Understanding CP/CPPS: Chronic Prostatitis and Pelvic Pain
When dealing with CP/CPPS, a long‑lasting inflammation of the prostate and surrounding pelvic structures that causes persistent pain and urinary issues. Also known as Chronic Prostatitis/Chronic Pelvic Pain Syndrome, it affects many men and often goes undiagnosed because its symptoms overlap with other urological problems.
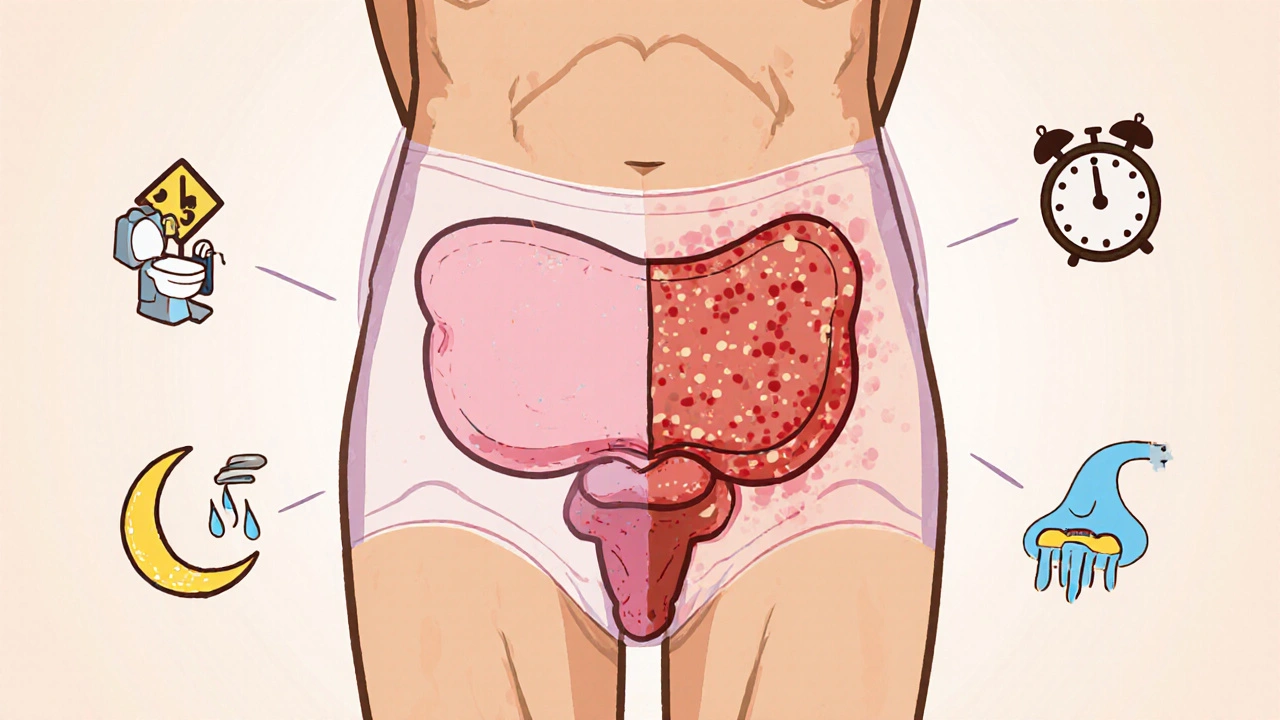
The prostate, a walnut‑sized gland sitting just below the bladder, plays a central role in CP/CPPS. When the prostate tissue becomes inflamed or irritated, it can trigger a cascade of nerve signals that radiate across the pelvic region. This makes prostate health a key factor in both the onset and persistence of symptoms.
Equally important is the pelvic floor, a network of muscles that support the bladder, rectum, and prostate. Tight or weak pelvic floor muscles often amplify pain signals, turning a mild discomfort into chronic pelvic pain. Strengthening or relaxing these muscles through targeted therapy can dramatically change a patient’s experience.
CP/CPPS often shows up as urinary urgency, frequent nighttime trips to the bathroom, or a burning sensation during urination. These urinary symptoms are not random; they stem from inflammation that irritates the bladder neck and urethra. Recognizing this link helps clinicians choose tests that focus on the lower urinary tract rather than searching for unrelated causes.
Another related entity is chronic prostatitis, which describes the same underlying inflammation but without a clear bacterial infection. This condition blurs the line between infection‑driven and non‑infectious pain, meaning treatment often needs a hybrid approach.
Antibiotic therapy is frequently tried first because some cases hide low‑grade bacterial infections. When antibiotics fail, doctors may shift to anti‑inflammatories, alpha‑blockers, or neuromodulators. The treatment plan therefore requires flexibility and a willingness to combine medications with physical therapy.
Lifestyle factors such as caffeine intake, alcohol consumption, and prolonged sitting can aggravate CP/CPPS. Simple changes—limiting spicy foods, staying hydrated, and taking short walks every hour—reduce pelvic congestion and ease muscle tension. Patients who adopt these habits often report a noticeable drop in pain intensity.
Diagnosis usually starts with a detailed questionnaire, followed by a digital rectal exam to assess prostate tenderness. Some clinicians add urine cultures, blood tests for inflammatory markers, and, if needed, imaging like transrectal ultrasound. Each step narrows down the possible triggers, guiding a more precise therapy.
Effective management of CP/CPPS hinges on a multi‑modal strategy: targeted antibiotics when needed, muscle‑relaxing physiotherapy for the pelvic floor, anti‑inflammatory medication, and lifestyle tweaks. By addressing the prostate, the pelvic floor, and the nervous system together, patients can break the cycle of chronic pain.
Below you’ll find a curated list of articles that dive deeper into each of these areas—everything from antibiotic comparisons to pelvic floor exercises, plus practical tips for everyday symptom relief. Explore the resources and start building a plan that works for you.
How Enlarged Prostate and Chronic Prostatitis Are Linked
Explore how an enlarged prostate and chronic prostatitis are linked, covering causes, symptoms, diagnosis, and effective management options.





