Chronic Prostatitis: What You Need to Know
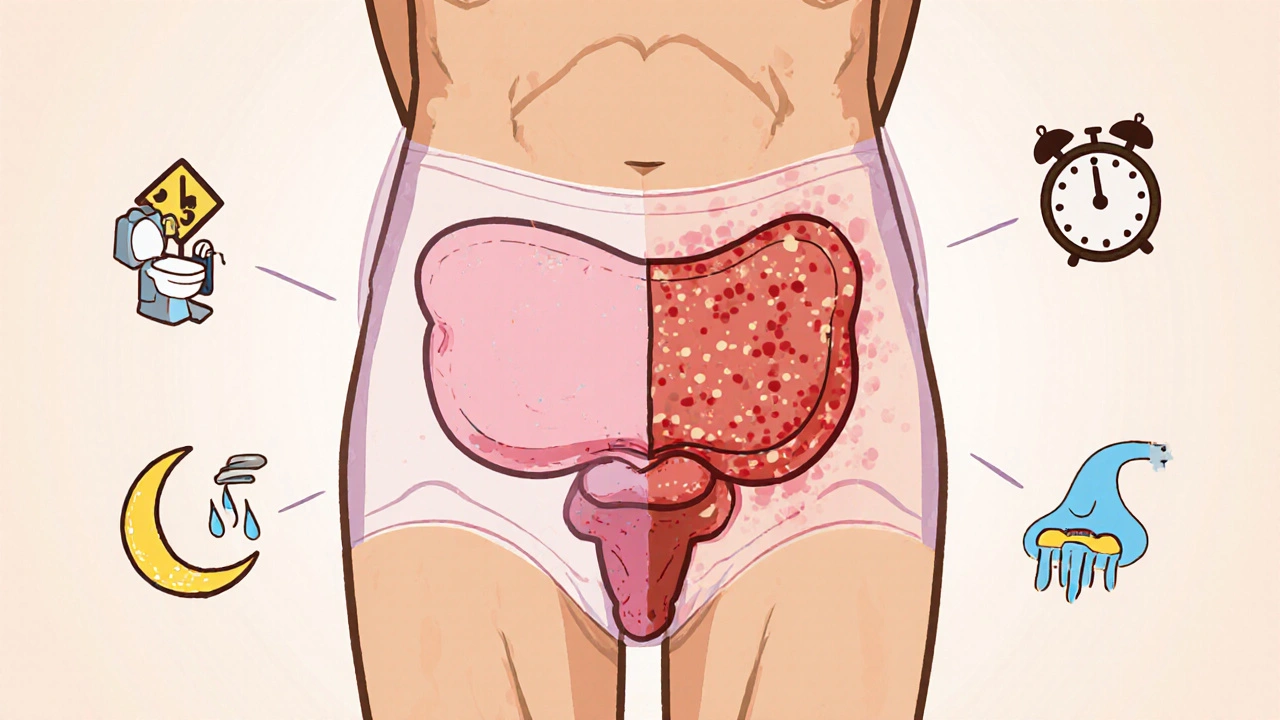
When dealing with chronic prostatitis, a long‑lasting inflammation of the prostate gland that often brings pelvic discomfort and urinary trouble. Also known as prostatic inflammation, it affects many men and can be tricky to pin down.
The condition chronic prostatitis encompasses three core ideas: it involves the prostate gland, it triggers persistent pelvic pain, and it frequently requires antibiotic therapy to control bacterial contributors. First, the prostate gland sits just below the bladder and surrounds the urethra, so any swelling directly irritates urinary flow. Second, pelvic pain can range from a dull ache to sharp throbbing, often worsening after sitting or during sexual activity. Third, doctors usually start a course of antibiotics because many cases stem from hidden bacterial infections, although non‑infectious inflammation also plays a role. Lifestyle factors such as frequent cycling, dehydration, or chronic stress can aggravate the inflamed tissue, while diet rich in spicy foods or alcohol may intensify symptoms. Diagnostic steps typically include a digital rectal exam, urine analysis, and sometimes a prostate massage to collect fluid for lab testing. Imaging like transrectal ultrasound helps rule out other prostate problems, ensuring the right treatment plan. Because the pain is often diffuse, patients sometimes confuse chronic prostatitis with other pelvic disorders like interstitial cystitis or musculoskeletal strain, making clear communication with a urologist essential.
Key Aspects of Managing Chronic Prostatitis
Understanding how the three entities interact makes treatment more effective. Antibiotic therapy targets the bacterial angle, while anti‑inflammatory meds and alpha‑blockers relax the prostate muscle, easing urinary obstruction. Physical therapy focused on the pelvic floor can relieve tension that fuels pain, and simple habits—drinking plenty of water, avoiding prolonged sitting, and practicing regular stretching—reduce flare‑ups. Some men find benefit from phytotherapy such as saw palmetto or quercetin, though evidence varies, so it’s wise to discuss supplements with a healthcare professional. Monitoring symptom patterns helps identify triggers; keeping a brief daily log of fluid intake, activity, and pain levels often reveals hidden connections. If standard antibiotics fail, doctors may consider longer‑term low‑dose options or explore newer agents that penetrate prostate tissue better. In rare cases where pain dominates and infection is ruled out, neuromodulators or low‑level laser therapy might be recommended. Throughout the process, open dialogue with the doctor ensures adjustments are made promptly, preventing chronic pain from spiraling. By combining targeted medication, lifestyle tweaks, and supportive therapies, most men achieve noticeable relief within a few weeks to months.
Below you’ll find a curated set of articles that dive deeper into each of these areas – from detailed antibiotic comparisons to practical tips for managing pelvic pain and improving prostate health. Whether you’re just starting to experience symptoms or looking for advanced strategies to keep flare‑ups at bay, the collection offers clear, actionable information to help you take control of chronic prostatitis.
How Enlarged Prostate and Chronic Prostatitis Are Linked
Explore how an enlarged prostate and chronic prostatitis are linked, covering causes, symptoms, diagnosis, and effective management options.





