BPH & Prostatitis Symptom Assessment Tool
Select Your Symptoms
This tool helps you understand which symptoms are most associated with each condition based on the article content. It is for educational purposes only and not a diagnostic tool.
Frequent nighttime trips to the bathroom
Common in enlarged prostate (BPH) but can occur in prostatitis
Weak or interrupted urine stream
Primary symptom of enlarged prostate
Pelvic or lower back pain
Typical of chronic prostatitis
Burning during urination
Common in chronic prostatitis
Painful ejaculation
Specific to chronic prostatitis
Feeling of incomplete emptying
Typical of enlarged prostate
Urinary urgency
Can occur in both conditions
Difficulty starting urination
Common in enlarged prostate
When the prostate grows larger, it’s called Enlarged prostate a non‑cancerous expansion of the prostate gland that often leads to urinary trouble. Many men also experience Chronic prostatitis persistent inflammation of the prostate that can cause pelvic pain and urinary issues. At first glance they seem like separate problems, but research shows they often overlap. Understanding that overlap helps you spot warning signs early and choose the right treatment.
What is an enlarged prostate?
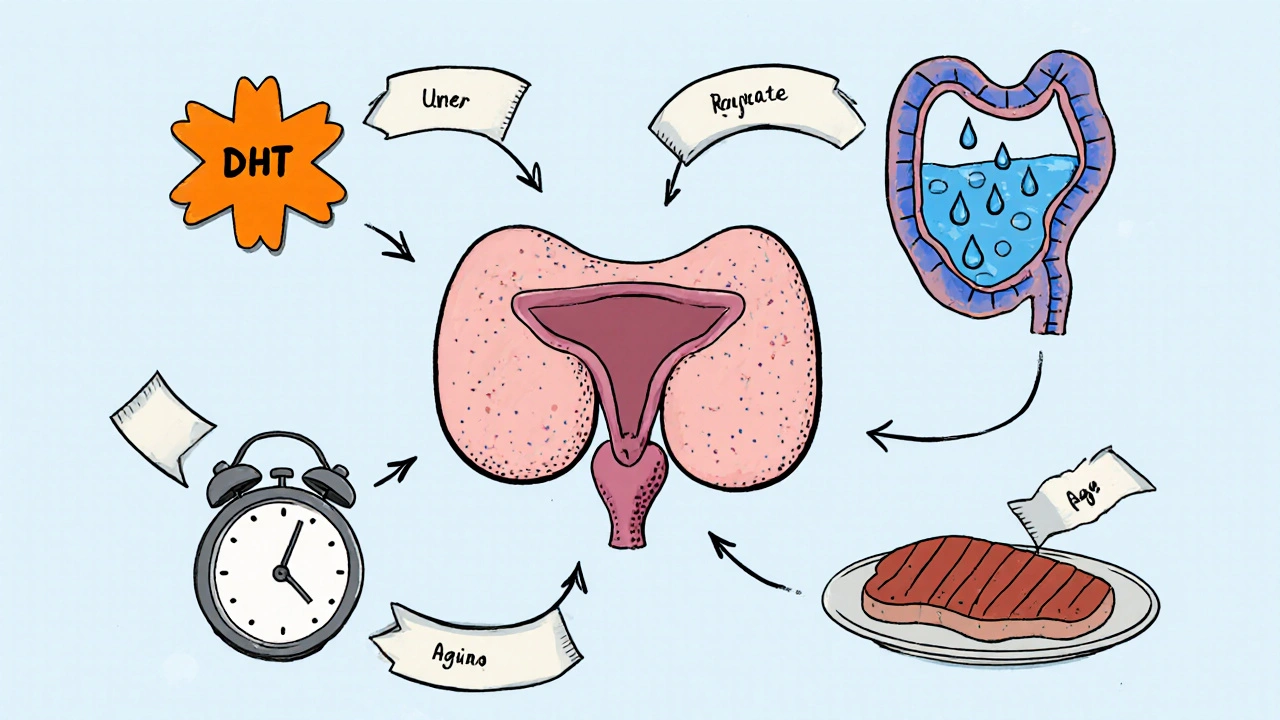
The medical term for an enlarged prostate is Benign Prostatic Hyperplasia a common age‑related condition where the prostate tissue multiplies, pressing on the urethra. It typically appears after age 50, and the risk rises sharply in the 60s and 70s. Hormones, especially Dihydrotestosterone (DHT) a potent androgen that drives prostate cell growth, are the main drivers. As the gland swells, men may notice:
- Frequent nighttime trips to the bathroom
- Weak or interrupted stream
- A feeling of incomplete emptying
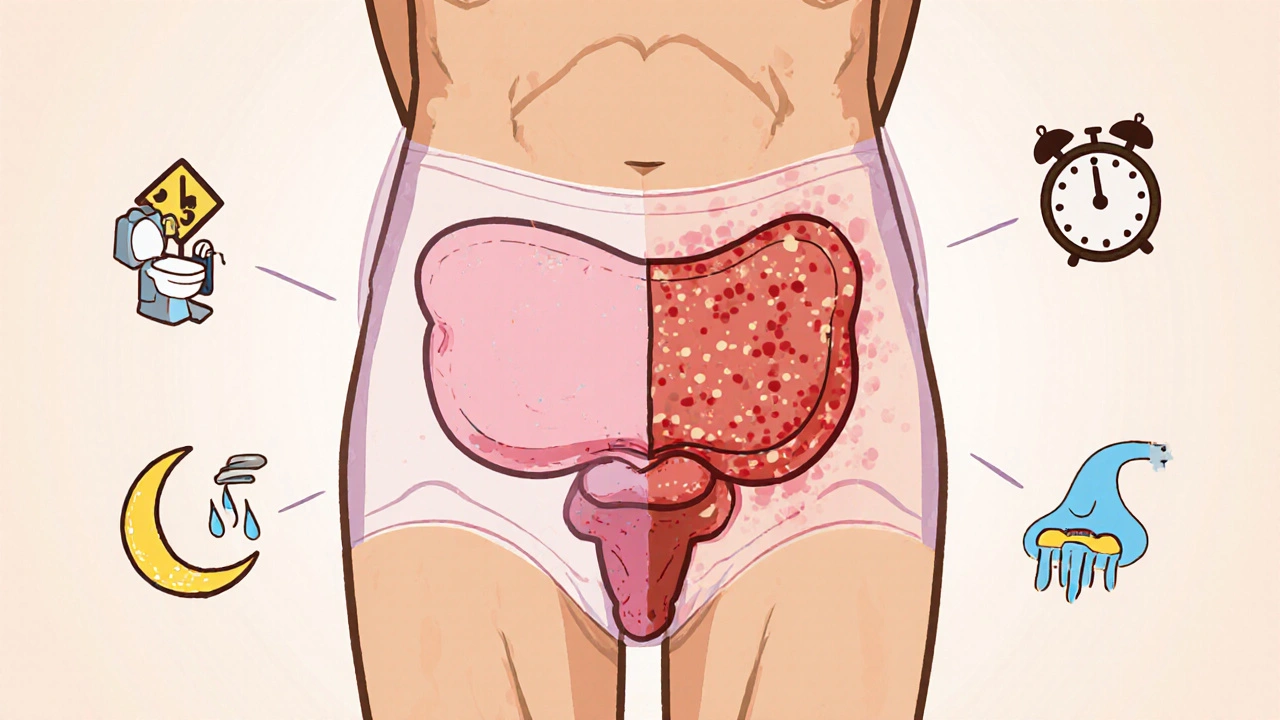
What is chronic prostatitis?
Chronic prostatitis, often labeled CP/CPPS Chronic prostatitis/chronic pelvic pain syndrome, a condition with pain lasting more than three months without a clear bacterial cause, is trickier to pin down. Unlike an infection that shows up on lab tests, CP/CPPS may involve low‑grade inflammation, nerve irritation, or stress‑related muscle tension. Typical complaints include:
- Pain in the pelvic area, lower back, or genital region
- Burning or discomfort during urination
- Painful ejaculation
- Occasional urinary urgency
Shared risk factors and biological links
Several mechanisms can tie an enlarged prostate to chronic prostatitis:
- Hormonal environment: High DHT levels not only enlarge the gland but also increase inflammatory cytokines inside prostate tissue.
- Urinary stasis: A larger prostate can block urine flow, causing residual urine that irritates the prostate lining and invites inflammation.
- Age‑related changes: Aging reduces immune regulation, making the prostate more prone to chronic low‑grade inflammation.
- Lifestyle influences: Diets high in red meat and low in omega‑3 fatty acids have been linked to both BPH progression and prostatitis flare‑ups.
- Micro‑trauma: Frequent straining during urination can damage the urethral wall, allowing irritants to reach the prostate.
Understanding these overlaps explains why treating one condition often improves the other.
Symptom comparison at a glance
| Aspect | Enlarged Prostate (BPH) | Chronic Prostatitis (CP/CPPS) |
|---|---|---|
| Primary cause | Hormonal‑driven gland growth | Persistent inflammation without clear infection |
| Typical age | 50 + years | 20‑60 years (can affect younger men) |
| Urinary symptoms | Frequency, weak stream, nocturia | Burning, urgency, occasional frequency |
| Pain location | Rarely painful | Pelvic floor, perineum, lower back |
| Diagnostic tests | Prostate‑specific antigen (PSA), ultrasound | Urine culture, expressed prostatic secretions, NIH‑CPSI questionnaire |
| First‑line treatment | Alpha blockers, 5‑alpha‑reductase inhibitors | Anti‑inflammatories, pelvic floor therapy, sometimes antibiotics |
How doctors diagnose the overlap
Urologists start with a detailed history and a digital rectal exam (DRE). If they suspect BPH, they’ll order a Prostate‑specific antigen (PSA) a blood marker that helps rule out prostate cancer and monitor gland size test. For chronic prostatitis, the doctor may ask you to provide a urine sample before and after a prostate massage to look for inflammatory cells.
Imaging like transrectal ultrasound can measure prostate volume, while MRI helps spot inflammation or structural abnormalities. Some clinics also use the NIH‑CPSI (Chronic Prostatitis Symptom Index) questionnaire to gauge pain severity and quality‑of‑life impact.
Treatment strategies that address both conditions
Because the two conditions share pathways, many therapies hit both targets.
- Alpha blockers (e.g., tamsulosin) relax the smooth muscle in the prostate and bladder neck, easing urinary flow for BPH and reducing pelvic pressure for prostatitis.
- 5‑alpha‑reductase inhibitors (e.g., finasteride) shrink the gland over months, which can lower the chance of urine stasis that fuels inflammation.
- Anti‑inflammatory meds such as ibuprofen or selective COX‑2 inhibitors relieve pain and may lessen prostatic swelling.
- Antibiotics are only useful if a bacterial component is found, but a short course is sometimes prescribed empirically for prostatitis flare‑ups.
- Pelvic floor physical therapy targets the muscles that often go into spasm with chronic prostatitis and can also improve bladder emptying disrupted by BPH.
- Lifestyle tweaks: Reduce caffeine and alcohol, stay hydrated (but avoid excessive fluid right before bedtime), eat a diet rich in fruits, vegetables, and omega‑3 fatty acids, and incorporate regular moderate exercise.
In severe cases where medication fails, minimally invasive procedures like transurethral resection of the prostate (TURP) or laser vaporization can dramatically cut gland size, often easing both urinary and pain symptoms.

When to seek professional help
If you notice any of the following, schedule a urology appointment promptly:
- Sudden increase in urinary frequency or urgency
- Pain that interferes with daily activities or sexual function
- Blood in urine or semen
- Difficulty starting or stopping urine flow
- Symptoms persisting more than a few weeks despite self‑care
Early evaluation can prevent complications such as urinary retention, bladder stones, or chronic pain syndromes.
Key take‑aways
- The prostate can enlarge (BPH) and become inflamed (chronic prostatitis) at the same time.
- Hormones, urinary stasis, age, and lifestyle all link the two conditions.
- Symptoms overlap, especially urinary issues, making accurate diagnosis essential.
- Many treatments-alpha blockers, anti‑inflammatories, pelvic floor therapy-help both conditions.
- Don’t ignore persistent pain or sudden urinary changes; see a urologist early.
Frequently Asked Questions
Can an enlarged prostate cause chronic prostatitis?
Yes. A larger prostate can obstruct urine flow, leading to residual urine that irritates the gland and triggers low‑grade inflammation, which may develop into chronic prostatitis.
Are the symptoms of BPH and chronic prostatitis identical?
They share urinary symptoms such as frequency and urgency, but chronic prostatitis also includes pelvic or perineal pain, painful ejaculation, and sometimes flu‑like feelings, which are less common in pure BPH.
Do PSA levels rise with chronic prostatitis?
PSA can be mildly elevated during prostatitis because inflammation releases more antigen into the bloodstream, but the rise is usually lower than the sharp increase seen with prostate cancer.
Is surgery ever needed for chronic prostatitis?
Surgery is rare for prostatitis alone. However, if a severely enlarged prostate (BPH) is causing chronic inflammation and medication fails, procedures like TURP can relieve both blockage and inflammation.
What lifestyle changes help both conditions?
Stay well‑hydrated, limit caffeine/alcohol, eat a plant‑rich diet, maintain a healthy weight, exercise regularly, and practice stress‑relief techniques such as yoga or meditation. These steps reduce hormonal spikes and inflammation.

Poornima Ganesan
October 18, 2025 AT 17:06First off, the link between DHT and inflammation is not some myth; numerous studies have shown that elevated DHT drives both hyperplasia and cytokine production. When the prostate cell mass expands, the local micro‑environment becomes hypoxic, which further fuels inflammatory mediators. Moreover, diet rich in saturated fats amplifies DHT synthesis, creating a feedback loop that worsens both BPH and CP/CPPS. Ignoring these hormonal cues is tantamount to ignoring the root cause. So if you’re only treating symptoms with alpha‑blockers, you’re missing the bigger picture.
Rajesh Singh
October 19, 2025 AT 22:16Let’s get real-popping endless cans of soda while guzzling red meat is practically a betrayal to your own bladder. You owe yourself a clean plate of leafy greens, omega‑3 rich fish, and a modest caffeine intake. It isn’t just about dodging a trip to the bathroom at 2 a.m.; it’s an act of self‑respect. If you keep feeding the prostate a banquet of hormones, you’re basically signing a contract with chronic pain.
Mike Hamilton
October 21, 2025 AT 02:53I think the article does a good job of explainng the overlap. The doctor will usually do a simple PSA and an ultrasound. It helps to keep an eye on all the symptoms.
Matthew Miller
October 22, 2025 AT 07:46Yo guys, don’t let BPH or prostatitis slow you down-stay active, hit the gym, and keep that pelvic floor strong! A daily walk and some Kegels can make a huge difference. Remember, you’re the boss of your own health, so grab that control and keep the flow smooth!
Norman Adams
October 23, 2025 AT 12:40Oh, sure, because the only thing standing between you and a peaceful night is a tiny gland that decided to grow a bit. Who needs nuanced medical advice when you can just blame your diet and call it a day? Apparently, the universe loves watching us squirm over urinary timetables.
Margaret pope
October 23, 2025 AT 13:46I get that it feels overwhelming you’re not alone we’ve all been there and a little patience goes a long way
Karla Johnson
October 24, 2025 AT 13:23When we discuss the interplay between an enlarged prostate and chronic prostatitis, it is essential to recognize that these conditions are not isolated incidents but parts of a broader urological continuum.
The hormonal milieu, specifically dihydrotestosterone, serves as both a growth factor and an inflammatory catalyst, a fact that is well‑documented in endocrine literature.
Clinical practitioners often observe that patients presenting with lower urinary tract symptoms also report pelvic discomfort, indicating a possible shared pathophysiology.
Age‑related immunosenescence further compromises the prostate’s ability to resolve low‑grade inflammation, thereby perpetuating chronic pain cycles.
Moreover, lifestyle components such as high red‑meat consumption and insufficient omega‑3 intake exacerbate both hyperplasia and inflammatory pathways.
While alpha‑blockers provide symptomatic relief, they do not address the underlying cytokine surge that drives tissue remodeling.
Similarly, 5‑alpha‑reductase inhibitors shrink gland volume but may also alter the balance of inflammatory mediators, an effect that warrants careful monitoring.
Patients should be educated on the importance of bladder emptying techniques, as urinary stasis creates a fertile environment for irritants.
Pelvic floor physical therapy, often overlooked, can simultaneously improve urinary flow and reduce muscular tension that contributes to prostatitis pain.
Nutrition counseling, emphasizing plant‑based foods, can modulate systemic inflammation and indirectly influence prostate health.
In addition, stress management strategies such as mindfulness or moderate exercise have been shown to lower sympathetic tone, which can exacerbate urinary urgency.
From a diagnostic standpoint, combining PSA testing with the NIH‑CPSI questionnaire provides a more comprehensive picture of both gland size and pain severity.
Imaging modalities like transrectal ultrasound and multiparametric MRI can differentiate between simple enlargement and areas of focal inflammation.
It is also prudent to consider a trial of short‑course antibiotics only when a bacterial component cannot be definitively excluded.
Ultimately, a multidisciplinary approach-urology, physiotherapy, nutrition, and mental health-offers the best chance for symptom resolution.
Therefore, patients and clinicians alike must move beyond siloed treatment algorithms and adopt an integrated strategy that targets both the mechanical and inflammatory aspects of prostate disease.
Linda A
October 24, 2025 AT 14:46Your thorough breakdown paints a vivid tapestry of the prostate’s silent battles. It reminds me of the ancient philosophers pondering the hidden forces within the body. Yet the drama of daily discomfort remains all too real for many.
Joe Moore
October 25, 2025 AT 17:10Yo, have you ever noticed how pharma pushes those alpha blockers like they’re the only answer? It’s like they want us stuck on meds forever. I bet there’s a hidden agenda behind the whole “surgery is last resort” spiel. Keep your eyes open, man.
Ayla Stewart
October 25, 2025 AT 18:33While it’s understandable to be sceptical, most urologists follow evidence‑based guidelines. It’s worth considering the benefits of a balanced treatment plan.
Emma Williams
October 26, 2025 AT 18:33Great summary thanks for the info
Stephanie Zaragoza
October 27, 2025 AT 22:20The article correctly delineates the overlapping etiologies of BPH and CP/CPPS; however, it could further emphasize the role of lifestyle modulation, such as dietary omega‑3 enrichment and regular aerobic activity, in mitigating inflammatory cascades. Additionally, the recommendation to employ both PSA screening and the NIH‑CPSI questionnaire provides a comprehensive diagnostic framework, which is commendable. Finally, emphasizing a multidisciplinary approach-including urology, physiotherapy, nutrition, and mental health-ensures holistic patient care.