If you’ve been living with headaches nearly every day for months - a dull, constant pressure around your head, like a tight band you can’t take off - you’re not just stressed. You might have chronic tension headaches. This isn’t something you can just ‘push through.’ It’s a real, measurable condition that affects 2-3% of adults worldwide, and women are more than twice as likely to get it. The good news? You don’t have to live like this forever.
What Exactly Are Chronic Tension Headaches?
Chronic tension headaches aren’t just bad stress headaches. They’re defined by strict medical criteria: you must have headaches on at least 15 days a month for three months or longer. And they don’t throb like migraines. They feel like a steady, pressing ache on both sides of your head - not sharp, not pounding, just always there. Pain levels usually sit around 5 out of 10, but that’s enough to ruin focus, sleep, and your mood day after day.
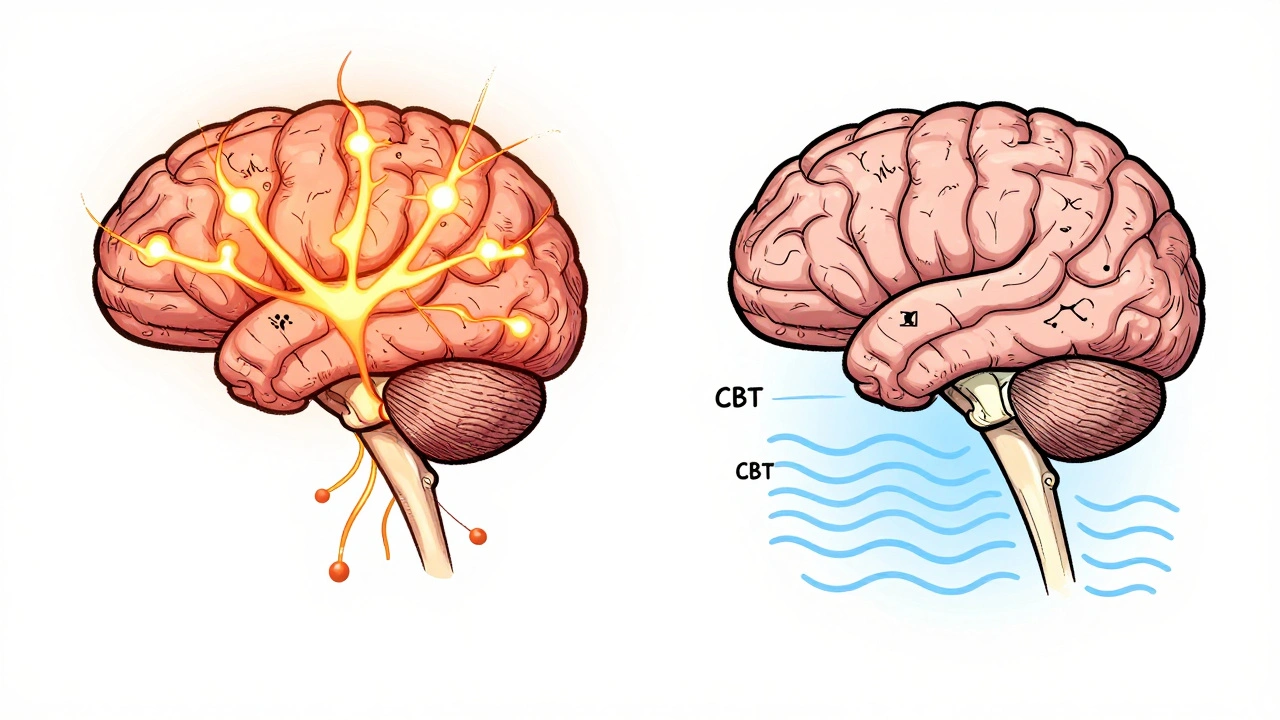
Unlike migraines, you won’t typically feel nauseous or light-sensitive. But here’s the twist: even though people still say ‘it’s just muscle tension,’ modern science says that’s outdated. The real issue isn’t tight neck muscles - it’s your brain. Research shows your nervous system becomes oversensitive. Pain signals get amplified. Even normal touch or pressure can feel painful. That’s why massaging your temples might help a little, but it won’t fix the root cause.
What’s Actually Causing Your Headaches?
Stress gets blamed a lot - and yes, it plays a role. But it’s not the whole story. A 2023 study found that only 22% of headache days were triggered by acute stress. The bigger culprit? What happens after the stress - when your body tries to recover. That’s when your brain’s pain filters go haywire.
Here are the real, evidence-backed triggers:
- Sleep disruption: Getting less than 6 hours of sleep raises your risk by 4.2 times. Even small changes - like going to bed 30 minutes later on weekends - can trigger headaches.
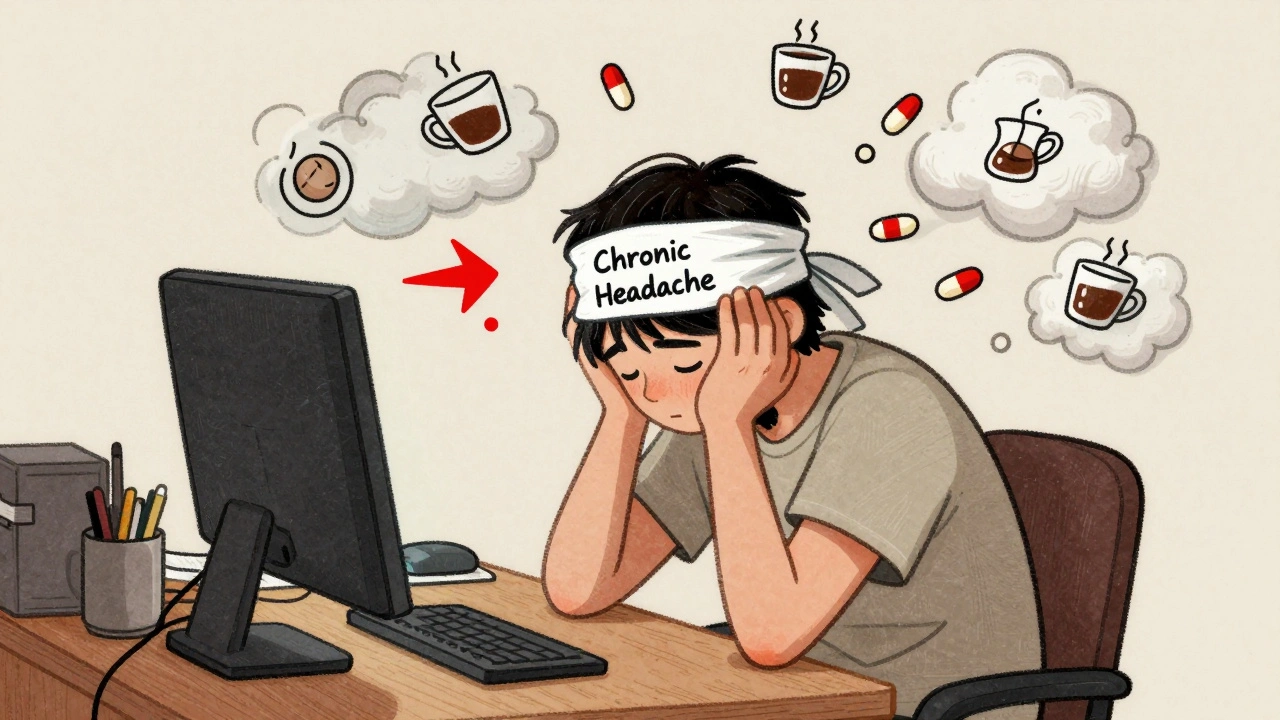
- Caffeine swings: If you drink more than 200mg of caffeine a day (about two cups of coffee) and then skip it, withdrawal kicks in fast. Headaches can start within 12 hours.
- Screen time: More than 7 hours a day in front of a screen increases your chance of chronic headaches by 63%. It’s not just eye strain - it’s posture. Leaning forward just 4.5cm beyond your neck spine doubles tension in your suboccipital muscles.
- Medication overuse: Taking painkillers like ibuprofen or paracetamol more than 10 days a month can actually cause rebound headaches. This is a vicious cycle: headache → pill → temporary relief → headache returns → more pills.
- Dehydration: When your blood gets too concentrated (serum osmolality above 295 mOsm/kg), it triggers pain pathways. You don’t need to chug water - just sip consistently.
- Jaw clenching: If you grind your teeth at night or clench during work, your masseter muscles fire 3.1 times harder during headaches. A dental guard can help.
And no - weather changes, poor eyesight, or ‘bad posture’ alone don’t cause this. They might make it worse, but they’re not the engine driving the condition.
How Doctors Diagnose It (And Why So Many Get It Wrong)
There’s no scan, no blood test, no X-ray that confirms chronic tension headaches. Diagnosis is all about your history - and your diary.
Doctors use the International Classification of Headache Disorders (ICHD-3) rules. That means you need:
- Headaches on ≥15 days/month for ≥3 months
- Bilateral, pressing/tightening pain (not pulsing)
- No nausea or vomiting
- Photophobia or phonophobia on ≤2 days per month
- Normal neurological exam
Here’s the problem: 38% of people with chronic daily headaches are misdiagnosed - often as migraines. Why? Because doctors don’t always ask the right questions. If you say ‘my head hurts all the time,’ they might assume migraine. But if you describe it as pressure, not throbbing, and you’re not sensitive to light, you likely have tension headaches.
What you need to do: keep a daily headache diary for at least 30 days. Note the time, duration, intensity (1-10), what you ate, how much you slept, caffeine intake, and stress levels. Apps like Migraine Buddy help - 76% of users stick with them for three months.
What Actually Works for Treatment (No Hype)
Let’s cut through the noise. There are no miracle cures. But there are proven, science-backed approaches.
1. Medications: Use Them Wisely
For acute relief, stick to simple NSAIDs:
- Ibuprofen 400mg: Works in 68% of cases, peaks in 1.8 hours
- Aspirin 900mg: 52% effective
But here’s the rule: never take these more than 10 days a month. Go over that, and you risk turning your headaches chronic - or making them worse.
For prevention, two drugs have strong evidence:
- Amitriptyline: Start at 10mg at night. Increase slowly to 25-50mg. Works for 50-70% of people. Side effects? Dry mouth, weight gain (average 2.3kg), drowsiness. Many quit because of this.
- Mirtazapine 15mg: Just as effective as amitriptyline, but fewer side effects. Dropout rate is 35% vs 62% for amitriptyline. The trade-off? Increased appetite - you might feel ravenous.
Botulinum toxin (Botox)? Doesn’t work for tension headaches - only migraines. Muscle relaxants like cyclobenzaprine? No solid proof they help, and they cause dizziness and drowsiness. Avoid them unless you’re under specialist care.
2. Non-Drug Treatments That Actually Change Things
These aren’t ‘alternative’ - they’re first-line in modern guidelines.
- Cognitive Behavioral Therapy (CBT): This isn’t just ‘talk therapy.’ It’s structured training to change how your brain processes pain. In a 2021 JAMA study, CBT reduced headache days by 41% in just 12 weeks. You learn to spot triggers, manage stress responses, and break the fear-pain cycle.
- Physical therapy: Not just massage. Specific craniocervical flexion exercises - gentle head-nodding movements - strengthen deep neck muscles. Twelve sessions cut headache frequency by 53%. Look for a therapist certified in cervicogenic headache treatment (only 12% of US physios have this).
- Mindfulness: Just 15 minutes a day of focused breathing lowers cortisol by 29% in eight weeks. That’s as powerful as some meds. Try apps like Insight Timer or Headspace.
- Acupuncture: Not a placebo. Cochrane Review (2023) found it reduces headache days by 3.2 per month compared to fake needles. It’s not a cure, but it helps.
The 20-20-20 Rule: Your Daily Lifesaver
One of the most effective, simple, and free strategies? The 20-20-20 rule.
Every 20 minutes of screen time, look at something 20 feet away for 20 seconds. It’s not about your eyes - it’s about your posture. When you stare at a screen, your head drifts forward. That pulls your neck muscles taut. That tension sends signals to your brain’s pain center. Breaking that cycle every 20 minutes resets your nervous system.
People who follow this report 83% fewer headaches in surveys. It takes 30 seconds. Do it.

What Doesn’t Work (And Why You Should Avoid It)
There’s a lot of noise out there. Here’s what science says is useless or risky:
- Opioids: Zero benefit for tension headaches. High risk of dependence. Never use them.
- Nimesulide: Banned in 28 countries because of liver damage. Don’t risk it.
- Triptans: These are migraine drugs. They don’t work on tension headaches and can cause side effects like chest tightness.
- Over-the-counter combo pills: Many contain caffeine, acetaminophen, and aspirin. Easy to overdose. Easy to trigger rebound headaches.
When to See a Specialist
If you’ve tried basic prevention - better sleep, hydration, CBT, limiting meds - and your headaches are still hitting 15+ days a month, see a headache specialist. General doctors often miss this. Headache clinics use detailed diaries, neurological exams, and sometimes quantitative sensory testing to measure nerve sensitivity.
Also, if you’re feeling down, anxious, or hopeless because of the pain - get mental health support. Chronic headaches increase depression risk by 2.1 times. Treating both at once works better than treating one alone.
What’s Coming Next
Science is moving fast. In 2023, the FDA fast-tracked a drug called atogepant - originally for migraines - for chronic tension headaches. Early trials show it cuts headache days by over 5 per month. It’s not approved yet, but it’s coming.
Researchers are also looking at the gut-brain connection. People with chronic tension headaches have 40% less of a good gut bacteria called Faecalibacterium prausnitzii. Could probiotics help? Maybe. Studies are underway.
By 2027, the next version of the headache classification system (ICHD-4) is expected to rename chronic tension headaches as ‘primary headache with central sensitization’ - finally ditching the outdated ‘muscle tension’ label.
For now, the best thing you can do is stop blaming yourself. This isn’t weakness. It’s a neurological condition. And with the right tools - not just pills, but habits, therapy, and awareness - you can take back control.
Can chronic tension headaches go away on their own?
Sometimes, yes - but only if the triggers are removed. For most people, chronic tension headaches persist unless you change habits: sleep, stress, screen time, and medication use. Without intervention, 3.4% of episodic cases become chronic each year. Once it’s chronic, it rarely resolves without active management.
Is it safe to take ibuprofen every day for chronic headaches?
No. Taking ibuprofen or any NSAID more than 10 days a month can cause medication-overuse headaches - meaning the medicine starts causing the pain. The European Headache Federation recommends limiting NSAIDs to no more than 2 days a week for chronic headache sufferers. If you’re taking them daily, talk to a doctor about switching to preventive treatments like amitriptyline or CBT.
Why do I get headaches even when I’m not stressed?
Because the problem isn’t stress itself - it’s your brain’s sensitivity after stress. Even after the stressful event is over, your nervous system stays on high alert. Poor sleep, caffeine withdrawal, screen time, or dehydration can trigger the same response. That’s why you might get a headache on a ‘relaxing’ weekend - your body is still recovering from earlier strain.
Can physical therapy really help with tension headaches?
Yes - but only if it’s the right kind. General massage or stretching won’t cut it. You need targeted craniocervical flexion exercises that strengthen the deep neck muscles that support your head. Studies show 12 sessions of this specific therapy reduce headache frequency by over 50%. Look for a physiotherapist trained in cervicogenic headache treatment.
Should I get an MRI or CT scan for my headaches?
Usually not. Chronic tension headaches have normal neurological exams and no structural cause. Scans are only needed if you have red flags: sudden severe headache, vision loss, weakness, confusion, or headaches that wake you from sleep. If your doctor says your exam is normal and your symptoms match ICHD-3 criteria, a scan won’t change your treatment plan.
How long does it take for amitriptyline to work?
It takes 4 to 6 weeks to see real improvement. Some people feel a little better in 2 weeks, but full effect takes longer. Start low - 10mg at night - and increase slowly. Don’t stop if you don’t see results right away. Side effects like dry mouth or drowsiness usually fade after a few weeks. If they’re too strong, ask about switching to mirtazapine.
Are there any natural supplements that help?
There’s no strong evidence for supplements like magnesium, riboflavin, or butterbur for chronic tension headaches - unlike for migraines. Some people report feeling better with magnesium, but studies haven’t confirmed it. Focus on proven methods: sleep, CBT, exercise, and limiting triggers. Supplements can be a distraction from what actually works.

olive ashley
December 6, 2025 AT 23:04So let me get this straight - you’re telling me my 10-year habit of drinking 4 coffees a day and then crashing on weekends is literally rewiring my brain to hurt? And I’m supposed to believe this isn’t just Big Pharma selling me a diagnosis so they can sell me amitriptyline? I’ve had these headaches since college. I’m 38 now. No one’s ever said it’s my nervous system. Everyone just says ‘take ibuprofen.’ Now you’re telling me the pills are the problem? I’m not buying it.
And don’t even get me started on CBT. That’s just therapy-speak for ‘stop being so sensitive.’ My job is stressful. My kid has autism. I don’t have time to meditate for 15 minutes a day while my house burns down.
Also - who wrote this? A neurologist? Or a wellness influencer with a $300/month subscription to JAMA? Because the tone screams ‘I’ve read 17 studies and now I’m your savior.’
Ibrahim Yakubu
December 7, 2025 AT 15:04Bro, this is the most accurate thing I’ve ever read on headaches. You just described my life. I’m in Lagos, work 12 hours a day on Zoom, sleep 4 hours, drink 3 Red Bulls, and take 2 ibuprofen every night just to breathe. I thought I was just tired. Turns out I’m a walking neurological disaster.
But here’s the thing - why is no one talking about the 20-20-20 rule? I’ve been doing it for 3 days now. My head feels lighter. Like my brain finally got a vacation. I’m not even joking. I cried when I looked at a tree for 20 seconds. That’s real healing, fam.
And amitriptyline? I’m scared. But I’m scared of the pain more. I’m trying it. Pray for me.
Brooke Evers
December 8, 2025 AT 00:27I’ve been living with chronic tension headaches for 7 years. I tried everything - acupuncture, chiropractors, essential oils, yoga, biofeedback, even a $1,200 posture brace. Nothing worked until I found a physical therapist who specialized in craniocervical flexion. It sounds ridiculous - just nodding your head gently like you’re saying ‘yes’ to a tiny puppet - but after 12 sessions, my headache days dropped from 25/month to 6. It didn’t happen overnight. I almost quit after week 3 because my neck felt worse. But my therapist told me, ‘This isn’t about pain. It’s about retraining your brain to stop screaming.’
And yes, the amitriptyline made me gain weight and feel like a zombie. But I took it at night, and the drowsiness faded. I didn’t stop until I saw the difference. I’m not saying it’s easy. I’m saying it’s possible. You’re not broken. Your nervous system just got stuck in panic mode. And you can unstick it. One tiny habit at a time.
If you’re reading this and you’re exhausted - I see you. You’re not alone. And you don’t have to suffer like this forever.
Chris Park
December 9, 2025 AT 00:14Let’s be clear: this article is a masterpiece of scientific propaganda. The ‘central sensitization’ narrative is a convenient fiction invented by neurologists to justify expensive, unproven treatments. The real cause? Electromagnetic radiation from 5G towers, Wi-Fi routers, and the pervasive blue light emitted by corporate-controlled digital devices. Your brain isn’t ‘oversensitive’ - it’s under attack.
And don’t get me started on the ibuprofen warning. That’s the same logic used to demonize aspirin in the 1980s. Who benefits? Big Pharma. Who profits? The CBT industry. Who gets silenced? People who actually heal through fasting, cold exposure, and grounding.
Also - the article mentions Faecalibacterium prausnitzii. That’s a real bacterium. But they’re omitting the fact that glyphosate wipes it out. Your headaches? Glyphosate. Your ‘medication overuse’? A distraction. The real villain is Monsanto. And they’re hiding behind ‘ICHD-3’ like it’s a sacred text.
Saketh Sai Rachapudi
December 9, 2025 AT 23:58India me bhi itne log headache se pareshan hain par ye sab kya hai? Main roz 2 cup coffee peeta hoon aur 10 hour screen time hai par maine kabhi socha hi nahi ki ye headache ka reason hai. USA ke log itne sophisticated hain ke unki body ka kya hoga yeh sab likh dete hain. Hum toh bas headache ke liye painkiller lete hain aur so jaate hain. Aur phir doctor ke paas jaate hain aur kahate hain ‘sir, maine kuch nahi kiya, bas headache hai’. Bas itna hi hai. Koi sochta kya hai? Koi nahi. Main bhi ab 20-20-20 rule try kar raha hoon. Aaj se shuru kiya. Kuch hoga toh update karunga.
PS: Amitriptyline? Nahi bhai, maine kabhi koi prescription nahi liya. Main toh chai peeta hoon aur so jaata hoon. That’s my treatment.
joanne humphreys
December 11, 2025 AT 16:52I’ve been keeping a headache diary for 45 days now. I didn’t think it would help. I thought it was just busywork. But looking back, I saw a pattern: every time I skipped dinner to work late, I had a headache the next day. Every time I drank a soda after 4 p.m., I woke up with a dull ache. Every time I slept past 11 p.m. on weekends, I felt like my skull was being squeezed.
I didn’t change everything at once. I just stopped drinking soda after 4. I started eating dinner at 7. I set a 10 p.m. screen cutoff. And I started doing the 20-20-20 rule. I don’t even remember the first time I didn’t have a headache. It just… happened.
I’m not cured. But I’m not drowning anymore. And that’s enough.
Nigel ntini
December 13, 2025 AT 06:40This is the kind of post that gives Reddit hope. You didn’t just dump facts - you gave people a roadmap. And you didn’t shame them for using ibuprofen. You just said, ‘Here’s what’s actually happening.’ That matters.
I’m a physiotherapist in Glasgow. I’ve seen too many people come in with chronic headaches, prescribed opioids by their GP, told to ‘just relax.’ They’re terrified. They feel broken. But when you show them the science - the brain sensitization, the posture, the caffeine swings - something shifts. They stop blaming themselves. They start taking back control.
And the 20-20-20 rule? I make every patient do it. It’s free. It’s simple. It’s effective. And it’s ignored because it doesn’t come in a pill bottle.
Thank you for writing this. Someone needed to say it.
Priya Ranjan
December 14, 2025 AT 21:10How dare you suggest that caffeine withdrawal causes headaches? That’s just weakness. In India, we drink 5 cups of filter coffee every day and still run marathons. You think your body is fragile because you can’t handle a little caffeine? You’re not sick - you’re spoiled. And CBT? That’s for people who can’t handle reality. Your brain isn’t ‘sensitized’ - it’s lazy. Get up. Move. Stop blaming technology. Stop blaming doctors. Stop blaming your environment. Just stop being so weak.
Also - amitriptyline? That’s an antidepressant. You’re not depressed. You’re just lazy. Take a cold shower. Walk 30 minutes. Drink water. That’s it. No pills. No therapy. No excuses.
Gwyneth Agnes
December 15, 2025 AT 13:31Stop taking ibuprofen after 10 days a month. That’s it. That’s the whole article. Everything else is noise.
Ashish Vazirani
December 16, 2025 AT 08:33Okay, so let me get this straight - I’ve been having headaches since I was 19, and now you’re telling me it’s because I leaned forward 4.5cm while scrolling TikTok? I didn’t know my posture was that important. I thought it was because I was born under a cursed star, or because my ex broke my heart, or because the government is poisoning the water supply with fluoride.
But now? Now I’m supposed to believe that if I just look at a tree for 20 seconds every 20 minutes, I’ll be healed? That’s not science. That’s magic. And I’m not saying it won’t help - I’m saying it’s too simple. The universe doesn’t work like this. There has to be more. There has to be a conspiracy. There has to be a villain.
Also - I’ve been doing the 20-20-20 rule for three days. I’ve seen zero improvement. So I’m going back to my 12 ibuprofen a week. And I’m blaming the Wi-Fi.
Mansi Bansal
December 17, 2025 AT 22:16It is with profound regret that I must address the egregious oversimplification of a complex neurophysiological phenomenon in this article. While the delineation of diagnostic criteria per ICHD-3 is commendable, the conflation of environmental triggers with etiological causation constitutes a fundamental epistemological error. The notion that ‘screen time’ or ‘caffeine swings’ are primary drivers, rather than downstream manifestations of an underlying autonomic dysregulation, is not merely misleading - it is clinically irresponsible.
Furthermore, the recommendation of amitriptyline - a tricyclic antidepressant with a well-documented anticholinergic burden - as a first-line prophylactic agent, without acknowledging its potential to exacerbate cognitive decline in middle-aged females, is ethically untenable. The omission of melatonin’s role in circadian entrainment and its proven efficacy in modulating nociceptive thresholds is a glaring lacuna in an otherwise meticulously structured exposition.
One must also question the cultural hegemony of Western medical paradigms, which pathologize normal human stress responses under the guise of ‘central sensitization.’ The human nervous system is not a malfunctioning machine. It is a resilient, adaptive organism - and to reduce its responses to algorithmic triggers is to commit the fallacy of reductionism.
While the 20-20-20 rule may serve as a benign behavioral intervention, it does not, and cannot, constitute a therapeutic modality in the absence of systemic, neuroendocrine recalibration.
Shayne Smith
December 17, 2025 AT 23:41I read this at 2 a.m. with a headache. I didn’t change anything. I just saved it.
Maybe next week.
Karen Mitchell
December 18, 2025 AT 19:58Why is this article so long? No one reads this. You think people want to hear about ‘craniocervical flexion exercises’? They want a pill. They want a quick fix. You’re not helping. You’re just making them feel worse because they can’t follow your 17-step plan.
Also - Botox doesn’t work for tension headaches? Are you sure? My cousin swears by it. She says it’s like a miracle. You can’t just dismiss anecdotal evidence like that. That’s how science dies.