Malabsorption: Causes, Symptoms, and Treatment Options
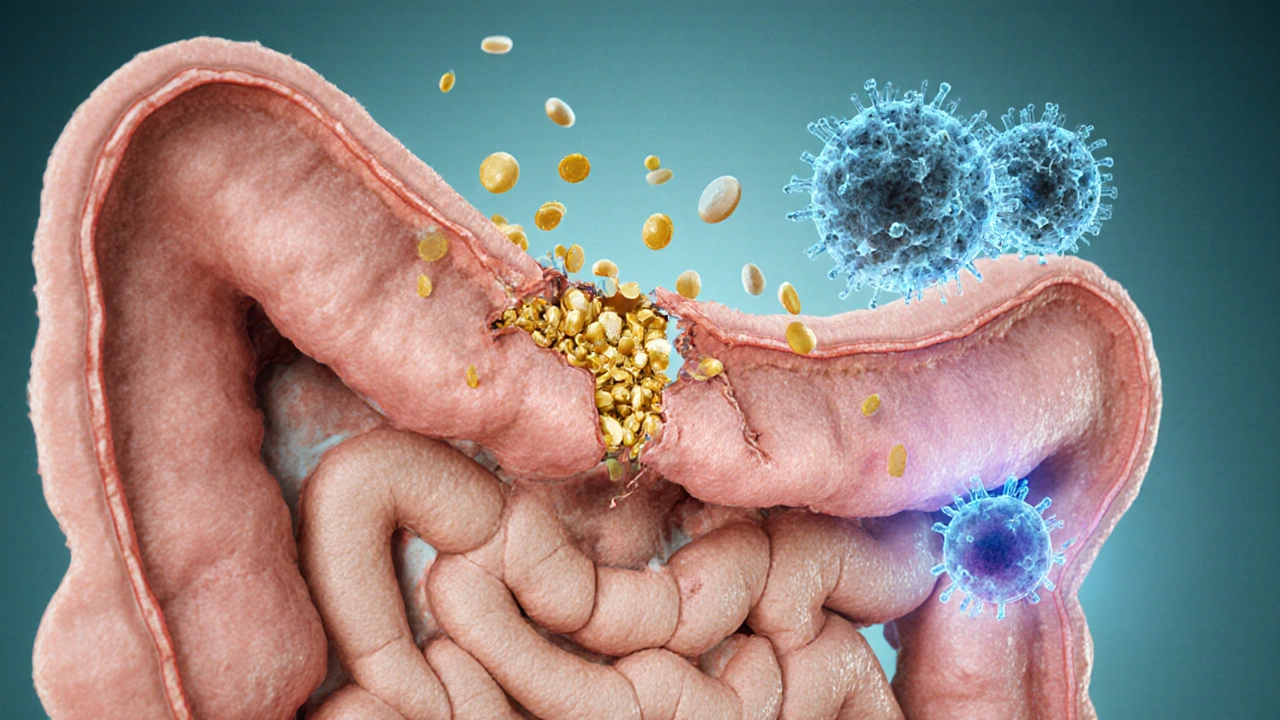
When dealing with malabsorption, the inability of the gut to absorb nutrients properly. Also known as nutrient maldigestion, it can set off a chain of health problems that affect energy, weight, and overall wellbeing. Malabsorption isn’t a disease on its own; it’s a symptom that points to something else not working right in the digestive system.
One of the most common triggers is celiac disease, an autoimmune reaction to gluten that damages the lining of the small intestine. When the villi in the small intestine are flattened, the body can’t pick up vitamins and minerals efficiently, leading to nutrient deficiencies. This connection creates the semantic triple: celiac disease influences malabsorption. If you’ve been diagnosed with celiac, strict gluten avoidance is the first line of defense.
Another often‑overlooked cause is pancreatic insufficiency, a condition where the pancreas fails to release enough digestive enzymes. Without enough enzymes, food isn’t broken down into absorbable units, so even a healthy gut lining can’t do its job. This yields the triple: pancreatic insufficiency requires enzyme replacement. Enzyme supplements can restore digestion and stop the cycle of poor nutrient uptake.
Speaking of enzymes, low levels of digestive enzymes, proteins that break down proteins, fats, and carbohydrates in the stomach and intestines are a direct barrier to absorption. When enzymes are missing, simple carbs may stay whole, proteins stay large, and fats stay greasy, all of which pass through the gut without delivering their nutrients. The link is clear: digestive enzymes enable nutrient absorption. Over‑the‑counter enzyme blends or prescription preparations can fill this gap.
How Malabsorption Shows Up in Your Body
Symptoms can be vague, but there are a few patterns that pop up often. Persistent diarrhea, unexplained weight loss, and chronic fatigue are red flags. You might also notice bloating, gas, or oily stools that look greasy – a sign that fat isn’t being absorbed. Micronutrient shortfalls, like iron‑deficiency anemia or low vitamin D, frequently accompany these signs. Recognizing these clues early helps you and your doctor pinpoint the underlying cause faster.
Testing usually starts with blood work to check for anemia, vitamin levels, and markers of inflammation. If those hint at a problem, doctors may order a stool test for fat content, a breath test for bacterial overgrowth, or imaging to look at the pancreas and small intestine. Endoscopy with a biopsy is the gold standard for confirming celiac disease. Each test is a piece of the puzzle that together explains why malabsorption is happening.
Management strategies depend on the root cause. For celiac disease, a lifelong gluten‑free diet is essential. For pancreatic insufficiency, enzyme replacement taken with every meal is key. In cases of bacterial overgrowth, a short course of antibiotics can reset the gut flora. Nutrient supplements—iron, B12, calcium, vitamin D—are often needed to catch up on what’s been lost.
Lifestyle tweaks also matter. Eating smaller, more frequent meals can give the digestive system a break. Chewing food thoroughly boosts the mechanical breakdown that enzymes later finish. Reducing alcohol intake helps protect the pancreas, and staying hydrated supports overall gut motility.
It’s easy to feel overwhelmed when faced with a term like malabsorption, but breaking it down into causes, symptoms, and actions makes it manageable. The articles below dig deeper into each of these areas—whether you want to learn more about celiac disease, enzyme therapy, or practical diet tips. Keep reading to find the specific guidance that matches your situation and start taking control of your nutrition today.

Poor Nutrient Absorption: Impact on Skin and Hair Health
Learn how poor nutrient absorption shows up on skin and hair, discover key nutrients, gut‑health tips, and when to see a doctor.
How Poor Food Absorption Triggers Autoimmune Disorders
Explore how poor nutrient absorption can trigger autoimmune disorders, learn the key mechanisms, symptoms, testing and gut‑healing strategies.





