Lifestyle Changes for Better Health: What Actually Works
When you hear lifestyle changes, practical, daily habits that improve health outcomes without relying solely on medication. Also known as behavioral health interventions, it’s not about extreme diets or punishing workouts—it’s about small, repeatable actions that add up over time. Many people think changing how they live means overhauling everything at once. But the truth? The most lasting changes are the ones that fit into your real life—like taking your blood pressure pill after brushing your teeth, or walking for 10 minutes after dinner because it’s easy and you already do it.
medication adherence, how consistently someone takes their prescribed drugs isn’t just about remembering pills. It’s tied to sleep, stress, food, and routine. If you’re on statins like pravastatin and skipping doses because you feel fine, or if you’re avoiding your diabetes meds because they make you nauseous, that’s not noncompliance—it’s a sign your current plan doesn’t match your life. That’s where diet and exercise, daily habits that directly affect how well drugs work and how your body responds come in. A person with high potassium from ACE inhibitors and diuretics might not need a new drug—they might need to eat fewer bananas and reduce salt. Someone with early-stage COPD doesn’t need to run a marathon—they need to walk daily while using a spacer correctly. These aren’t side notes. They’re part of the treatment.
chronic disease management, the ongoing process of controlling long-term health conditions through daily choices and medical support is rarely about one magic pill. It’s about stacking small wins: eating protein with your morning meds to reduce stomach upset, using secure messaging to ask your pharmacist about a new supplement, or getting your child’s vision checked before age five to prevent lifelong issues. The posts below show how people are doing this—without gimmicks, without hype. You’ll see how peanut allergy prevention works by introducing tiny amounts early, how GLP-1 agonists help with weight loss but still require movement and better sleep, and why using the wrong steroid cream for athlete’s foot can make it worse. These aren’t theoretical ideas. They’re real strategies people use every day to take back control.
What you’ll find here isn’t a checklist of things to do. It’s a collection of real-world examples showing how lifestyle changes connect to the medicines you take, the tests you get, and the decisions you make. Whether you’re managing liver disease with acetaminophen, balancing hormones while on warfarin, or trying to stick to a complex pill schedule, the answers aren’t always in a prescription. Sometimes, they’re in how you start your day, what you eat at lunch, or whether you ask your pharmacist a simple question. The tools are simple. The impact? Life-changing.
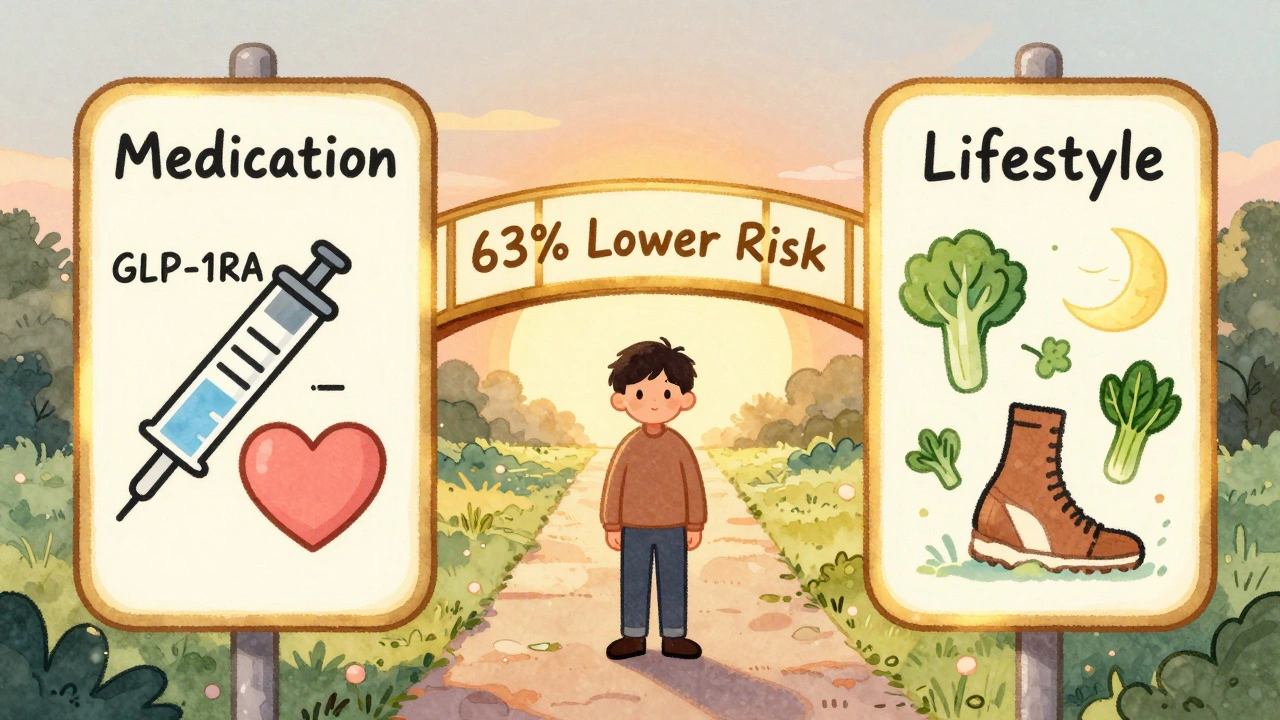
Diabetes and Heart Disease: How Medications and Lifestyle Together Lower Risk
Diabetes greatly increases heart disease risk, but combining GLP-1 RA medications like semaglutide with lifestyle changes-diet, exercise, and weight loss-can cut cardiovascular risk by up to 63%. This is the most effective strategy proven today.





