Probenecid – Uses, Dosage, and Interactions
When working with Probenecid, a uricosuric drug that helps the kidneys eliminate excess uric acid. Also known as Benemid, it’s primarily prescribed for gout and to boost the effectiveness of certain antibiotics such as penicillin.
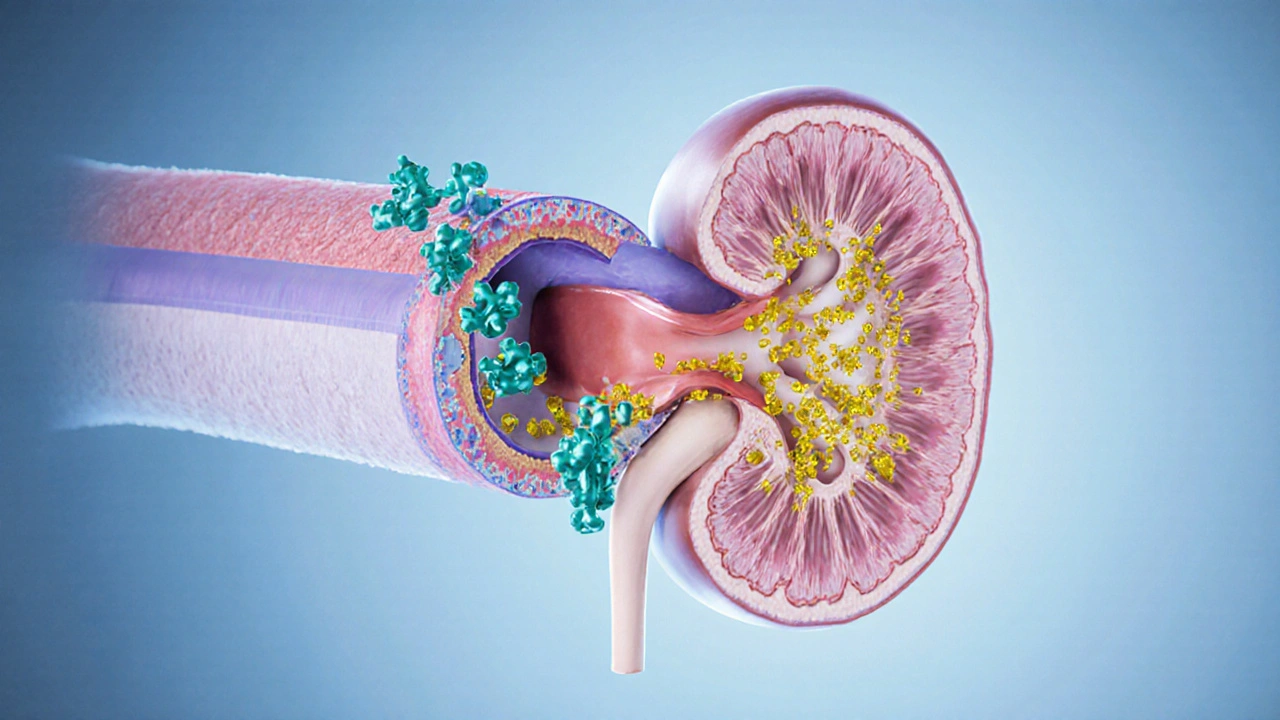
In simple terms, Probenecid works by blocking the reabsorption of uric acid in the renal tubules, which lowers blood uric‑acid levels and reduces crystal formation in joints. This mechanism creates a direct link between the drug and uric acid management, making it a cornerstone of gout therapy. Because it changes how the kidneys handle substances, clinicians also monitor kidney function before and during treatment.
Key Facts About Probenecid
Three essential facts shape how you use Probenecid: first, it lowers uric‑acid concentrations; second, it can increase plasma levels of specific antibiotics, enhancing their therapeutic effect; third, it requires regular kidney‑function checks to avoid toxicity. These three points form a semantic chain: Probenecid → uric‑acid reduction → gout relief, and Probenecid → antibiotic level boost → more reliable infection control, while Probenecid → kidney monitoring → safety assurance.
For gout sufferers, the drug offers a non‑invasive alternative to surgery or aggressive anti‑inflammatory regimens. Patients typically start with a low dose, such as 250 mg twice daily, and adjust upward based on serum uric‑acid readings. Blood tests every few weeks help confirm that levels are dropping into the target range (usually below 6 mg/dL) without triggering kidney strain.
If you’re on penicillin, ampicillin, or ceftriaxone, Probenecid can be a useful partner. By inhibiting renal excretion, it holds the antibiotic in the bloodstream longer, allowing lower doses or fewer injections. This interaction is especially valuable in outpatient settings where IV therapy is impractical.
However, the same interaction can turn risky when combined with drugs that also rely on renal clearance, such as certain diuretics or non‑steroidal anti‑inflammatory drugs (NSAIDs). Mixing these can raise the chance of side effects like electrolyte imbalance or heightened blood pressure. Always tell your prescriber about every medication you take, including over‑the‑counter supplements.
Kidney health is the linchpin of safe Probenecid use. Before starting, doctors assess creatinine clearance; a value below 30 mL/min often disqualifies patients because the drug’s benefit‑risk profile shifts. During therapy, routine labs—creatinine, electrolytes, and uric‑acid levels—provide a feedback loop that guides dose tweaks.
Side effects are generally mild but worth knowing. The most common complaints include nausea, headache, and occasional rash. Rarely, patients experience crystal‑induced kidney stones, which underscores the need for adequate hydration—aim for at least 2 L of water a day unless fluid restriction is advised for another condition.
Special populations need extra attention. Pregnant or breastfeeding women should avoid Probenecid unless the benefits dramatically outweigh risks, as animal studies suggest possible fetal harm. Elderly patients often have reduced kidney function, so initiating therapy at the lowest dose and titrating slowly is prudent.
Summing up, Probenecid sits at the crossroads of gout management, antibiotic optimization, and kidney‑function monitoring. Understanding these relationships lets you and your healthcare provider tailor a plan that maximizes relief while keeping safety in check. Below you’ll find a curated selection of articles that dive deeper into dosage strategies, interaction warnings, and real‑world patient experiences, giving you practical insight to make informed decisions.
Benemid (Probenecid) vs Other Uric Acid Medications - Comparison Guide
A detailed comparison of Benemid (Probenecid) with gout alternatives, covering mechanism, safety, dosing, and when each drug fits best.





