SSRI and Alcohol: Risks, Effects, and What You Need to Know
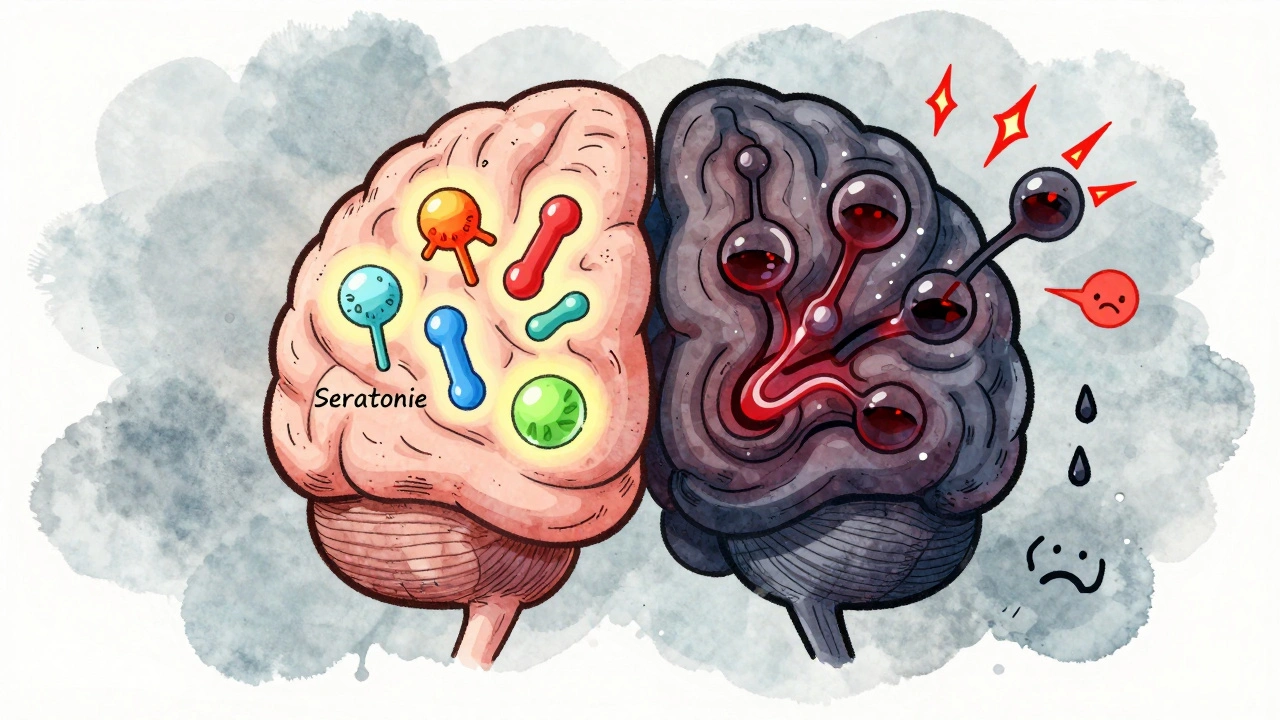
When you take a SSRI, a type of antidepressant that increases serotonin in the brain to improve mood. Also known as selective serotonin reuptake inhibitor, it’s one of the most common treatments for depression and anxiety. But if you’re drinking alcohol, a central nervous system depressant that affects brain chemistry and slows bodily functions while on an SSRI, you’re playing with fire—even if you think it’s just one drink. The combination doesn’t just make you feel more tired. It can worsen your symptoms, trigger dangerous side effects, and even lead to a life-threatening condition called serotonin syndrome, a buildup of too much serotonin in the body, often caused by mixing drugs that affect serotonin levels.
SSRIs like sertraline, fluoxetine, or escitalopram work by keeping serotonin active in your brain. Alcohol, on the other hand, lowers serotonin over time and messes with your sleep, judgment, and coordination. When you mix them, your body gets conflicting signals. You might feel more depressed, more anxious, or more dizzy than usual. Some people think alcohol helps with SSRI side effects like insomnia or low mood—but it doesn’t. It makes them worse. Studies show that even moderate drinking reduces how well SSRIs work, and increases the chance of relapse. And if you’re someone who drinks regularly, your liver might not process the SSRI properly, leading to higher drug levels in your blood and more side effects.
The biggest danger? Serotonin syndrome. It doesn’t happen often, but when it does, it hits fast. Symptoms include high fever, rapid heartbeat, confusion, muscle stiffness, and seizures. It’s rare with just one drink—but if you’re taking multiple medications, drinking heavily, or suddenly increase your alcohol intake, the risk climbs. You might not notice it at first. You might think you’re just "feeling off." But if you’re on an SSRI and you drink, you need to watch for these signs. And if you’re ever in doubt, don’t wait. Call your doctor. Don’t assume it’s "just a hangover."
What the research says—and what your doctor won’t always tell you
Most guidelines say: avoid alcohol while on SSRIs. But many patients still drink. Why? Because they’re told it’s "fine in moderation." But "moderation" isn’t defined clearly, and it doesn’t account for how your body reacts. One study in the Journal of Clinical Psychiatry found that people who drank while on SSRIs reported 40% more side effects than those who didn’t. Another showed that drinkers were twice as likely to stop their medication early because they felt worse. The truth? There’s no safe level of alcohol when you’re treating depression. It’s not about how much you drink—it’s about what your brain is already struggling with. Alcohol is a depressant. SSRIs are trying to lift you out of depression. They’re working against each other.You might be thinking: "But I’ve had a glass of wine before and felt fine." That’s not proof it’s safe. It’s proof your body hasn’t reacted yet. Side effects build up. So do risks. And if you’re on other meds—like painkillers, sleep aids, or even herbal supplements—the mix gets even more dangerous. The posts below cover real cases: people who didn’t realize how alcohol was sabotaging their treatment, how serotonin syndrome sneaks up on you, and what alternatives actually work when you want to unwind without risking your mental health.
Antidepressants and Alcohol: What Happens When You Mix Them
Mixing antidepressants and alcohol can worsen depression, reduce medication effectiveness, and increase suicide risk. Learn why even one drink can be dangerous and what to do instead.





