The first company to file a generic drug application with a patent challenge gets 180 days of exclusive rights to sell that generic version - no one else can enter the market during that time. This isn’t a reward for being first in line. It’s a carefully designed legal tool meant to shake up the drug market, lower prices, and get affordable medicines to patients faster. But the system is far from simple. It’s filled with legal traps, strategic delays, and billion-dollar stakes. And if you think it’s just about who files first, you’re missing half the story.
How the 180-Day Clock Starts
The rule comes from the Hatch-Waxman Act of 1984, a law that tried to balance two things: protecting brand-name drug patents and letting generics in quickly. The key is the Paragraph IV certification. That’s when a generic company says, "This patent is invalid, or we won’t break it." It’s a legal challenge wrapped in a paperwork form. The first company to file that form with a complete application gets the exclusivity.
But here’s the twist: the 180 days don’t always start when the FDA approves the drug. They can start when a court rules in the generic company’s favor - even if the FDA hasn’t signed off yet. That means a company could win a lawsuit in January, sit on it for 18 months, and then launch in July. During that entire time, no other generic can enter. The clock is running, but the market stays locked.
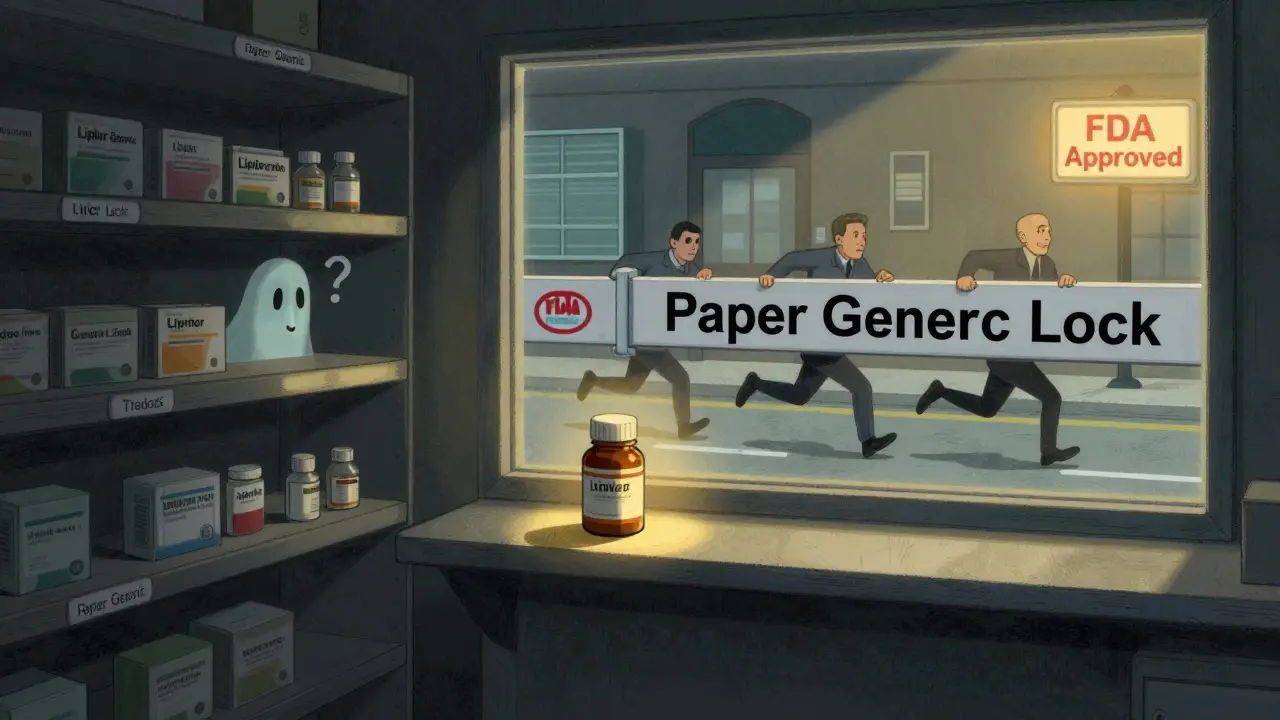
This loophole has been exploited. Some companies file a Paragraph IV challenge, win the court case, then delay launching the drug. Why? To block competitors. It’s called a "paper generic." The company never sells the drug, but no one else can either. The brand-name company wins too - they keep their monopoly. Patients lose. The FDA says this undermines the whole point of the law.
Why It’s Worth Billions
That 180-day window isn’t just a perk - it’s a financial jackpot. The first generic entrant usually captures 70% to 80% of the entire market share during that time. For a blockbuster drug like Lipitor or Nexium, that means hundreds of millions, sometimes over a billion dollars in sales. Teva made $1.2 billion in 180 days selling a generic version of Copaxone. That’s not luck. That’s strategy.
Companies invest $5 million to $10 million just to prepare for a Paragraph IV challenge. They hire patent lawyers, run complex analyses, and prepare for lawsuits that can last years. But the payoff is worth it. A generic drug with first-filer status can be worth 200% to 300% more than one that comes in second. That’s why big players like Teva, Viatris, and Sandoz file most of these challenges - they have the money and the legal teams to play the game.
The Dark Side: Reverse Payments and Authorized Generics
It’s not just about waiting. Sometimes, the brand-name company pays the first generic filer not to launch. These are called "reverse payments." The brand company offers the generic maker millions of dollars to delay their product. In return, the generic company sits still. The brand keeps its high prices. Patients pay more. The FTC estimates this costs U.S. consumers $3.5 billion a year.
There’s another trick: the "authorized generic." The brand company launches its own generic version - same drug, same packaging, just a different label - right when the 180-day clock starts. Now, instead of one generic competitor, you have two: the original filer and the brand’s own version. The brand still controls the market. The first filer gets a cut. Patients get no real price drop. Reddit threads from former pharma execs reveal this happens more than people think. One anonymous post said, "We paid first filers up to $50 million not to launch for 18 months. Cheaper than losing everything."
Why the System Is Broken
The FDA admits it. In 2022, Commissioner Robert Califf told Congress the current system has been "manipulated in ways that delay generic competition rather than accelerate it." Since 2010, nearly half of all Paragraph IV filings have led to delays. On average, patients wait 27 months longer than they should before generics enter the market.
Why? Because the law doesn’t require actual market entry to trigger the exclusivity. It only requires a court win or a launch. So companies game the system. They file, win in court, and do nothing. The FDA can’t approve anyone else. The clock ticks. The market stays empty. Patients keep paying brand prices.
There’s also the "multi-filer" problem. Sometimes, two or more companies file on the same day. Who gets the exclusivity? The FDA has to dig into filing timestamps down to the second. It’s messy. It’s slow. And it creates legal chaos. One regulatory consultant told a Drug Information Association forum, "Determining true first applicant status requires analyzing filing timestamps down to the second. It’s a nightmare."

What’s Being Done to Fix It
The FDA proposed a fix in 2022: make the 180-day clock start only when the generic drug actually hits the market. No more paper generics. No more court wins that don’t lead to sales. If you don’t launch, you don’t get exclusivity. Simple. Fair. This would force companies to either compete or walk away.
The new Competitive Generic Therapy (CGT) program, created in 2017, already does this right. CGT exclusivity starts only when the drug is sold. No court wins, no delays. Just launch or lose. The FDA has already used CGT exclusivity for over 70 drugs since 2022. It works. Why not expand it?
But the brand-name drug industry is fighting back. PhRMA argues that changing the rule would hurt innovation. They say if generics don’t have this big reward, they won’t challenge patents. But the data says otherwise. Since Hatch-Waxman, 90% of prescriptions in the U.S. are for generics. The system already works. It just needs a reset.
Who Benefits - and Who Doesn’t
Who wins? The first generic filer. Big pharma companies with legal teams. And sometimes, the brand company if they strike a deal.
Who loses? Patients. Medicare. Medicaid. Small generic companies that can’t afford the $10 million price of entry. And the public, who pay more for drugs than any other country.
Every year, Americans spend $2.2 trillion on healthcare. Generic drugs make up 90% of prescriptions but only 22% of spending. That’s the power of competition. But if the first filer never launches, that power disappears. The system was built to save money. Now, it’s being used to protect it.
The fix isn’t complicated. Make exclusivity real. If you don’t sell the drug, you don’t get the monopoly. No loopholes. No delays. No reverse payments. Just a fair race to the market.
The FDA has the power to change this. Congress has the power to write new rules. The question is: who will act before another generation pays too much for medicine?
What is a Paragraph IV certification?
A Paragraph IV certification is a legal statement filed by a generic drug company with its Abbreviated New Drug Application (ANDA). It declares that a patent listed for the brand-name drug is either invalid, unenforceable, or won’t be infringed by the generic version. This triggers a 30-month stay on FDA approval and makes the filer eligible for 180 days of market exclusivity if they’re the first to file.
Can multiple companies share the 180-day exclusivity?
Yes, but only under specific conditions. If two or more companies file identical ANDAs with Paragraph IV certifications on the same day, and all meet the requirements, they can share the exclusivity period. However, if one company starts marketing first, they get the full 180 days, and the others lose their rights. This is why filing timing matters down to the second.
What happens if the first filer never launches the drug?
If the first filer wins a court case but never markets the drug, the 180-day clock still starts - blocking all other generics from entering the market. This is called a "paper generic," and it’s a major problem. The FDA has tried to close this loophole, but under current law, the exclusivity period still runs even without a product launch, delaying competition for years.
Why do brand-name companies pay generic makers not to launch?
These payments, called "reverse payments," happen when a brand-name company pays a generic manufacturer to delay entering the market. Instead of losing 100% of sales to competition, the brand pays the generic to stay out. This keeps prices high and protects profits. The FTC has called this anti-competitive and estimates it costs consumers $3.5 billion annually.
Is the 180-day exclusivity still useful today?
Yes - but only if it works as intended. When a first filer actually launches, the exclusivity drives down prices fast and saves billions. The problem isn’t the rule itself - it’s how it’s abused. The original goal was to speed up access to affordable drugs. Today, too often, it’s used to delay them. Reforming it to require actual market entry would restore its purpose.







Lexi Karuzis
January 27, 2026 AT 23:35This is literally a legalized scam-180 days of monopoly just for filing paperwork? And they don’t even have to sell anything?! The FDA’s asleep at the wheel. I’ve seen this happen with my dad’s insulin-$600 a vial for years, then suddenly, a "generic" appears… but it’s just the brand’s own label with a different name. Reverse payments? Of course they’re happening. They’re just too rich to get caught. The system is rigged, and we’re the ones paying.
Brittany Fiddes
January 29, 2026 AT 15:19Oh please. You Americans think you invented capitalism, but this? This is third-world corruption dressed in a suit. In the UK, we don’t let pharmaceutical giants hold the entire market hostage for half a year just because someone filed a form. We have real competition. Real transparency. And real patients who don’t have to choose between rent and medication. You’ve turned healthcare into a poker game-and the house always wins. Pathetic.
Amber Daugs
January 31, 2026 AT 08:35Let me be clear: if you’re not launching a drug after winning a patent challenge, you shouldn’t get exclusivity. Period. Full stop. This isn’t rocket science. It’s basic ethics. The Hatch-Waxman Act was meant to lower prices-not create a legal loophole for billionaires to sit on a patent like a dragon hoarding gold. And don’t even get me started on authorized generics. That’s not competition-that’s collusion with a fancy label. The FDA has the power to fix this. Why haven’t they? Because they’re bought off. Or scared. Or both.
Ambrose Curtis
February 1, 2026 AT 07:25bro i worked at a small generic co and we tried to file a paragraph iv on a major drug-spent 8 months and $2 mil just to get the docs right. then we found out another company filed the day before. we didn’t even know. the timestamp was 3 seconds earlier. 3 SECONDS. and now they’ve been sitting on it for 2 years. no product. no sales. just blocking everyone. the system is BROKEN. we’re not even allowed to talk about this without getting sued. pharma execs are laughing at us while we pay $500 for a pill that costs 7 cents to make.
Linda O'neil
February 2, 2026 AT 03:04If you’re reading this and you’re a patient struggling to afford meds-know this: you’re not alone. And change is possible. The CGT program proves it. When the FDA requires actual market entry, prices drop FAST. Look at the 70+ drugs already approved under CGT. Patients saved billions. We need to expand that model to EVERYTHING. It’s not about punishing companies-it’s about making sure the law serves people, not profits. We can fix this. We just have to demand it.
Robert Cardoso
February 4, 2026 AT 02:32Let’s deconstruct the economics. The 180-day exclusivity is a classic rent-seeking mechanism. The first filer doesn’t create value-they extract monopoly rents by exploiting regulatory ambiguity. The real innovation is in legal strategy, not pharmacology. The FDA’s failure to require launch as a trigger for exclusivity is a regulatory capture case study. The cost to society? Estimated at $12B annually in delayed savings. The fix? Simple: amend the statute to require commercialization. No launch = no exclusivity. No exceptions. The fact that this isn’t already law proves the regulatory state is captured by industry interests.
James Dwyer
February 6, 2026 AT 00:58I know this sounds dark, but there’s hope. People are waking up. More patients are speaking out. More lawmakers are asking questions. And the FDA’s own proposal to tie exclusivity to actual sales? That’s a win. We just need to push harder. Tell your reps. Share this post. Talk to your pharmacist. Change doesn’t come from the top-it comes from us. We’ve done it before with HIV meds, insulin, epinephrine. We can do it again.
jonathan soba
February 7, 2026 AT 14:26