added - like bone density drugs or vaccines - that are often missed.
- Do a Brown Bag Review. Have patients bring all their pills - prescription, OTC, and supplements - to their appointment. One study found an average of 3.2 medication errors per patient during these reviews.
Pharmacists play a critical role here. When they’re involved in care teams, medication errors drop by 31%. Yet, many older adults still see doctors who don’t consult pharmacists or use tools like the Beers Criteria app - downloaded over 125,000 times since 2020.
Real Stories, Real Consequences
Patient experiences tell the true story behind the statistics. One Reddit user, ‘ElderlyPatient92’, wrote: “After starting amitriptyline for nerve pain at age 78, I developed severe urinary retention requiring catheterization within 3 days.” That’s not an accident. That’s a known risk - and a preventable one. A caregiver on AgingCare.com shared: “My 82-year-old mother’s blood pressure medication caused such severe orthostatic hypotension that she fell and fractured her hip - her doctor had prescribed the same dose he uses for 50-year-olds.” A 2022 survey of 1,200 older adults found that 45% stopped taking at least one medication because of side effects. The top reasons? Constipation (28%), dizziness (24%), and confusion (19%). These aren’t minor inconveniences. They’re life-altering events that lead to falls, hospitalizations, and loss of independence.
What You Can Do
If you or a loved one is over 65 and taking multiple medications, here’s what to do:- Ask your doctor: “Is this drug still necessary? Could it be causing my symptoms?”
- Request a medication review every six months - even if you feel fine.
- Bring all your pills to every appointment - including vitamins, supplements, and over-the-counter drugs.
- Ask if a lower dose is possible, especially for drugs cleared by the kidneys or liver.
- Learn about the Beers Criteria. You can find the full list on the American Geriatrics Society website.
- If you’re experiencing dizziness, confusion, constipation, or falls, don’t assume it’s just aging. Ask: Could this be a drug reaction?
Deprescribing - the careful, planned reduction or stopping of medications - isn’t about cutting corners. It’s about restoring safety. Studies show that 30-50% of medications in nursing homes are unnecessary. Removing them improves cognition, reduces falls, and even extends life.
The Future Is Personalized
New tools are emerging to make geriatric prescribing smarter. Pharmacogenomic testing - which checks how your genes affect drug metabolism - is now being used in clinics. One 2023 study found that testing for CYP2D6 and CYP2C19 genes reduced adverse drug reactions by 35% in older adults on antidepressants. AI systems like MedAware, approved by the FDA, flag dangerous interactions in real time and have cut medication errors by 42% in hospital settings. The FDA now encourages including more seniors in clinical trials - a goal of 25% representation by 2026. Until then, we’re prescribing based on data from people half their age.The bottom line: Aging isn’t just about gray hair and wrinkles. It’s about changes in how your body handles medicine. What works for a 40-year-old might harm a 75-year-old. The solution isn’t more pills. It’s smarter prescribing - and the courage to stop what no longer helps.
Why do older adults have more side effects from medications?
Older adults have more side effects because their bodies change with age. Kidneys and liver process drugs more slowly, body fat increases and water decreases, and the brain becomes more sensitive to certain drugs. These changes mean medications stay in the system longer, reach higher concentrations, and affect the body more intensely - even at standard doses.
What is the Beers Criteria?
The Beers Criteria is a list of medications that are potentially inappropriate for older adults due to high risks of side effects. Updated every two years by the American Geriatrics Society, it identifies 56 drugs that should be avoided or used with extreme caution in people over 65. It’s used by doctors, pharmacists, and caregivers to reduce harmful prescribing.
Can stopping a medication cause problems?
Yes - but only if done suddenly or without planning. Some medications, like blood pressure or antidepressant drugs, must be tapered slowly. The key is deprescribing: a structured, step-by-step process guided by a doctor. Stopping unnecessary drugs often improves health, reduces side effects, and lowers the risk of falls and confusion.
How do I know if a medication is causing my symptoms?
Look for timing. Did symptoms start after beginning a new drug or changing a dose? Common signs include dizziness, confusion, constipation, urinary problems, fatigue, or falls. Bring a list of all your medications - including supplements - to your doctor and ask: “Could any of these be causing this?”
Are over-the-counter drugs safe for older adults?
Not always. Many OTC drugs - like Benadryl, sleep aids, and pain relievers - contain ingredients that are risky for older adults. Anticholinergics in allergy and sleep meds can cause confusion and urinary retention. NSAIDs like ibuprofen can cause stomach bleeding or kidney damage. Always check with a pharmacist before taking any OTC medication.
What’s the best way to reduce medication risks in older adults?
The best approach is a combination of regular medication reviews, using the Beers Criteria and STOPP/START guidelines, doing a Brown Bag Review with all your pills, and working with a pharmacist. Start with the lowest possible dose. Ask if any drugs can be stopped. And don’t assume new symptoms are just part of aging - they might be drug-related.






Guillaume VanderEst
December 18, 2025 AT 23:55My grandma took Benadryl for allergies and turned into a confused zombie for three days. No one told her it was dangerous for seniors. She thought it was just "getting old." Turned out it was the meds. Now she’s off everything except her blood pressure pill and she’s walking again. Funny how a simple swap fixes so much.
Doctors act like pills are candy. They’re not.
Nina Stacey
December 19, 2025 AT 15:04ok so i just wanna say i love this post so much like honestly i’ve been begging my dad to get his meds reviewed for years and he’s 79 and he’s on like 12 pills and he swears he’s fine but he’s always stumbling and forgetting where he put his glasses and i kept thinking oh he’s just aging but nooo it was the amitriptyline and the ibuprofen and the zolpidem and honestly i cried when his pharmacist pulled all the beers criteria meds and said ‘this is why you’re confused’
he’s been on deprescribing for 4 months now and he’s playing chess again and remembering birthdays and i just want everyone to know it’s not normal to feel like a foggy ghost at 80
pls talk to your pharmacist they’re the real heroes
Dominic Suyo
December 21, 2025 AT 05:26Let’s be real - this isn’t medicine. It’s pharmaceutical negligence dressed up as ‘standard care.’
Doctors get paid per prescription. Geriatric pharmacology? Not on the CME menu. They’re prescribing 40-year-old dosing protocols to octogenarians like it’s 1998. The Beers Criteria isn’t a suggestion - it’s a death warrant ignored by the system.
And don’t get me started on the ‘brown bag’ reviews. Half the time the doctor glances at the pills and says ‘oh, interesting’ like it’s a trivia game. Meanwhile, grandma’s kidneys are turning to dust because someone thought ‘it’s just a little naproxen.’
AI tools like MedAware? Cool. But they’re band-aids on a hemorrhage. The real fix is firing every MD who still thinks ‘start low and go slow’ is optional.
And yes - I’ve seen this kill three people in my family. It’s not anecdotal. It’s systemic.
Janelle Moore
December 21, 2025 AT 06:44Did you know the FDA allows drug trials with only 5% seniors? That’s because the pharmaceutical industry doesn’t want to pay for real data - they want profits. The Beers Criteria? A joke. They’re just trying to scare you so you’ll buy ‘safer’ drugs that cost 10x more.
My neighbor stopped all his meds and now he’s healthy. The doctors said he’d die. He’s 85 and mows his lawn. Coincidence? I think not.
They’re poisoning us with pills and calling it care. Wake up.
Also - 5G is making dementia worse. Don’t ignore the signs.
Aadil Munshi
December 22, 2025 AT 16:42It’s funny how we romanticize aging as wisdom and grace, yet treat the body like a broken machine that just needs more parts.
We don’t give a 20-year-old a 40-year-old’s insulin dose - so why do we give a 75-year-old a 50-year-old’s warfarin? It’s not ignorance. It’s arrogance wrapped in white coats.
And let’s not pretend ‘polypharmacy’ is just a buzzword - it’s the quiet genocide of the elderly. We call it ‘standard of care’ while their kidneys fail, their brains fog, and their dignity evaporates one pill at a time.
Deprescribing isn’t risky - it’s the only ethical choice. The real danger isn’t stopping meds. It’s continuing them because no one had the guts to ask: ‘Why are we doing this?’
Frank Drewery
December 24, 2025 AT 13:00This is so important. My mom was on 8 meds and kept falling. We thought it was her balance. Turned out it was the combination of her blood pressure med and the sleep aid. After the review, they cut 3 and lowered the others. She hasn’t fallen in 8 months.
It’s not magic. It’s just listening.
Thank you for writing this. I’m sharing it with everyone I know.
mary lizardo
December 25, 2025 AT 12:42The author’s argument is both clinically sound and structurally coherent, yet the casual tone and lack of formal citations undermine its academic credibility. The Beers Criteria, while widely adopted, remains a consensus document - not a randomized controlled trial. Moreover, the conflation of correlation with causation in anecdotal patient reports is methodologically unsound.
Furthermore, the assertion that 50-60% of senior medication-related hospitalizations are preventable lacks a peer-reviewed source. While the intent is commendable, the presentation risks diluting legitimate clinical concerns with emotional rhetoric.
For a truly evidence-based approach, one must consult the Cochrane Reviews on deprescribing, not Reddit testimonials.
jessica .
December 26, 2025 AT 20:27They’re trying to take away our meds so they can control us. Who benefits? Big Pharma? The WHO? The CDC? They want seniors weak so they can push vaccines and forced care.
My uncle took his pills and lived to 92. Now they want him off everything? That’s not medicine - that’s tyranny.
And why do they always blame the drugs? What about the chemicals in the water? The fluoride? The 5G towers? Nobody talks about that.
Stay strong. Don’t let them take your pills.