Genetic Kidney Disease: Causes, Symptoms, and What You Need to Know
When genetic kidney disease, a group of inherited disorders that damage kidney function over time. Also known as hereditary nephropathy, it doesn’t come from lifestyle choices—it’s in your DNA. Unlike kidney damage from high blood pressure or diabetes, this type starts long before symptoms show. It can sneak up in childhood, strike in your 30s, or quietly worsen as you age—often without warning.
Two of the most common forms are polycystic kidney disease, a condition where fluid-filled cysts grow in the kidneys and slowly replace healthy tissue and Alport syndrome, a genetic disorder that affects the filtering units of the kidney and often leads to hearing loss and vision problems. These aren’t rare outliers. Polycystic kidney disease affects about 1 in 500 people worldwide. Alport syndrome is less common but just as serious, especially when diagnosed late. Both can lead to kidney failure, and both run in families. If a parent has it, you have a 50% chance of inheriting the faulty gene.
What makes genetic kidney disease tricky is that it often looks like other kidney problems. Fatigue, swelling in the legs, high blood pressure, or blood in the urine—these signs get blamed on aging, diet, or stress. But if they show up early, or if multiple family members have kidney issues, it’s not just bad luck. Genetic testing can confirm it. And knowing your risk changes everything: earlier monitoring, smarter medication choices, and avoiding drugs that hurt the kidneys—like NSAIDs or certain antibiotics.
Some of the treatments you’ll see in the articles below aren’t about curing it—they’re about slowing it down. ACE inhibitors, for example, are often prescribed not just for blood pressure, but because they reduce protein leakage in the kidneys, a key sign of damage. Potassium levels matter too—high potassium can be dangerous when kidneys are failing, which is why drug interactions with diuretics or supplements need careful tracking. Even something as simple as staying hydrated or avoiding dehydration during illness can make a real difference in how fast the disease progresses.
You won’t find a magic pill here. But you will find real, practical advice from people who’ve lived with this. From how to talk to your doctor about genetic testing, to what blood tests actually mean, to how to spot early signs before it’s too late. The articles below cover what works, what doesn’t, and what’s often overlooked—like the hidden risks of common OTC meds or how to manage kidney health alongside other conditions like diabetes or heart disease. This isn’t theory. It’s what people are using right now to protect their kidneys and their lives.
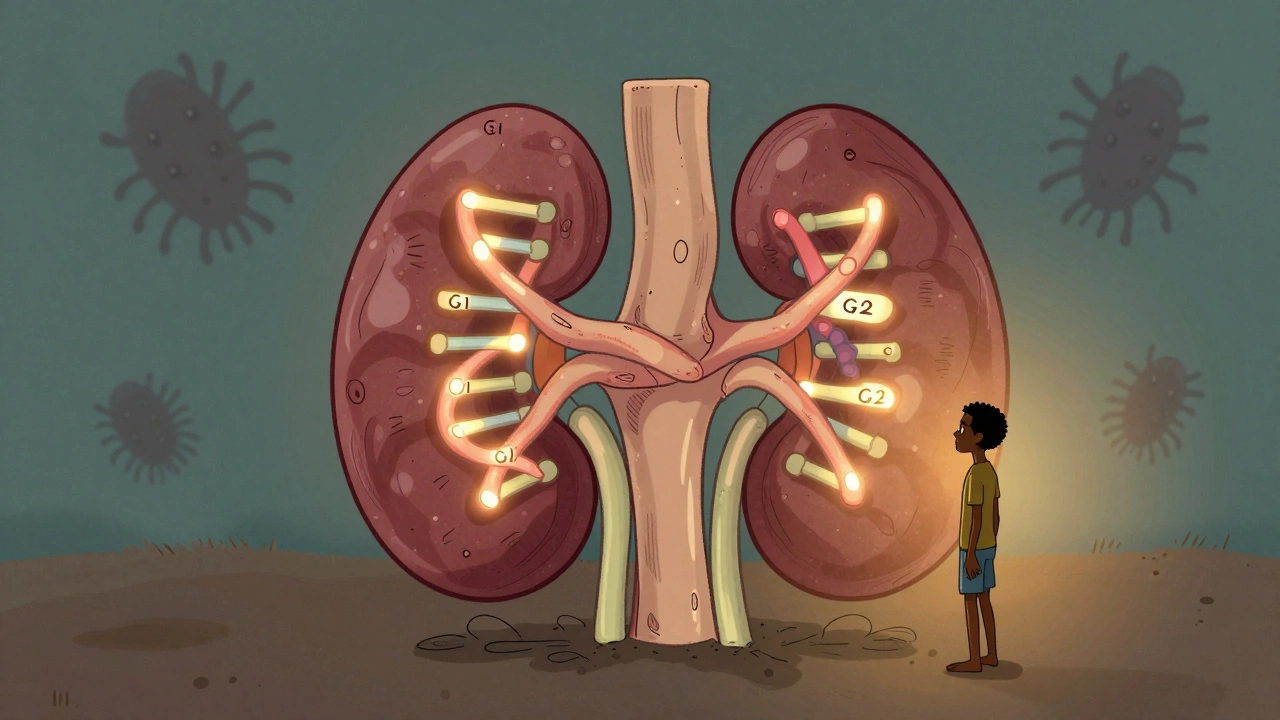
APOL1 Genetic Risk: Understanding Kidney Disease in African Ancestry
APOL1 genetic variants explain most of the higher kidney disease risk in people with African ancestry. Learn how these genes work, who should be tested, and what steps can protect kidney health.





