ACE Inhibitors: What They Are, How They Work, and What You Need to Know
When your blood pressure stays too high, your heart and kidneys pay the price. That’s where ACE inhibitors, a class of medications that block the angiotensin-converting enzyme to relax blood vessels and lower pressure. Also known as angiotensin-converting enzyme inhibitors, these drugs are among the most prescribed for hypertension, heart failure, and kidney protection in people with diabetes. They don’t just lower numbers — they change how your body handles stress on the cardiovascular system.
ACE inhibitors work by stopping the body from making angiotensin II, a chemical that narrows blood vessels and raises blood pressure. By blocking this process, they let arteries widen, which reduces the workload on your heart. This makes them especially useful for people with heart failure, diabetes, or chronic kidney disease. Unlike some other blood pressure meds, they also help slow kidney damage — which is why doctors often pick them for patients with protein in their urine. They’re not magic, but they’re one of the few drug classes proven to protect organs, not just numbers.
They’re not without trade-offs. A dry cough is common — enough that some people stop taking them. High potassium levels can happen, especially if you’re also on potassium supplements or have kidney issues. And they’re not safe during pregnancy. But for millions of people, especially older adults and those with diabetes, they’re the go-to choice because they work reliably and come with long-term safety data. You’ll often see them paired with diuretics or calcium channel blockers when one drug isn’t enough.
What’s interesting is how these drugs show up in other areas too. Studies link them to lower rates of stroke and heart attack in high-risk groups. They’re used after heart attacks to improve survival. Even in people with normal blood pressure but early kidney disease, they’re recommended to delay damage. That’s why you’ll find them in posts about diabetes and heart disease, kidney health in African ancestry, and even in discussions about medication adherence — because if you feel fine, it’s easy to skip them, even though they’re working behind the scenes to protect you.
There’s no single ACE inhibitor that’s right for everyone. Some, like lisinopril, are taken once a day and cost very little. Others, like benazepril or enalapril, might be chosen based on kidney function or how your body processes them. They’re not the same as ARBs — those block the same final effect but work differently, and if you can’t tolerate the cough from an ACE inhibitor, that’s often the next step.
What you’ll find below is a collection of real-world stories and science-backed facts about how these drugs fit into bigger health pictures. You’ll see how they connect to kidney disease, heart protection, medication safety, and even how pharmacists help patients stay on track. There’s no fluff here — just what matters: how they work, who they help, and what to watch for. Whether you’re taking one, considering one, or just trying to understand why your doctor picked it, this is the practical guide you need.
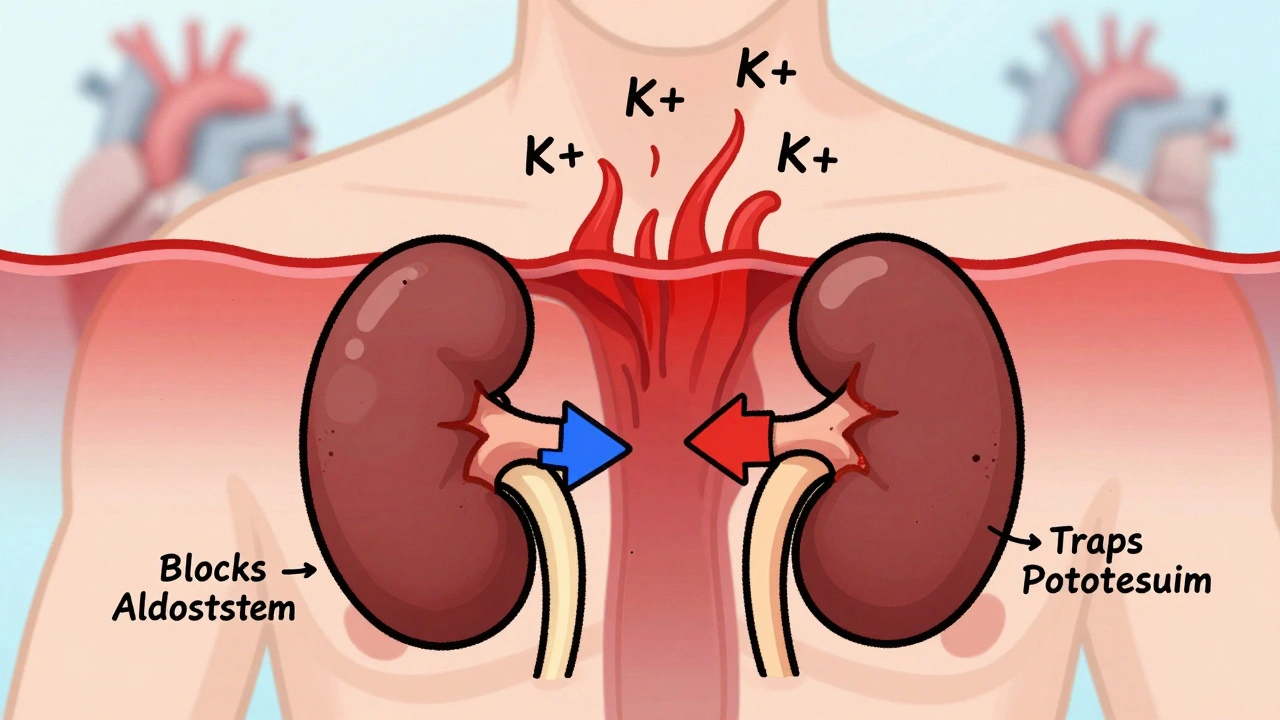
ACE Inhibitors and Potassium-Sparing Diuretics: Understanding the Hyperkalemia Risk
Combining ACE inhibitors and potassium-sparing diuretics can dangerously raise potassium levels, leading to life-threatening heart rhythms. Learn who's at risk, how to monitor, and what to do if levels climb.





