Wellbutrin and Alcohol: Risks, Reactions, and What You Need to Know
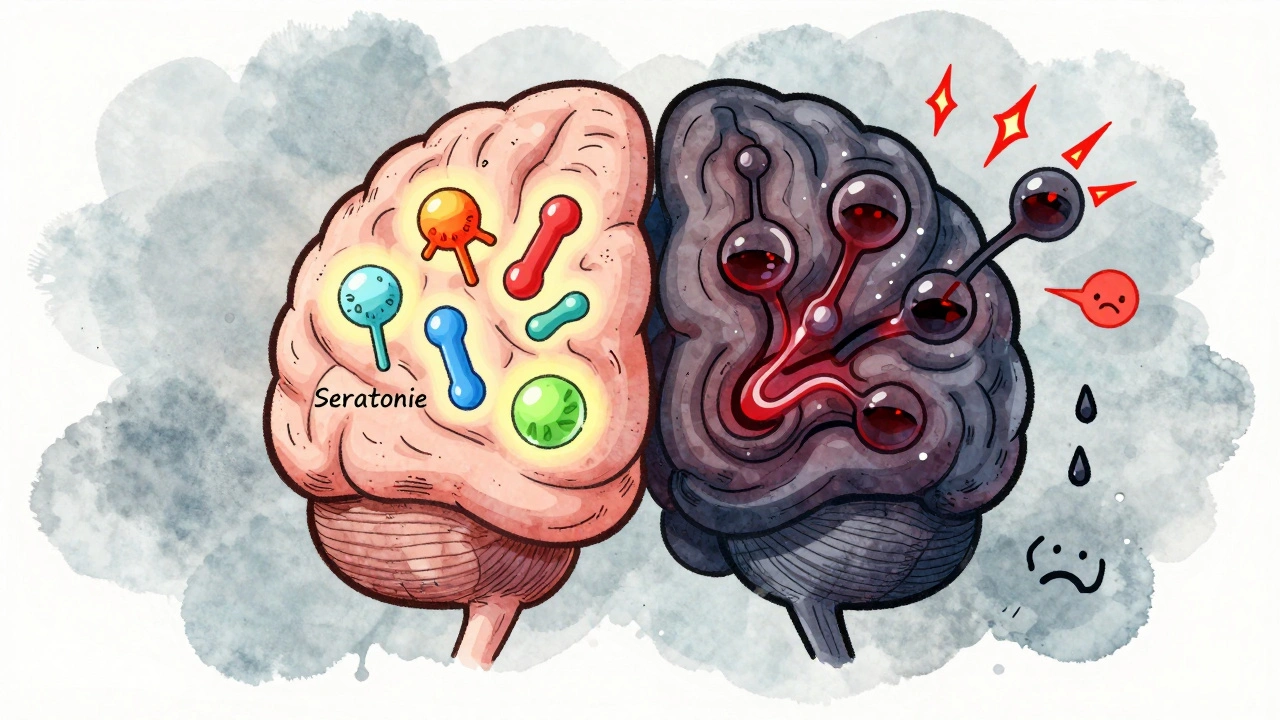
When you take Wellbutrin, a brand name for the antidepressant bupropion, used to treat depression and help with smoking cessation. Also known as bupropion, it works differently than most antidepressants by targeting dopamine and norepinephrine, not serotonin. That’s why many people think it’s "safer" to drink while on it. But mixing Wellbutrin and alcohol isn’t just a bad idea—it can trigger seizures, spike blood pressure, and worsen depression. This isn’t theoretical. The FDA and multiple clinical studies have flagged this combination as high-risk, especially at higher doses.
Alcohol doesn’t just dull the effects of Wellbutrin—it actively fights against it. While Wellbutrin helps stabilize mood by boosting brain chemicals, alcohol suppresses them. The result? You might feel worse after drinking, even if you took your pill. Worse, alcohol lowers your seizure threshold, and Wellbutrin already raises that risk slightly on its own. At doses above 450 mg per day, the chance of a seizure jumps significantly. Add alcohol, and that risk multiplies. People with eating disorders, liver problems, or a history of seizures are especially vulnerable. You might think one drink won’t hurt, but your body doesn’t know the difference between one drink and two when it’s already under chemical stress.
There’s also the mental health side. Wellbutrin is often prescribed because other antidepressants made people feel numb or sluggish. But alcohol can undo that progress fast—leading to increased anxiety, irritability, or even suicidal thoughts. It’s not just about physical reactions; it’s about your recovery. If you’re using Wellbutrin to get through a tough time, alcohol doesn’t help you cope—it makes the coping harder.
Some people try to justify drinking by saying they’ve done it before with no issues. But that’s like saying, "I’ve driven without a seatbelt and never crashed." Risk isn’t always immediate. The damage builds quietly. And if you’re on Wellbutrin for depression, you’re already at higher risk for impulsive decisions—including drinking more than you planned.
What you’ll find in the articles below isn’t just a list of warnings. You’ll see real-world examples of how people managed this balance, what doctors actually recommend when someone wants to drink occasionally, and how to spot early signs of trouble. We’ll also cover what to do if you’ve already mixed them, how to talk to your provider about it without shame, and what alternatives exist if you want to cut back on alcohol while staying on medication. This isn’t about fear—it’s about making informed choices that protect your health, your progress, and your future.
Antidepressants and Alcohol: What Happens When You Mix Them
Mixing antidepressants and alcohol can worsen depression, reduce medication effectiveness, and increase suicide risk. Learn why even one drink can be dangerous and what to do instead.





