Benemid vs Other Uric Acid Medications Comparison Tool
Comparison Results
| Drug | Class | Mechanism | Typical Dose | Pros | Cons |
|---|---|---|---|---|---|
| Benemid (Probenecid) | Uricosuric | Inhibits URAT1 → ↑ renal uric acid excretion | 250 mg‑1 g BID (max 2 g/day) | Effective when production inhibitors fail; cheap | Kidney stones; drug interactions; requires good hydration |
| Allopurinol | Xanthine oxidase inhibitor | Blocks conversion of hypoxanthine → xanthine → uric acid | 100 mg‑300 mg daily (adjust for renal function) | Well‑studied; broad experience; reduces urate production | Allopurinol hypersensitivity syndrome; less effective in high urate loads |
| Febuxostat | Xanthine oxidase inhibitor | Selective inhibition of xanthine oxidase | 40 mg‑80 mg daily | Works in patients with mild renal impairment; lower hypersensitivity risk | Higher cost; cardiovascular safety concerns in some studies |
| Lesinurad | Uricosuric (adjunct) | Inhibits URAT1, used with allopurinol/febuxostat | 200 mg daily (often combined) | Boosts effect of production inhibitors; useful in refractory cases | Increases kidney stone risk; limited as monotherapy |
| Rasburicase | Uricase enzyme | Converts uric acid → allantoin (soluble) | 0.2 mg/kg IV, 1‑5 days as needed | Rapid urate reduction; life‑saving in tumor lysis | IV only; expensive; contraindicated in G6PD deficiency |
| Pegloticase | Recombinant uricase | Converts uric acid → allantoin | 0.14 mg/kg IV bi‑weekly | Effective in refractory chronic gout | High cost; infusion reactions; requires pre‑medication |
When treating gout, Benemid is a uricosuric medication (probenecid) that increases renal excretion of uric acid. It’s been on the market for decades, yet many patients wonder how it stacks up against newer options. This guide walks you through the science, safety profile, and real‑world pros and cons of Benemid, then pits it side‑by‑side with the most common alternatives so you can pick the right drug for your gout or hyperuricemia situation.
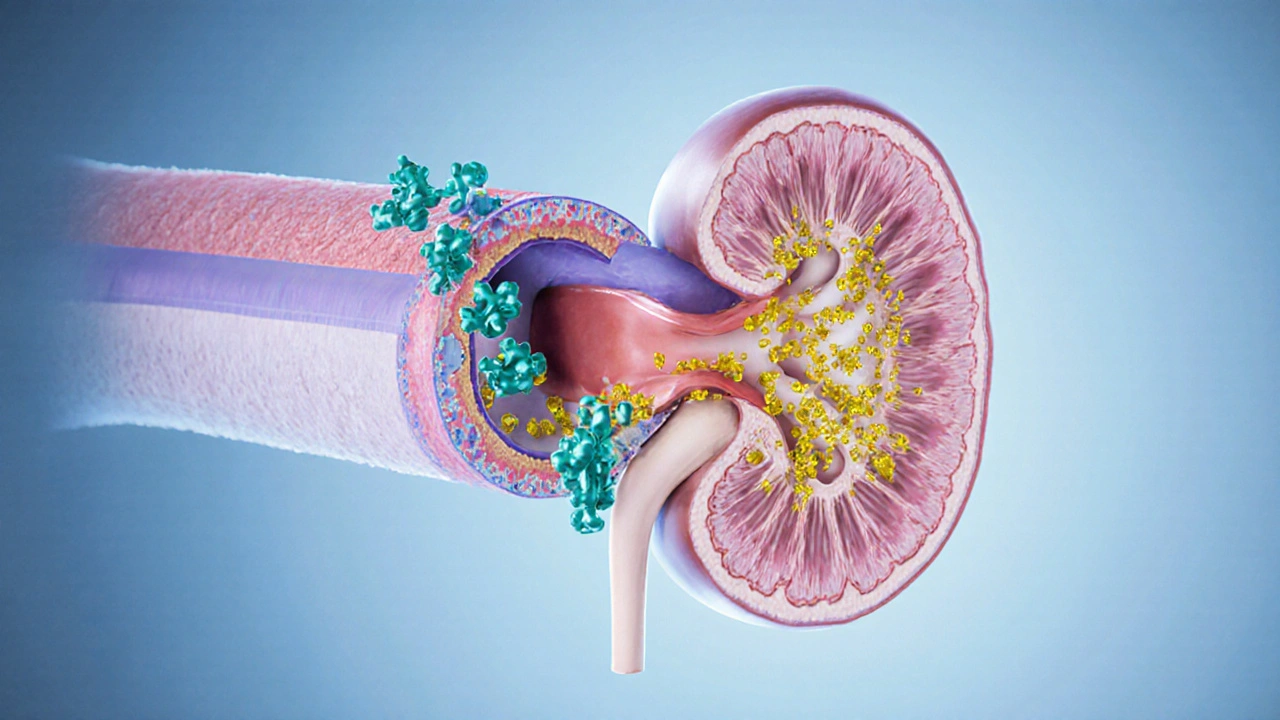
What Benemid (Probenecid) Actually Does
Benemid belongs to the uricosuric agents a class of drugs that block the reabsorption of uric acid in the renal tubules. By inhibiting the transporterURAT1, it forces the kidneys to dump more uric acid into the urine, lowering serum urate levels. Typical dosing starts at 250mg twice daily, adjusted up to 2g per day based on serum urate response and kidney function.
When Doctors Choose Benemid
- Patients who can’t tolerate xanthine oxidase inhibitors (allopurinol or febuxostat).
- Those with mild to moderate renal impairment where uricosurics remain effective.
- Individuals who need rapid urate reduction during acute flares, combined with colchicine or NSAIDs.
Because Benemid works by flushing uric acid out, it can increase the risk of kidney stones. Adequate hydration-at least 2-3L of water daily-is essential.
Safety Snapshot
Common side effects include:
- Kidney stones (nephrolithiasis) - the biggest concern.
- Gastro‑intestinal upset (nausea, dyspepsia).
- Rash or mild allergic reactions.
Serious but rare events are hemolysis in patients with glucose‑6‑phosphate dehydrogenase (G6PD) deficiency and severe hypersensitivity. Drug interactions are notable: Benemid can raise plasma levels of penicillins, cephalosporins, and certain NSAIDs by competing for renal tubular secretion.
Alternatives on the Market
Below are the main competitors you’ll hear about:
Allopurinol a xanthine oxidase inhibitor that blocks uric acid production.
Febuxostat a more selective xanthine oxidase inhibitor used when allopurinol is ineffective or not tolerated.
Lesinurad a uricosuric that works alongside a xanthine oxidase inhibitor to boost uric acid excretion.
Rasburicase an enzyme that converts uric acid to the more soluble allantoin, used mainly in tumor lysis syndrome.
Pegloticase a PEG‑ylated recombinant uricase for refractory chronic gout.
Side‑by‑Side Comparison Table
| Drug | Class | Mechanism | Typical Dose | Pros | Cons |
|---|---|---|---|---|---|
| Benemid (Probenecid) | Uricosuric | Inhibits URAT1 → ↑ renal uric acid excretion | 250mg‑1g BID (max 2g/day) | Effective when production inhibitors fail; cheap | Kidney stones; drug interactions; requires good hydration |
| Allopurinol | Xanthine oxidase inhibitor | Blocks conversion of hypoxanthine → xanthine → uric acid | 100mg‑300mg daily (adjust for renal function) | Well‑studied; broad experience; reduces urate production | Allopurinol hypersensitivity syndrome; less effective in high urate loads |
| Febuxostat | Xanthine oxidase inhibitor | Selective inhibition of xanthine oxidase | 40mg‑80mg daily | Works in patients with mild renal impairment; lower hypersensitivity risk | Higher cost; cardiovascular safety concerns in some studies |
| Lesinurad | Uricosuric ( adjunct ) | Inhibits URAT1, used with allopurinol/febuxostat | 200mg daily (often combined) | Boosts effect of production inhibitors; useful in refractory cases | Increases kidney stone risk; limited as monotherapy |
| Rasburicase | Uricase enzyme | Converts uric acid → allantoin (soluble) | 0.2mg/kg IV, 1‑5days as needed | Rapid urate reduction; life‑saving in tumor lysis | IV only; expensive; contraindicated in G6PD deficiency |
| Pegloticase | Recombinant uricase | Converts uric acid → allantoin | 0.14mg/kg IV bi‑weekly | Effective in refractory chronic gout | High cost; infusion reactions; requires pre‑medication |

Choosing the Right Medicine - Decision Guide
- Is uric acid over‑production the main issue? If labs show high uric acid synthesis, start with a xanthine oxidase inhibitor (allopurinol or febuxostat).
- Do you have kidney stones or a history of nephrolithiasis? Skip Benemid and lesinurad; they raise stone risk.
- Is renal function compromised? Allopurinol dose‑adjusts well; febuxostat tolerates mild impairment; uricosurics need decent GFR.
- Are you on medications that share renal tubular pathways? Check for penicillins, cephalosporins, NSAIDs; Benemid may need dose changes.
- Do you need rapid urate clearance (e.g., tumor lysis or severe flare)? Consider rasburicase or pegloticase rather than oral agents.
In practice, many clinicians start with allopurinol, add benemid only if urate targets aren’t reached, and reserve lesinurad for the toughest cases. Febuxostat serves as an all‑in‑one alternative when allopurinol isn’t tolerated.
Practical Tips for Patients on Benemid
- Drink at least 2L of water daily; consider potassium citrate to reduce stone formation.
- Monitor serum urate every 2-4weeks until stable, then every 3-6months.
- Check kidney ultrasound annually if you have a prior stone history.
- Inform your doctor about any antibiotics or NSAIDs you’re taking.
- Report any rash, fever, or sudden joint pain - could signal hypersensitivity.
Frequently Asked Questions
Can Benemid be used together with allopurinol?
Yes. Combining a uricosuric like Benemid with a xanthine oxidase inhibitor can achieve deeper serum urate reductions, especially in patients who don’t hit targets on a single agent.
What’s the biggest advantage of Benemid over febuxostat?
Cost. Benemid is generic and inexpensive, while febuxostat carries a higher price tag, which matters for long‑term gout management.
Is Benemid safe for people with mild kidney disease?
Generally, yes, as long as the glomerular filtration rate (GFR) stays above ~30mL/min and the patient stays well‑hydrated. Below that, uricosurics lose effectiveness and stone risk rises.
How quickly does Benemid lower serum urate?
You can see a 15‑20% drop within 1‑2weeks, reaching a plateau around 4‑6weeks. Adjusting dose may add a few more percentage points.
Do I need regular blood tests while on Benemid?
Yes. Besides serum urate, monitor renal function (creatinine, eGFR) and liver enzymes every 3‑6months, especially if you’re on other nephrotoxic drugs.
Whether you’re a long‑time gout sufferer or newly diagnosed with hyperuricemia, understanding how Benemid compares to its peers helps you and your doctor make an evidence‑based choice. Keep the hydration mantra, watch for stones, and don’t hesitate to revisit the treatment plan if goals aren’t met.






Matt Cress
October 7, 2025 AT 15:14Oh great, another med compare tool, ’cause we needed more decision fatigue.
Andy Williams
October 13, 2025 AT 09:54Benemid’s standard dosing begins at 250 mg twice daily, titratable up to 2 g per day. The dosage is adjusted according to serum urate response and renal function. It remains a cost‑effective option compared with newer agents, provided patients maintain adequate hydration.
Paige Crippen
October 19, 2025 AT 04:34One can’t ignore the possibility that pharmaceutical companies subtly steer clinicians toward newer, pricier drugs while keeping older, cheap options like Benemid under the radar.
sweta siddu
October 24, 2025 AT 23:14Great guide! 👍 It really helps to see the pros and cons side‑by‑side. 🌟 Stay hydrated and you’ll avoid most stone issues.
Ted Mann
October 30, 2025 AT 16:54When we contemplate uric acid, we are, in essence, confronting the body’s relentless pursuit of equilibrium. Benemid nudges the kidneys to relinquish excess, a subtle rebellion against metabolic inertia. Yet this rebellion is not without consequence; stones may form like uninvited guests at a party. The philosophy here mirrors many of life’s compromises-gain a benefit, accept a risk. Ultimately, the choice reflects personal thresholds for discomfort versus control.
Brennan Loveless
November 5, 2025 AT 11:34American patients shouldn’t have to pay a premium for a drug that’s been generic for decades. The market pushes newer, expensive alternatives like a patriotic parade of profit. Keep the focus on efficacy, not brand‑name fireworks.
Vani Prasanth
November 11, 2025 AT 06:14Pro tip: drink at least 2–3 L of water daily while on Benemid to flush out crystals.
Maggie Hewitt
November 17, 2025 AT 00:54Because the only thing cheaper than Benemid is my patience.
Mike Brindisi
November 22, 2025 AT 19:34Benemid works by blocking URAT1 increasing uric acid excretion it’s simple yet effective many patients tolerate it well however watch out for drug interactions especially with penicillins and NSAIDs dose can be adjusted upward if serum urate remains high
Steven Waller
November 28, 2025 AT 14:14Consider adding Benemid only after evaluating allopurinol response. A gradual approach respects patient autonomy and mitigates adverse events. This measured strategy often yields the most sustainable urate control.
Puspendra Dubey
December 4, 2025 AT 08:54Oh wow, the drama of uric acid! 😱 Benemid swoops in like a hero, yet the villainous kidney stones lurk in the shadows. Hydration becomes your sidekick, battling the crystal villains. Remember, every dose is a plot twist!
Shaquel Jackson
December 10, 2025 AT 03:34Sure, Benemid does its job, but the stone risk feels like a tiny, unnecessary nuisance. 😒
Tom Bon
December 15, 2025 AT 22:14The comparative table succinctly outlines the pharmacologic classes, mechanisms, and side‑effect profiles. Benemid remains a viable uricosuric for select patients requiring cost‑effective therapy. Clinical discretion should guide its utilization.
Clara Walker
December 21, 2025 AT 16:54It’s no coincidence that the push for newer agents aligns with a coordinated agenda to marginalize older, affordable options like Benemid. The collusion between insurers and pharma giants subtly redirects prescribing patterns. Vigilance is essential to preserve therapeutic independence.
Jana Winter
December 27, 2025 AT 11:34The term “uric acid” is a misnomer; the relevant serum component is urate. Precision in language reflects precision in care. Please revise the manuscript accordingly.
Linda Lavender
January 2, 2026 AT 06:14Reading through the Benemid versus newer uric‑lowering agents feels like embarking on an epic odyssey through the annals of rheumatology. From the outset, Benemid’s historic lineage bestows upon it a certain rustic charm, reminiscent of an ancient scholar imparting wisdom in a modern lecture hall. Its mechanism, the inhibition of URAT1, elegantly coaxes the kidneys into expelling excess urate, a process that is both simple and profoundly effective. Yet, this simplicity is a double‑edged sword, for the very act of increasing urinary uric acid precipitates a heightened risk of nephrolithiasis, a complication that demands vigilant prophylaxis. The cost advantage cannot be overstated; while competitors such as febuxostat and pegloticase command premium pricing, Benemid remains a generic staple affordable to the broader populace. Clinical guidelines often relegate it to a secondary role, yet in hands of a knowledgeable clinician, it can serve as a primary agent, especially when xanthine oxidase inhibitors prove intolerable. Hydration emerges as the unsung hero, a preventive measure that, if adhered to, dramatically reduces stone formation, thereby enhancing the drug’s safety profile. Moreover, the drug’s interaction spectrum, notably with penicillins and NSAIDs, necessitates a nuanced prescription strategy to avoid inadvertent toxicity. In populations with preserved renal function, Benemid’s uricosuric effect shines brightest, delivering serum urate reductions comparable to its more expensive counterparts. Conversely, in the setting of chronic kidney disease, its efficacy wanes, and the risk–benefit calculus tilts toward alternatives. The comparative table in the guide succinctly captures these nuances, juxtaposing pros and cons across a spectrum of agents. It is noteworthy that while rasburicase and pegloticase offer rapid urate clearance, their intravenous administration, exorbitant cost, and eligibility criteria restrict their routine use to specialized contexts. The guide’s inclusion of decision algorithms further aids clinicians in navigating this therapeutic labyrinth, encouraging a stepwise escalation from allopurinol to combination therapy, and reserving biologics for refractory cases. Ultimately, the decision to employ Benemid hinges upon a confluence of factors: patient comorbidities, renal function, financial considerations, and personal preferences regarding oral versus intravenous therapy. When these variables align, Benemid can be a cornerstone of gout management, delivering efficacy without the financial burden that often accompanies newer drugs. Therefore, dismissing Benemid outright would be an oversight, whereas a thoughtful integration of its benefits can enhance individualized patient care.
Jay Ram
January 8, 2026 AT 00:54Stay motivated! Managing gout is a marathon, not a sprint-keep hydrated and stay consistent with your meds.
Elizabeth Nicole
January 13, 2026 AT 19:34Exploring the pharmacology of uric‑lowering agents can be daunting, but each piece of knowledge empowers better decisions. Remember that diet and lifestyle are integral companions to any medication regimen. If Benemid is chosen, prioritize water intake and monitor kidney health regularly. Your proactive approach will pay dividends in symptom relief.
Dany Devos
January 19, 2026 AT 14:14The comparative analysis presented adheres to evidence‑based standards and offers a balanced perspective on therapeutic options. Clinicians are encouraged to integrate these insights with individualized patient assessments.