Polycystic Ovary Syndrome (PCOS) affects about 1 in 10 women of childbearing age. For many, the biggest struggle isn’t just irregular periods or acne-it’s the inability to get pregnant. At the heart of this issue is a hidden problem: insulin resistance. When your body doesn’t respond properly to insulin, your ovaries get flooded with signals to make more male hormones, which shuts down ovulation. That’s where metformin comes in.
What Metformin Actually Does in PCOS
Metformin isn’t a fertility drug. It’s a diabetes medication-first developed in the 1950s-that works by helping your body use insulin better. In women with PCOS, high insulin levels directly trigger excess testosterone production, which blocks ovulation. Metformin breaks that cycle.
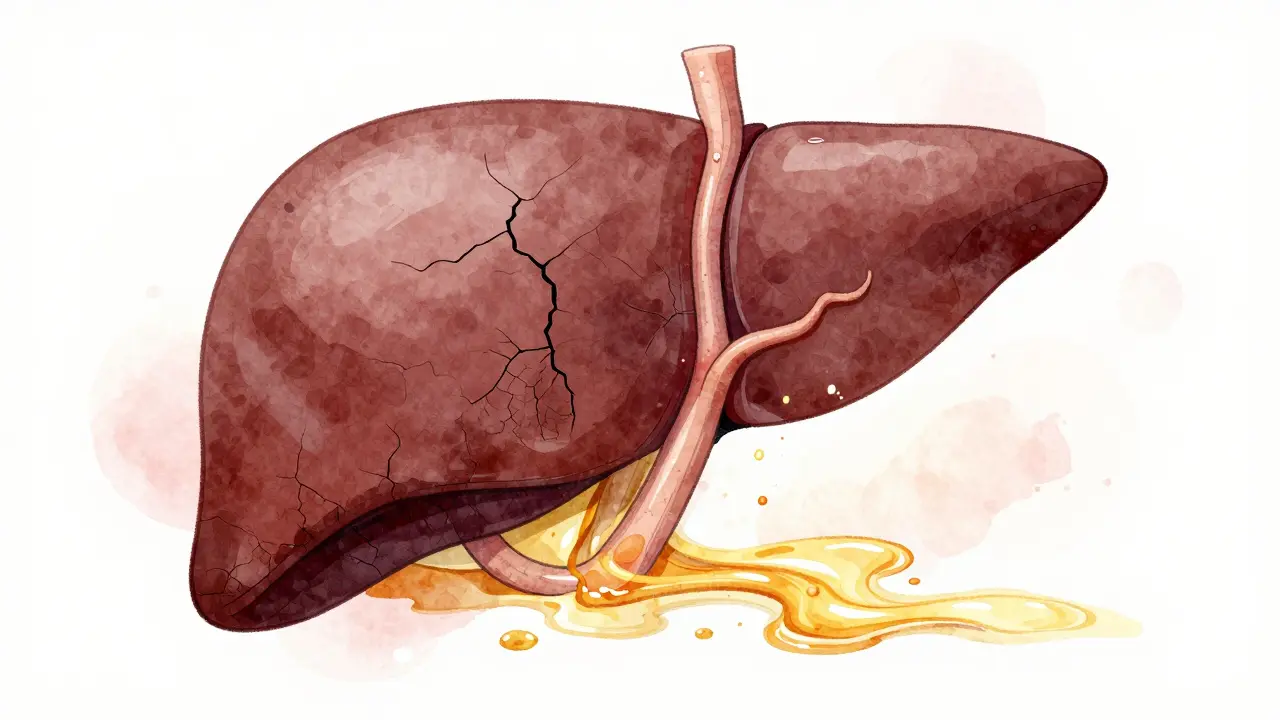
It does three key things:
- Reduces how much glucose your liver releases into your bloodstream
- Improves how muscle and fat cells absorb sugar
- Slows down sugar absorption from your gut
The result? Lower insulin levels. And when insulin drops, so does testosterone. That’s when ovulation starts to return. Studies show that after 3 to 6 months of consistent use, about 60-70% of women with PCOS begin ovulating regularly again. For some, this is the first time in years.
Does Metformin Really Help You Get Pregnant?
Yes-but not always on its own.
A Cochrane review of 44 studies found that metformin doubles the odds of ovulation compared to no treatment. It also increases the chance of clinical pregnancy by more than double. But here’s the catch: if you’re trying to conceive, metformin alone isn’t the fastest route.
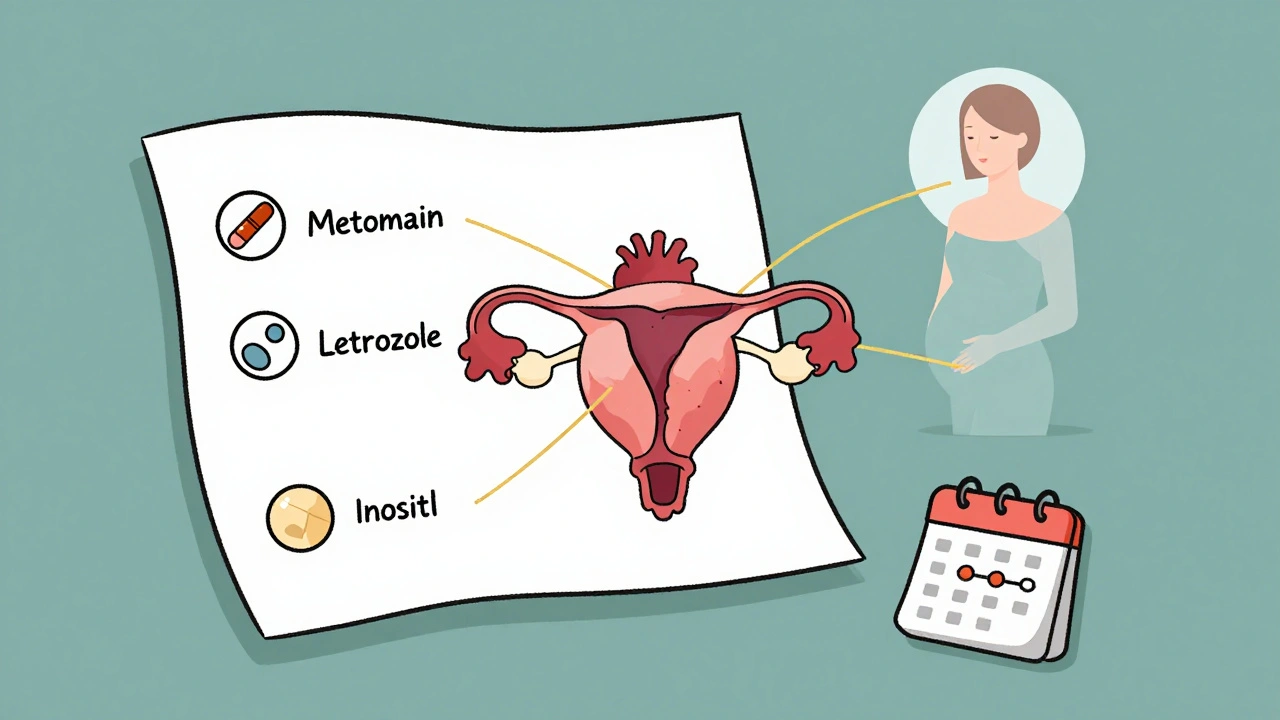
Let’s compare:
- Metformin alone: 69% ovulation rate
- Letrozole alone: 88% ovulation rate
- Letrozole + metformin: 89% ovulation rate
Letrozole, a drug originally designed for breast cancer, is now the top first-line choice for ovulation induction in PCOS. It works directly on the brain to trigger egg release. Metformin works slower-it fixes the underlying insulin problem so your body can ovulate naturally.
So why use metformin at all? Because it doesn’t just help you get pregnant-it helps you stay pregnant and stay healthy.
Why Metformin Is Better Than You Think
Most women start metformin for fertility. But the real benefits go far beyond that.
First, it cuts the risk of ovarian hyperstimulation syndrome (OHSS)-a dangerous complication during IVF-by more than 70%. That’s huge for women needing assisted reproduction.
Second, it improves pregnancy outcomes. When women continue metformin through the first trimester, clinical pregnancy rates are higher than if they stop after a positive test. It may help prevent early miscarriages, which are more common in women with PCOS due to high insulin and inflammation.
Third, it helps with long-term health. Women with PCOS have a 4-7 times higher risk of developing type 2 diabetes. Metformin reduces that risk by improving insulin sensitivity. One long-term study found that women on metformin for 3 years had a 50% lower chance of developing diabetes compared to those on placebo.
And it’s not just about diabetes. Metformin can reduce hirsutism (excess hair growth) and improve acne by lowering androgen levels. For women who can’t or won’t take birth control pills, it’s a viable alternative to manage those symptoms without hormonal suppression.
Who Benefits Most From Metformin?
Not all women with PCOS respond the same way. The biggest factor? Insulin resistance.
Women who are overweight or obese often have severe insulin resistance-and metformin helps them. But surprisingly, research now shows that non-obese women with PCOS and clear insulin resistance benefit just as much, if not more. These women often go undiagnosed because they don’t fit the "typical" PCOS profile. They might have regular periods but still struggle to ovulate.
Doctors now use fasting insulin levels, HOMA-IR scores, or glucose tolerance tests to spot insulin resistance-even in women with normal weight. If your insulin is high, metformin is likely to help.
On the other hand, if your insulin levels are normal, metformin probably won’t do much for ovulation. That’s why testing matters.
How to Take Metformin for PCOS
Most doctors start low and go slow.
Typical protocol:
- Start with 500 mg once daily with dinner
- After 1 week, increase to 500 mg twice daily
- After another week, go to 500 mg three times daily (1,500 mg total)
- If tolerated, increase to 2,000 mg daily (1,000 mg twice daily)
Many patients switch to the extended-release version (metformin XR) after experiencing stomach upset. XR releases the drug slowly, so side effects like nausea, bloating, and diarrhea drop by 50% or more. It’s often better tolerated and can be taken once a day.
Side effects usually fade within 2 to 4 weeks. Taking it with food helps. If you can’t tolerate even the XR form, your doctor may lower the dose or space it out further.
It takes time. Most women see changes in their cycle after 2 to 3 months. Ovulation is confirmed with a blood test around day 21 of your cycle-progesterone above 3 ng/mL means you ovulated.
Metformin vs. Other Treatments
Here’s how metformin stacks up against common options:
| Treatment | Ovulation Rate | Pregnancy Rate | OHSS Risk | Cost (Monthly) |
|---|---|---|---|---|
| Metformin (alone) | 60-70% | 19-37% | Low | $4-$10 |
| Letrozole (alone) | 85-90% | 25-40% | Low | $50-$100 |
| Clomiphene (alone) | 70-80% | 20-30% | Low | $30-$50 |
| Letrozole + Metformin | 88-90% | 30-45% | Very Low | $55-$110 |
| Clomiphene + Metformin | 75-85% | 25-35% | Low | $35-$60 |
Metformin isn’t the fastest, but it’s the safest and cheapest. It’s also the only one that improves your long-term metabolic health. For women planning to get pregnant soon, letrozole is still the gold standard. But for those wanting to fix the root cause, or who’ve failed clomiphene, metformin is a powerful tool.
What About Pregnancy?
Many women stop metformin as soon as they get a positive pregnancy test. But growing evidence suggests keeping it on board during the first trimester might reduce miscarriage risk.
A 2023 meta-analysis of 12 trials found women who continued metformin through the first 12 weeks had higher pregnancy success rates than those who stopped. There’s no sign of harm to the baby-metformin is classified as Category B, meaning animal studies show no risk, and human data supports safety.
Some doctors recommend stopping after the first trimester. Others keep it going until delivery, especially if the woman has prediabetes or gestational diabetes risk. It’s a personal decision with your provider.
Real Stories, Real Results
Women on Reddit’s r/PCOS forum report similar experiences:
- "Started metformin at 500mg. First week, I felt sick. By week 3, the nausea was gone. My period came back after 4 months. Pregnant at 6 months."
- "I was told I’d need IVF. Took metformin for 6 months, lost 8 pounds, started ovulating naturally. Got pregnant on my own."
- "My acne cleared up after 3 months. My hair stopped falling out. I didn’t expect that."
These aren’t outliers. They’re the result of fixing insulin resistance.
Final Thoughts: Is Metformin Right for You?
Metformin isn’t magic. It won’t work if you’re not taking it consistently. It won’t help if your PCOS isn’t driven by insulin resistance. And it won’t replace letrozole if you need a quick pregnancy.
But if you’re looking for a treatment that:
- Restores your natural cycle
- Reduces your diabetes risk
- Improves your skin and hair
- Costs less than a coffee a day
- Is safe during pregnancy
Then metformin deserves a serious look-even if it’s not your first choice.
Ask your doctor for a fasting insulin test. If it’s high, metformin might be the quiet hero your PCOS needs.
Can metformin help me ovulate if I have normal weight?
Yes. While obesity is common in PCOS, many women with normal weight still have insulin resistance. Studies show that non-obese women with elevated insulin levels respond just as well to metformin as those who are overweight. The key isn’t body weight-it’s insulin levels. A fasting insulin test or HOMA-IR score can confirm if you’re a candidate.
How long does it take for metformin to start working for ovulation?
Most women notice their periods becoming more regular after 2 to 3 months. Ovulation typically resumes within 3 to 6 months of consistent use. Some women ovulate sooner, especially if they also lose weight or improve their diet. But it’s not instant. Patience and consistency are key.
Is metformin safe during pregnancy?
Yes. Metformin is classified as Category B, meaning no evidence of harm in animal studies, and human data over decades shows no increased risk of birth defects. Many doctors recommend continuing metformin through the first trimester, especially if you have insulin resistance or prediabetes. Some continue it throughout pregnancy to reduce gestational diabetes risk. Always discuss this with your OB-GYN.
Why do some doctors say metformin doesn’t work for PCOS infertility?
Some studies show metformin alone doesn’t improve live birth rates as much as letrozole. That’s true. But those studies often compare it as a standalone treatment. Metformin works best as part of a strategy-not as a magic bullet. It’s most effective when used to improve insulin sensitivity before or alongside other fertility drugs. It’s not about replacing letrozole-it’s about making it work better.
Can I take metformin with other supplements like inositol?
Yes. Inositol, especially myo-inositol and D-chiro-inositol, is often used alongside metformin for PCOS. Both improve insulin sensitivity and have been shown in studies to enhance ovulation rates. Many women combine them with no side effects. Some doctors even recommend inositol as a first step before starting metformin, especially for mild cases.
What if metformin gives me bad stomach issues?
You’re not alone. Up to 30% of people experience nausea, bloating, or diarrhea at first. Switching to the extended-release version (XR) reduces side effects by half. Take it with meals, start low, and increase slowly. Most side effects fade within 2 to 4 weeks. If they don’t, talk to your doctor about lowering the dose or trying a different approach.
Does metformin help with PCOS acne and hair growth?
Yes. By lowering insulin and testosterone, metformin reduces hirsutism (excess hair) and improves acne. It can take 3 to 6 months to see results, but many women report noticeable improvements without needing birth control pills or anti-androgen medications. It’s a good option for those who want to avoid hormonal treatments.



Lara Tobin
December 13, 2025 AT 04:53Jamie Clark
December 14, 2025 AT 20:31Keasha Trawick
December 16, 2025 AT 04:43Bruno Janssen
December 16, 2025 AT 09:18Emma Sbarge
December 18, 2025 AT 08:48Deborah Andrich
December 19, 2025 AT 21:59Tommy Watson
December 21, 2025 AT 15:26Willie Onst
December 22, 2025 AT 07:39Casey Mellish
December 24, 2025 AT 04:24Tyrone Marshall
December 25, 2025 AT 19:49kevin moranga
December 27, 2025 AT 16:36Alvin Montanez
December 29, 2025 AT 13:56