When a doctor prescribes a biosimilar-like Inflectra instead of Remicade-how does the clinic get paid? It’s not as simple as handing in a prescription and collecting a check. The way biosimilars are billed and reimbursed under Medicare Part B is a complex, rules-heavy system that affects everything from provider profits to patient access. Unlike generic pills, which are chemically identical to brand-name drugs, biosimilars are highly similar but not exact copies of complex biologic medicines. That difference changes how they’re coded, priced, and paid for-and it’s made billing for biosimilars one of the trickiest parts of modern healthcare finance.
How Biosimilars Got Their Own Codes
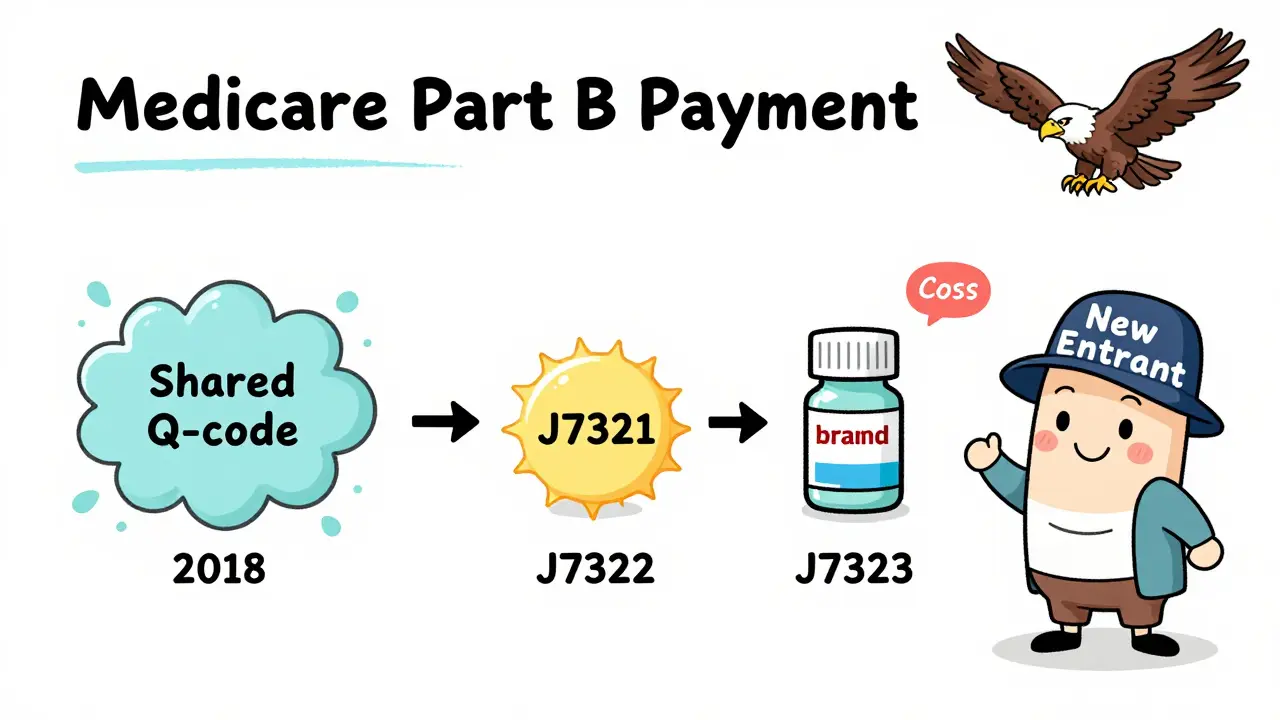
Before 2018, all biosimilars for the same reference drug shared one HCPCS code. For example, if two biosimilars were approved for infliximab (Remicade), they both used code Q5101. Payment was based on a blended average of all those products’ prices. That created a big problem: if one biosimilar came in cheaper, the others still got paid the same average rate. Why would a manufacturer bother lowering their price if they’d just be paid the same as the more expensive option? It was a disincentive to compete.
In January 2018, CMS flipped the script. Now, every FDA-approved biosimilar gets its own unique HCPCS code. Inflectra has J7321. Renflexis has J7322. Hadlima has J7323. Each one has its own payment rate based on its actual average selling price (ASP). This change was meant to reward manufacturers who bring down costs. If your biosimilar is cheaper, you get paid less-but you also have a better shot at being chosen by providers because it’s cheaper for the system overall.
How Much Do Providers Get Paid?
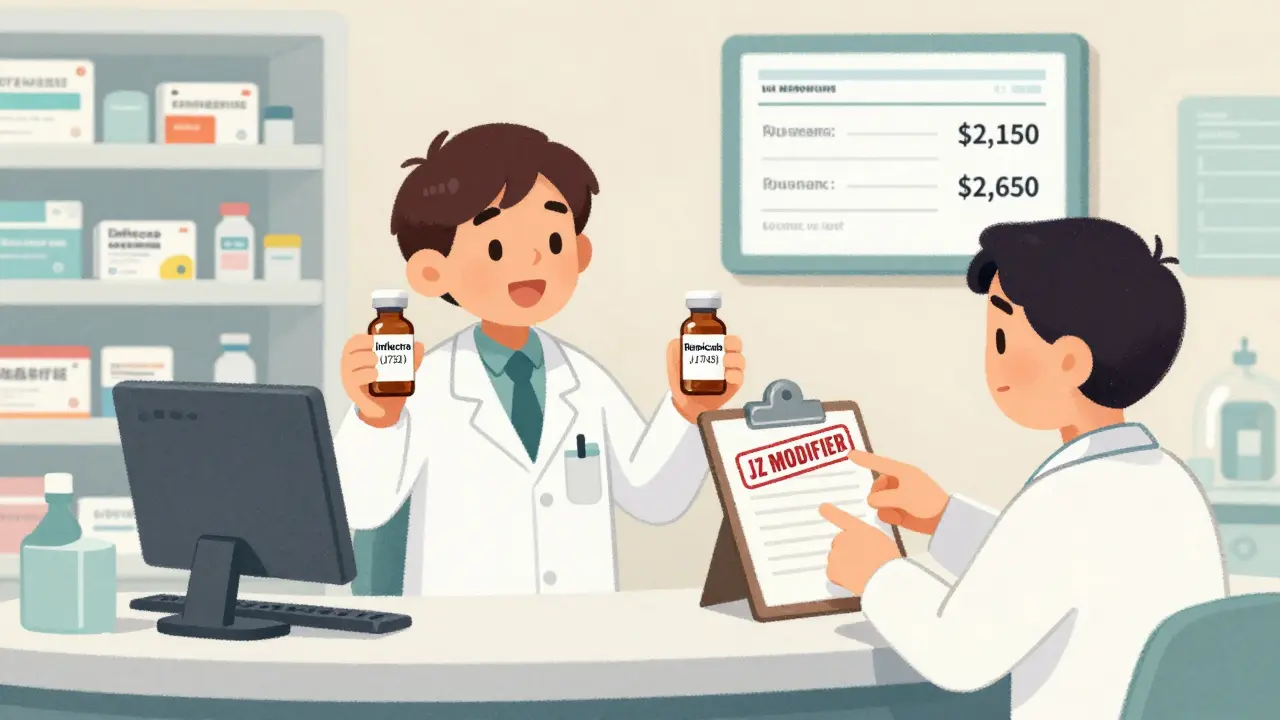
The payment formula sounds simple: 100% of the biosimilar’s ASP plus 6% of the reference product’s ASP. But here’s where it gets confusing. Let’s say Remicade costs $2,500 per dose, and Inflectra costs $2,000. The provider gets paid:
- 100% of Inflectra’s ASP = $2,000
- Plus 6% of Remicade’s ASP = $150
- Total = $2,150
That’s $150 more than what the biosimilar actually costs. But here’s the catch: if the provider uses Remicade instead, they get:
- 100% of Remicade’s ASP = $2,500
- Plus 6% of Remicade’s ASP = $150
- Total = $2,650
So the provider makes $500 more per dose using the brand-name drug. That’s not a small difference. It’s why, even with a 20% price drop, biosimilar adoption in the U.S. still lags behind Europe. In Europe, many countries pay the same amount regardless of which product is used-so providers have no financial reason to pick the expensive one. In the U.S., the system still rewards the higher-priced option.
The JZ Modifier: A New Layer of Complexity
Starting July 1, 2023, CMS added another layer: the JZ modifier. This code is required on claims for infliximab and its biosimilars when no drug is wasted. If a vial has 100 mg and the patient only needs 50 mg, the other 50 mg is discarded. That’s common. But if the provider uses a single-dose vial and administers the entire amount, they must add JZ to the claim. If they don’t, the claim gets denied.
Why? Because CMS wants to make sure providers aren’t getting paid for unused drug. But this created a new administrative burden. A 2023 survey of gastroenterology practices found billing staff spent 30% more time verifying discarded amounts. One clinic reported going from 10 minutes per claim to 13 minutes. That adds up fast when you’re handling dozens of infliximab injections a week.
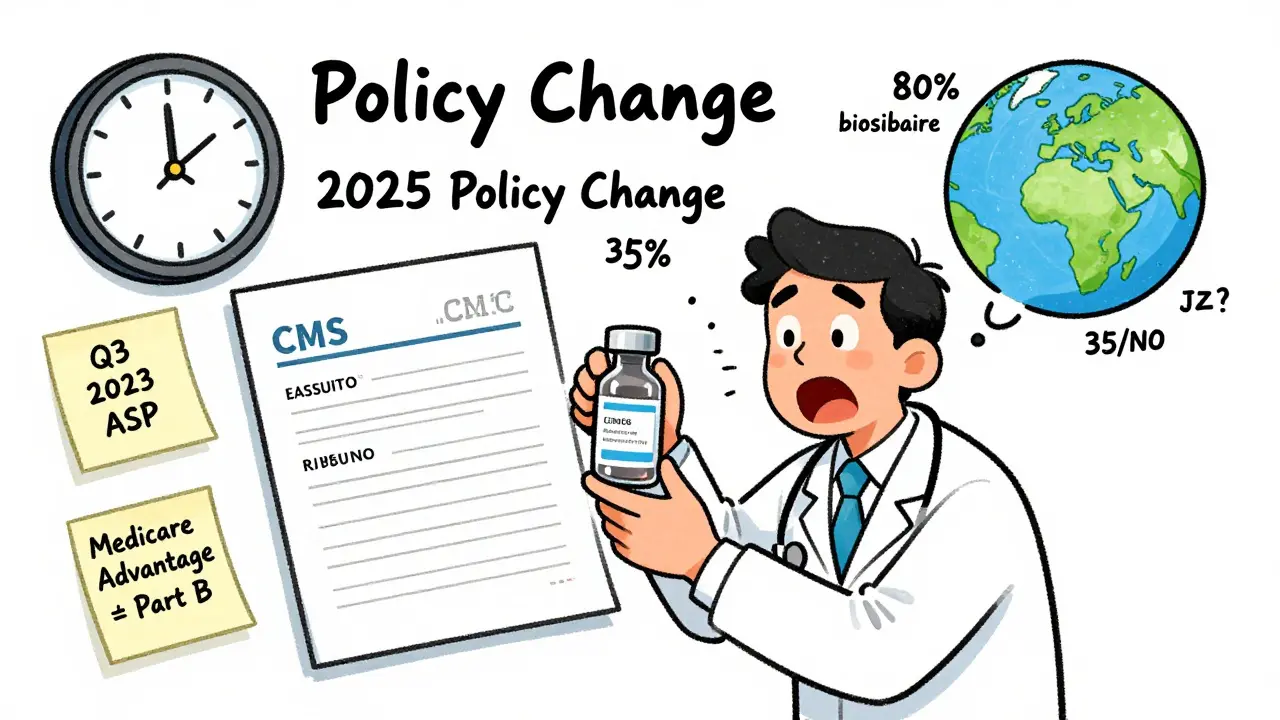
What Happens When a New Biosimilar Enters the Market?
When a new biosimilar launches, it doesn’t immediately get paid based on ASP. There’s a six-month grace period. During that time, CMS pays 106% of the wholesale acquisition cost (WAC)-the list price before discounts. This gives manufacturers time to collect real-world sales data. Once six months of sales are in, CMS switches to ASP-based payments. Subsequent biosimilars for the same drug skip the WAC phase entirely. They jump straight to ASP-based payment, because the system already has enough data to calculate it.
This staggered rollout helps new entrants survive the early months, but it also means the payment system is always catching up. Providers have to check CMS’s quarterly updates to make sure they’re using the right code and rate. Outdated codes are one of the top reasons claims get denied.
Why This Matters for Patients and Providers
For patients, the billing system doesn’t always translate into lower out-of-pocket costs. Medicare Part B pays providers based on ASP, but patients still pay 20% coinsurance. If the provider is paid $2,150 for a biosimilar, the patient still owes $430. If they get the brand-name drug, they owe $530. That’s a $100 difference-but patients rarely know which drug they’re getting, and few providers explain the cost difference.
For providers, especially oncology clinics and rheumatology practices, the system is a minefield. A 2022 survey of 217 cancer centers found 68% had billing confusion during the 2018 code switch. Nearly half had claims denied because someone used the wrong J-code. Training staff took 40 to 60 hours per practice. Even now, 22% of claim denials are due to using an old code.
Successful practices now use dual verification: the pharmacist checks the vial label, and the billing team checks the code against CMS’s latest update. That cuts error rates from 15% down to under 3%. But not every clinic has the resources for that.
How This Compares to Generics
It’s easy to think biosimilars are just like generic pills. They’re not. Generics have the same active ingredient and are AB-rated by the FDA. They share the same HCPCS code as the brand drug. Payment is the same. No modifiers. No separate codes. No ASP tracking.
Biosimilars? They’re treated like their own distinct products. Each one needs its own code. Each one has its own payment rate. Each one requires extra documentation. The system was built to handle complexity-not because it’s easy, but because biologics are too complex to treat like simple pills.
What’s Next? The Push for Change
Experts agree the current system works for tracking-but not for encouraging use. The 6% add-on tied to the reference product’s price is the biggest barrier. If the add-on was based only on the biosimilar’s price, providers would have a real incentive to switch. Avalere Health estimated that change could boost biosimilar use by 15-20 percentage points.
MedPAC has proposed a "least costly alternative" model: pay 106% of the weighted average price of all biosimilars and the reference product. That would eliminate the incentive to pick the expensive option. The Congressional Budget Office estimates this could save Medicare $3.2 billion over 10 years.
CMS is already listening. In February 2023, they issued a notice asking for feedback on whether to change the add-on structure. Some manufacturers are already preparing for it. If the change comes in 2025, as many expect, we could see a real surge in biosimilar adoption.
Right now, U.S. biosimilar market share sits at about 35%. In Europe, it’s 75-85%. The difference isn’t just about price. It’s about payment rules. Until the U.S. system stops rewarding the most expensive option, that gap won’t close.
What Providers Need to Do Today
If you’re billing for biosimilars, here’s what you need to do right now:
- Use the correct HCPCS code for the exact biosimilar administered. Check CMS’s quarterly updates.
- Apply the JZ modifier only when no drug is discarded (for infliximab products).
- Verify the patient’s plan: Medicare Part B pays 106% ASP. Medicare Advantage plans often pay less-sometimes only 100-103% ASP.
- Train staff to cross-check the vial label with the billing code before submission.
- Keep a copy of the manufacturer’s coding guide (Fresenius Kabi, Sandoz, and others publish these).
Don’t rely on memory. Don’t assume the code hasn’t changed. CMS updates its drug pricing files every quarter. One outdated code can cost you a claim-and a few hundred dollars.
Why This System Exists
This isn’t arbitrary. The system was designed to balance two goals: encourage new biosimilars to enter the market, and make sure providers aren’t losing money on expensive drugs. The individual codes help track which biosimilar is being used. The ASP-based payment ensures reimbursement reflects actual market prices. The 6% add-on was meant to cover handling and administration costs.
But the add-on is now outdated. It was never meant to be a profit driver. And it’s become one. The result? A system that tracks innovation well but doesn’t reward it.
Change is coming. The question is whether it will come fast enough to close the gap between U.S. and global adoption. Until then, providers are stuck in a system that pays more for the more expensive drug-and patients are left wondering why their co-pay didn’t go down when their doctor switched to a biosimilar.
Do biosimilars have the same HCPCS code as the reference biologic?
No. Each biosimilar has its own unique HCPCS code-either a J-code (permanent) or Q-code (temporary). The reference biologic keeps its original code. For example, Remicade uses J1745, while Inflectra uses J7321. This allows CMS to track each product’s usage and payment separately.
Why do providers sometimes still prescribe the brand-name biologic even when a biosimilar is available?
Because they make more money. The reimbursement for a biosimilar includes 6% of the reference product’s ASP, not the biosimilar’s. So if Remicade costs $2,500 and Inflectra costs $2,000, the provider gets $2,650 for Remicade but only $2,150 for Inflectra. That $500 difference per dose creates a financial incentive to stick with the brand.
What is the JZ modifier and when is it required?
The JZ modifier is required on claims for infliximab and its biosimilars when the entire contents of a vial are administered-meaning no drug is discarded. It was introduced on July 1, 2023. If a provider uses a 100 mg vial for a 50 mg dose and discards the rest, they do not use JZ. If they use a single-dose vial and give the full amount, they must use JZ. Failure to use it correctly leads to claim denials.
How often are biosimilar payment rates updated?
CMS updates biosimilar payment rates quarterly, based on the average selling price (ASP) reported by manufacturers. The most recent update was July 1, 2023. Providers must check the Medicare Physician Fee Schedule each quarter to ensure they’re using the correct code and payment amount.
Do Medicare Advantage plans pay the same as Medicare Part B for biosimilars?
No. Medicare Part B pays 106% of the ASP. Medicare Advantage plans often pay less-typically between 100% and 103% of ASP. Some plans may have their own formularies or prior authorization rules. Providers must verify payment terms with each plan, as reimbursement can vary significantly.
Is there a difference between biosimilars and generic drugs in billing?
Yes. Generic drugs share the same HCPCS code as the brand-name drug and are paid the same rate. Biosimilars have unique codes and are paid based on their own ASP plus 6% of the reference product’s ASP. This reflects their complexity and the fact that they’re not considered interchangeable by default.





Vinayak Naik
January 5, 2026 AT 16:57Man, this whole biosimilar billing mess is wild. I work in a clinic in Bangalore and we don’t even have this crap here-just one code, one price, everyone wins. Back home, if a drug’s cheaper, you use it. No 6% add-on nonsense. Here in the States, it’s like they’re paying doctors to pick the expensive stuff. Why?!
Kiran Plaha
January 6, 2026 AT 22:52So if I get the cheaper biosimilar, I still pay 20% of the brand’s price? That doesn’t make sense. Why isn’t my co-pay lower? I thought biosimilars were supposed to save us money.
Molly McLane
January 7, 2026 AT 03:48This is such an important breakdown. I’m a nurse in Texas and I see this confusion every day. Patients assume switching to Inflectra means cheaper bills-but they don’t realize their 20% coinsurance is still based on Remicade’s price. We need better patient education. Maybe even a simple handout: ‘Your drug is cheaper, but your copay isn’t.’ It’s not their fault they’re confused.
Lily Lilyy
January 8, 2026 AT 11:03Thank you for writing this! 🙌 This is the kind of clarity our healthcare system desperately needs. 💡 I’m so proud of how far we’ve come with biosimilars-even with all the bureaucratic mess. The fact that we’re even having this conversation means progress is happening. Keep pushing for change, because every little update brings us closer to affordable care for everyone. You’re doing amazing work! 🌟
Joann Absi
January 9, 2026 AT 19:23THE GOVERNMENT IS LYING TO YOU!!! 🤯 They say biosimilars save money-but look at this! They pay providers MORE for the expensive drug! This isn’t healthcare-it’s a corporate heist. Big Pharma owns CMS. They wrote these rules. They control the codes. They profit from your suffering. 🚨 Wake up, sheeple! This is why I don’t trust Medicare. They’re not here to help you-they’re here to line the pockets of the 1%. #MedicareIsBroken #BiosimilarScam
Ashley S
January 10, 2026 AT 20:12Ugh. So doctors are getting paid more to use the expensive drug? That’s disgusting. I’m not even mad-I’m just tired. Why do we keep letting this happen? People are dying because they can’t afford their meds, and the system rewards greed. I can’t even.
Rachel Wermager
January 11, 2026 AT 18:59The ASP+6% model is structurally inefficient because it creates a misalignment between reimbursement incentives and cost-containment objectives. The reference product’s ASP becomes a distortionary anchor, effectively subsidizing the brand-name drug through a perverse form of cost-shifting. The JZ modifier, while administratively burdensome, is a necessary step toward utilization transparency. However, without decoupling the add-on from the reference product, we’re merely optimizing for tracking, not for value-based care. The MedPAC proposal is the only viable path forward.
Tom Swinton
January 12, 2026 AT 02:30I’ve been in this game for 20 years, and honestly? This is the most messed-up billing system I’ve ever seen. I’ve had claims denied because someone used J7322 instead of J7323-on a Friday afternoon, right before a holiday. The clinic lost $12,000 that month. I’ve trained staff, printed laminated cheat sheets, set up alerts for CMS updates, and still, someone screws it up. It’s not the providers’ fault-it’s the system. It’s designed to fail. And now they’re adding modifiers? Please. We need a complete overhaul. Not tweaks. Not patches. A full reset.
Katelyn Slack
January 14, 2026 AT 02:26wait so if you use the biosimilar you get paid less but the patient still pays the same coinsurance? i think i read that wrong… is that right? because that seems… wrong? like really wrong? 😅
Melanie Clark
January 15, 2026 AT 19:34They’re hiding something. The JZ modifier? It’s not about waste. It’s about tracking. They’re building a database. Every vial. Every dose. Every patient. Who’s behind this? Who’s collecting this data? Big Pharma? The military? The NSA? They’re not trying to save money-they’re trying to control you. And when they stop paying for biosimilars entirely? You’ll see. Just wait.
Brian Anaz
January 17, 2026 AT 13:51Europe’s doing it right. We’re doing it wrong. End of story. We’re the only country that pays more for the expensive drug. That’s not healthcare. That’s American exceptionalism gone rogue. We’re not innovating-we’re subsidizing greed. Fix the add-on or shut it down. This isn’t rocket science.
Venkataramanan Viswanathan
January 19, 2026 AT 10:30In India, we have no such complexity. Biosimilars are priced transparently, coded under generic categories, and reimbursed uniformly. The U.S. system is not just complicated-it is unnecessarily convoluted. The 6% add-on is an artifact of a bygone regulatory era. The innovation exists; the payment model does not. One must wonder: is this complexity a feature or a bug?
Saylor Frye
January 21, 2026 AT 03:25Interesting. But honestly? I’m more intrigued by the cultural implications. The fact that we’ve created a financial incentive structure that actively discourages cost-saving innovation suggests a deeper pathology in our healthcare ethos. We reward inefficiency. We glorify brand. We fetishize price as quality. It’s not about drugs-it’s about identity. The biosimilar is the poor cousin. The brand is the heir. And we, as a society, still bow to the crown.
Matt Beck
January 21, 2026 AT 13:46Let’s be real for a second. 💸 This whole system is a joke. The 6% add-on? It’s not a ‘handling fee’-it’s a bribe. Big Pharma pays lobbyists to keep it. CMS doesn’t care about patients-they care about keeping the money flowing to the same 5 companies. And now they’re adding JZ? Like, congrats, you made billing take 30% longer. But did you save anyone money? Nope. You just made everyone more stressed. 🤦♂️ We need to burn this whole thing down and start over. #BiosimilarJustice