When you have type 2 diabetes, your risk for heart disease isn’t just higher-it’s devastatingly high. About 65% of people with diabetes die from heart-related causes, according to the American Heart Association. That’s not a coincidence. High blood sugar damages blood vessels over time, pushes up blood pressure, and fuels inflammation-all of which strain your heart. But here’s the good news: you don’t have to accept that fate. The most powerful way to cut your risk isn’t just one thing-it’s two things working together: modern medications and real lifestyle changes.
Why Diabetes and Heart Disease Are Linked
Diabetes doesn’t just mean high blood sugar. It means your body’s whole metabolic system is out of balance. Insulin resistance leads to fat buildup around organs, including the heart. Your arteries stiffen. Cholesterol levels go haywire. Blood pressure climbs. All of this sets the stage for heart attacks, strokes, and heart failure. The 2017 ACC/AHA guidelines made it official: diabetes is now classified as a major risk factor for cardiovascular disease, just like smoking or high cholesterol. You don’t need to wait for symptoms. If you have diabetes, you’re already in the high-risk group.How GLP-1 RAs Are Changing the Game
For years, metformin was the go-to drug for diabetes. It helps with blood sugar, but its heart benefits are modest. That changed with the rise of GLP-1 receptor agonists-medications like semaglutide (Wegovy, Ozempic) and tirzepatide (Mounjaro, Zepbound). These aren’t just diabetes drugs anymore. They’re heart protectors. Semaglutide, at the 2.4 mg weekly dose, helps people lose nearly 15% of their body weight on average. Tirzepatide? Up to 22.5%. That kind of weight loss doesn’t just improve how you look-it rewires your metabolism. It lowers blood pressure, reduces liver fat, improves insulin sensitivity, and cuts inflammation. In the LEADER trial, liraglutide (another GLP-1 RA) lowered major heart events by 13%. But the real breakthrough came in 2023, when the FDA approved Wegovy specifically to reduce heart attack, stroke, and cardiovascular death in people with obesity or overweight and existing heart disease. This was the first time a weight-loss drug got a cardiovascular approval.What Lifestyle Changes Actually Work
Medications do a lot-but they don’t fix everything. Lifestyle changes bring benefits drugs can’t replicate: better sleep, lower stress, stronger social ties, and improved mental health. The American Diabetes Association doesn’t push one single diet. Instead, it recommends patterns that work: Mediterranean, DASH, or plant-based eating. That means more vegetables, beans, nuts, whole grains, fish, and olive oil. Less processed food, sugar, and saturated fat. Exercise isn’t optional. The CDC and ADA agree: aim for at least 150 minutes a week of moderate activity-like brisk walking, cycling, or swimming. You don’t need to do it all at once. Three 10-minute walks a day count. Strength training twice a week helps too. Blood pressure goals? Below 130/80 mm Hg. Weight loss target? Seven percent of your body weight. That’s not about being thin-it’s about breaking the cycle of metabolic damage.
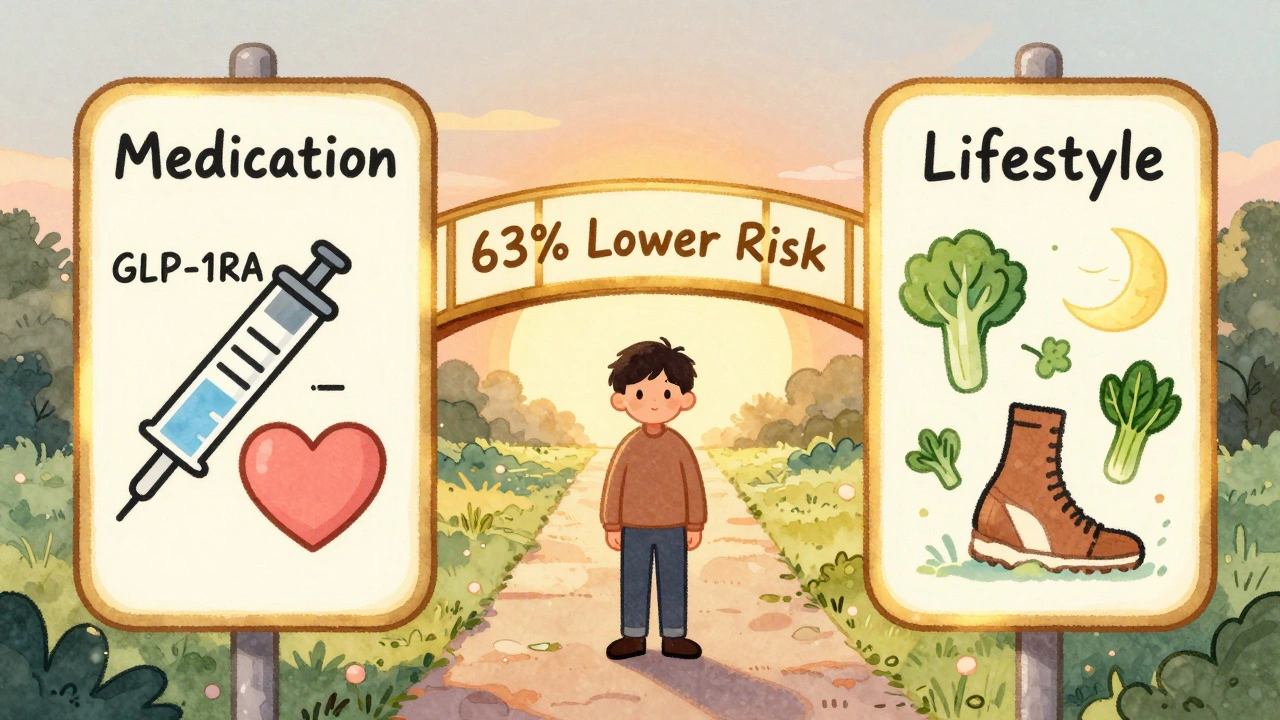
The Magic Is in the Combination
Here’s the truth: taking a GLP-1 RA alone is better than nothing. But combining it with healthy habits? That’s when things get powerful. A study of veterans with type 2 diabetes showed those on GLP-1 RAs had a 20% lower risk of heart events. But those who also followed eight heart-healthy habits-eating well, moving daily, not smoking, managing stress, sleeping enough, limiting alcohol, maintaining social connections, and keeping weight down-cut their risk by 63%. That’s not additive. That’s multiplicative. The Look AHEAD trial showed that even with 7% weight loss through diet and exercise, heart attacks didn’t drop significantly. But when you add a GLP-1 RA to that same lifestyle change? The risk plummets. Why? Because medications tackle the biological barriers-insulin resistance, fat storage, appetite signals-that make lifestyle changes so hard to stick with. Lifestyle, in turn, supports the medication by reducing inflammation, improving sleep, and lowering stress hormones that spike blood sugar.Why Doctors Are Changing Their Minds
Ten years ago, the rule was: try diet and exercise for six months. If that didn’t work, then consider meds. Now? The American College of Cardiology’s June 2025 guidance says: Don’t make patients fail before helping them. Obesity is a chronic disease. You wouldn’t wait six months to treat high blood pressure with meds. Why treat obesity differently? GLP-1 RAs are now seen as first-line options for people with diabetes and overweight or obesity-even if they haven’t tried lifestyle changes yet. But here’s the catch: the FDA still requires that Wegovy be used in addition to a reduced-calorie diet and increased physical activity. The medicine doesn’t replace the lifestyle. It enables it.
What’s Holding People Back
The science is clear. The tools exist. But access is still a problem. Insurance often won’t cover these drugs unless you’ve tried other treatments first. Even when covered, copays can hit $1,000 a month. Only about 2% of eligible patients are currently prescribed these medications. That’s not because they’re ineffective-it’s because the system hasn’t caught up. And cost isn’t the only barrier. Many people don’t know these drugs exist. Others fear injections. Some think lifestyle changes are enough. But research shows: if you’re at high risk, waiting to lose weight on your own is risky. The SELECT trial showed semaglutide reduced heart events by 20% even in people without diabetes-just because they had obesity and heart disease. That’s a game-changer.What You Can Do Right Now
If you have diabetes and are worried about your heart:- Ask your doctor about GLP-1 RAs like semaglutide or tirzepatide. Don’t wait for them to bring it up.
- Start small with movement. Walk 10 minutes after meals. That’s more effective than one long walk once a week.
- Swap one processed snack for a handful of nuts or an apple. Don’t overhaul your whole diet overnight.
- Track your blood pressure at home. Write it down. Bring it to appointments.
- Focus on sleep and stress. Poor sleep raises cortisol, which raises blood sugar. Meditation, deep breathing, or even a nightly walk can help.
The Future Is Integrated
By 2030, experts predict GLP-1 RAs will be standard care for people with diabetes and heart risk. But they won’t replace lifestyle-they’ll empower it. The next wave of drugs will target multiple pathways at once. Eli Lilly’s tirzepatide already does that, hitting both GLP-1 and GIP receptors for even stronger results. The real win isn’t just living longer. It’s living better-without chest pain, without shortness of breath, without fear. You don’t have to choose between pills and willpower. You can have both. And together, they’re the most effective shield against heart disease you’ve ever had.Can I just take the medication and skip lifestyle changes?
No. While GLP-1 RAs like semaglutide and tirzepatide significantly reduce heart risk, they work best when paired with healthy eating and regular movement. The FDA requires these medications to be used alongside diet and exercise. Lifestyle changes improve sleep, reduce stress, and lower inflammation in ways drugs can’t. Combining both cuts your risk up to 63%-far more than either alone.
Are GLP-1 RAs only for people with diabetes?
No. The FDA approved Wegovy (semaglutide) in 2023 specifically for reducing heart attack, stroke, and cardiovascular death in adults with overweight or obesity and existing heart disease-even if they don’t have diabetes. The SELECT trial showed clear benefits in this group. These drugs aren’t just for blood sugar-they’re for heart protection.
How much weight do I need to lose to see heart benefits?
Losing just 7% of your body weight-like 15 pounds if you weigh 215-can improve blood pressure, cholesterol, and insulin sensitivity. But GLP-1 RAs often help people lose 10-22% of their weight, which leads to even stronger results. The key isn’t perfection-it’s progress. Even small, sustained weight loss reduces strain on your heart and blood vessels.
What’s the best diet for lowering heart risk with diabetes?
There’s no single “best” diet, but the most proven patterns are Mediterranean, DASH, and plant-based diets. Focus on vegetables, legumes, whole grains, nuts, fish, and healthy fats like olive oil. Cut back on added sugar, processed meats, fried foods, and refined carbs. You don’t need to go vegan or keto-just make smarter swaps. One study showed people who followed these patterns lowered their heart risk by up to 30%.
Is exercise really as effective as medication for heart health?
Yes, in some ways. Studies show that structured exercise programs can reduce mortality after a heart attack by 27%-similar to the benefit seen with certain heart medications. Exercise improves circulation, lowers blood pressure, and reduces inflammation. But for people with diabetes and obesity, combining exercise with a GLP-1 RA gives the strongest protection. Think of exercise as a powerful tool-and medication as the force multiplier.






patrick sui
December 2, 2025 AT 10:34GLP-1 RAs are a game-changer, no cap. The fact that semaglutide got FDA approval specifically for CVD reduction in non-diabetics with obesity? That’s massive. 🤯 We’ve been treating diabetes like it’s just a sugar problem, but it’s a full-system metabolic meltdown. These drugs don’t just lower glucose-they rewire fat storage, inflammation, and even appetite signaling. It’s not magic, it’s molecular biology. And yes, lifestyle still matters, but now we’ve got tools that make lifestyle actually doable. #DiabetesIsNotAPersonalFailure
Declan O Reilly
December 2, 2025 AT 19:11man i read this whole thing and im just like… why did we wait so long? i mean seriously. we knew insulin resistance was bad, we knew obesity was bad, but we kept acting like the solution was just ‘eat less, move more’ like its 1998. glp-1 ras arent a crutch, they’re a bridge. and the fact that the ada and acc still make you ‘try lifestyle first’ is honestly criminal. if you had high bp youd get meds on day one. why is obesity treated like a moral failing? 🤦♂️
Conor Forde
December 3, 2025 AT 18:56Oh wow. Another ‘meds are the answer’ fairy tale. Let me guess-next you’ll tell me we should inject insulin into our cats to fix their obesity too? 😏 You people treat these drugs like they’re the holy grail, but the real story? They’re expensive, hard to access, and come with side effects that make you feel like a zombie who lost a fight with a blender. And don’t get me started on the ‘8 heart-healthy habits’-who has time for that? I’ve got a job, a kid, and a Netflix queue longer than my life expectancy. Let’s be real: this is just Big Pharma repackaging weight loss as heart disease prevention. Again.
Souvik Datta
December 5, 2025 AT 02:29This is one of the most balanced and scientifically grounded pieces I’ve read on diabetes and cardiovascular risk in years. The synergy between pharmacotherapy and lifestyle isn’t just additive-it’s exponential. I’ve seen patients on tirzepatide lose 20% of their body weight and finally sleep through the night, stop snoring, and walk without knee pain. But here’s the thing: the real win isn’t the scale. It’s the dignity. When someone stops feeling like their body is betraying them, they start taking care of themselves-not because they’re told to, but because they feel capable again. That’s the hidden benefit of these drugs: they restore agency.
Priyam Tomar
December 5, 2025 AT 03:57Everyone’s acting like GLP-1 RAs are some miracle cure, but let’s be honest-this is just a fancy way of saying ‘take a drug so you don’t have to change your life.’ Meanwhile, people in India and Africa have been managing type 2 diabetes for decades with nothing but diet, walking, and rice portions. You don’t need a $1000/month injection to live longer. You need discipline. And if you can’t manage that, maybe your problem isn’t your biology-it’s your laziness. The system is rewarding weakness, not strength.
Jack Arscott
December 5, 2025 AT 12:07Just read this. Wow. 🙌 I’ve been on semaglutide for 6 months and honestly? My blood pressure dropped 20 points. I started walking after dinner because I didn’t feel like puking anymore. 🍎🚶♂️ The meds didn’t fix me, but they gave me the energy to fix myself. Also, the FDA’s new guidance? Long overdue. 💯
Irving Steinberg
December 6, 2025 AT 01:14Lydia Zhang
December 6, 2025 AT 17:19Kay Lam
December 8, 2025 AT 13:57I’ve been working with patients with type 2 diabetes for over 15 years and I can tell you this: the most transformative thing I’ve seen isn’t the medication-it’s the moment someone stops believing they’re broken. GLP-1 RAs don’t cure diabetes, but they do something more important: they give people a fighting chance. When you’re constantly told you lack willpower, and then you take a drug that actually reduces your cravings and makes movement feel possible, it changes your entire relationship with your body. It’s not about losing weight-it’s about reclaiming your life. And yes, it’s not perfect. Insurance denials, cost barriers, stigma-it’s all real. But if we can get even half the people who need this access to it, we could prevent tens of thousands of heart attacks. This isn’t hype. This is survival.
Declan Flynn Fitness
December 10, 2025 AT 02:56Just wanted to add something real quick-walking after meals? 10 minutes? That’s the secret sauce. I’ve had clients who couldn’t run a mile but did 3 x 10-min walks after breakfast, lunch, and dinner. Within 6 weeks, their fasting glucose dropped 30 points. No meds needed. But if you’re on a GLP-1 RA? Do it anyway. It’s like turbocharging a hybrid. The drug lowers the barrier, the movement builds the habit. And habits stick. That’s how you live longer-not because you’re perfect, but because you’re consistent. Keep it simple. Walk. Breathe. Eat real food. And if you’re on a med? Thank the scientists who made it possible.