Nosebleed Risk Calculator
How Likely Are Your Medications Causing Nosebleeds?
Answer these questions to get a personalized risk assessment based on the article content.
Ever had a nosebleed out of nowhere and wondered if your meds might be to blame? You’re not alone. Around 60% of people experience a nosebleed at least once in their life, but for many, it’s not just dry air or a bad habit-it’s something they’re taking every day. Medications can quietly turn your nose into a fragile spot, especially if you’re on blood thinners, painkillers, or even allergy sprays. The good news? Most of these nosebleeds are preventable-and you don’t have to stop your meds to make it happen.
Which Medications Cause Nosebleeds?
It’s not just the big, scary drugs. Some of the most common medicines people take daily can trigger nosebleeds. The biggest culprits fall into three groups: blood thinners, pain relievers, and nasal sprays.Aspirin, even the low-dose kind (81mg) taken for heart health, is one of the top offenders. It doesn’t just reduce pain-it stops platelets from clumping together, which is great for preventing clots but bad for stopping nosebleeds. The same goes for ibuprofen (Advil, Motrin) and naproxen (Aleve). These NSAIDs work the same way, making your blood less likely to clot when you need it to.
Then there are the real heavyweights: warfarin (Coumadin), clopidogrel (Plavix), and heparin. These are prescribed for serious conditions like atrial fibrillation or after a stroke. But they work by thinning your blood significantly, and that means even a small bump inside your nose can lead to bleeding that won’t stop easily. In fact, patients on these drugs are 3 to 5 times more likely to have nosebleeds than those who aren’t.
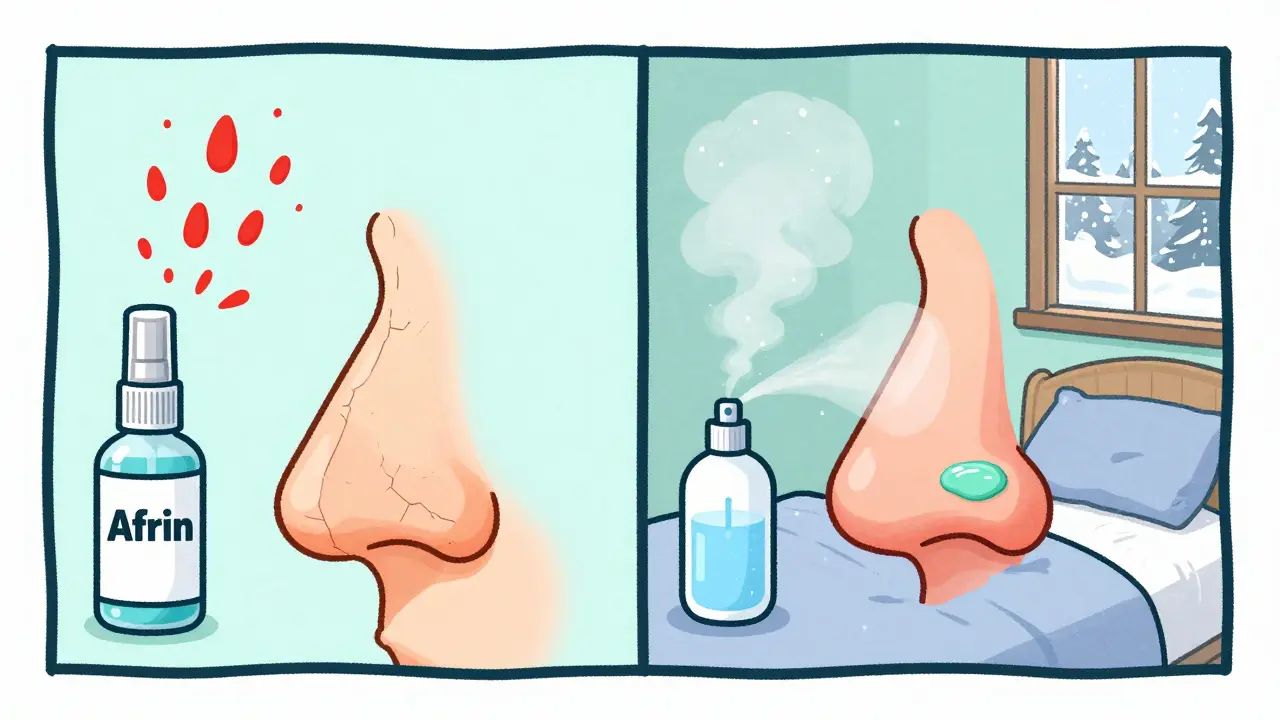
Don’t forget about nasal sprays. Oxymetazoline (Afrin) gives quick relief for congestion, but if you use it longer than 3 days, your nose pays the price. The spray shrinks blood vessels at first, but then they rebound, swelling bigger than before. Over time, the lining dries out, cracks, and bleeds. Same goes for long-term use of antihistamines and decongestants-they dry up your nasal passages, turning delicate blood vessels into easy targets.
Why Your Nose Is So Vulnerable
Your nose isn’t just a passageway for air. Inside, right near the front, there’s a dense network of tiny blood vessels called Kiesselbach’s plexus. It’s one of the most vascular areas in your whole body. That’s why even a tiny scratch or dry crack can cause bleeding.When you take medications that thin your blood or dry out your nasal lining, you’re basically removing two layers of protection. No clotting ability + dry, brittle tissue = nosebleed waiting to happen. It’s not magic-it’s biology. And it’s why someone on aspirin might get a nosebleed after blowing their nose too hard, while someone not on meds wouldn’t even notice it.
This is especially true in winter. Indoor heating drops humidity to 20-30%, and your nose dries out even faster. Combine that with daily NSAIDs or a nasal spray, and you’ve got the perfect storm.
How to Stop Nosebleeds When They Happen
If you feel blood starting to flow, don’t panic. Most nosebleeds stop on their own if you handle them right.- Pinch your nose. Use your thumb and index finger to squeeze the soft part of your nose shut. Don’t just tap it-squeeze hard enough to feel pressure. Keep it pinched for 10 to 15 minutes. Set a timer. Most people think they’ve done it long enough after 5 minutes, but it takes longer than you think.
- Stay upright. Lean slightly forward, not back. Tilting your head up lets blood run down your throat, which can make you gag or even vomit. Swallowing blood isn’t dangerous, but it’s unpleasant and can irritate your stomach.
- Don’t stuff tissues. Avoid putting cotton or paper inside your nose. That can cause more damage when you pull it out.
- Apply cold. Hold an ice pack or cold washcloth to the bridge of your nose. Cold helps shrink blood vessels and slow bleeding.
If the bleeding doesn’t stop after 15 minutes, or if you’re feeling dizzy, weak, or lightheaded, get medical help right away. Same goes if the nosebleed followed a fall, hit to the face, or if you’re on blood thinners and the bleeding won’t quit.
Prevention: Simple Steps That Actually Work
You don’t need to quit your meds. You just need to protect your nose.- Switch pain relievers. If you’re taking ibuprofen or aspirin regularly, talk to your doctor about switching to acetaminophen (Tylenol). It doesn’t affect clotting, so it’s much safer for your nose.
- Moisturize daily. Put a thin layer of petroleum jelly (Vaseline) inside each nostril, twice a day-morning and before bed. It’s simple, cheap, and works better than most sprays. If you prefer, use a saline nasal gel or spray twice a day.
- Use a humidifier. Especially in winter, run a cool-mist humidifier in your bedroom. Keeping indoor humidity above 40% makes a huge difference. Dry air is the silent partner in most nosebleeds.
- Avoid nose picking and rubbing. This sounds obvious, but people do it without realizing. Even scratching your nose with a tissue can trigger bleeding if your lining is thin.
- Limit nasal sprays. If you’re using oxymetazoline (Afrin), stop after 3 days. If congestion returns, talk to your doctor about alternatives like steroid sprays (Flonase) or saline rinses.
Who’s at Highest Risk?
Some people are more likely to get medication-related nosebleeds:- Adults over 45-blood vessels naturally become more fragile with age.
- Pregnant women-hormones cause nasal blood vessels to expand, making them easier to rupture.
- Children-they pick their noses, and their nasal lining is thinner. Even mild medications can trigger bleeding.
- People with high blood pressure or atherosclerosis-these conditions already stress the blood vessels in your nose.
- Those on multiple blood-thinning meds-combining aspirin with warfarin or clopidogrel multiplies the risk.
If you’re in one of these groups and you’ve had more than three nosebleeds in a week, it’s time to get checked. It’s not normal. It’s a signal.

When to Call Your Doctor
Not every nosebleed needs a doctor. But here’s when you should call:- Bleeding lasts longer than 20 minutes despite pressure
- You feel faint, dizzy, or your heart races
- You’re on blood thinners and the bleeding won’t stop
- You’re bleeding from other places-gums, urine, or bruising easily
- You’ve had more than 3 nosebleeds in a week
- The nosebleed followed a head injury
Your doctor or pharmacist can review your meds and see if any can be swapped, lowered, or replaced. Sometimes, switching from aspirin to a different antiplatelet drug, or adjusting your warfarin dose, can cut nosebleeds dramatically without increasing clot risk.
The Role of Your Pharmacist
Pharmacists aren’t just the people who hand you pills. They’re trained to spot drug interactions and side effects. If you’re getting frequent nosebleeds, bring your full med list to your pharmacist. They can check for combinations that increase bleeding risk-like mixing NSAIDs with warfarin-or suggest safer alternatives.Many people don’t realize that pharmacists can recommend non-prescription solutions too, like saline sprays, humidifiers, or even specific brands of nasal ointments that work better than others.
Final Thought: Don’t Ignore It
A nosebleed might seem small, but when it’s linked to your meds, it’s a warning sign. Ignoring it won’t make it go away. It might get worse. And if you’re on blood thinners, what starts as a minor bleed can turn into something serious fast.The goal isn’t to stop your medication-it’s to protect your body while still treating your condition. With a few simple changes-moisturizing your nose, switching painkillers, using a humidifier-you can stop nosebleeds in their tracks without giving up the drugs you need.
Can aspirin cause nosebleeds even at low doses?
Yes. Even low-dose aspirin (81mg), commonly taken for heart health, interferes with platelet function and can make nosebleeds more likely and harder to stop. Studies show people on daily aspirin have a significantly higher risk of epistaxis compared to those who don’t take it.
Is it safe to use Afrin (oxymetazoline) if I get nosebleeds?
No, not for long. Afrin provides quick relief but causes rebound congestion and dries out nasal tissue if used for more than 3 days. This makes your nose more prone to bleeding. If you need ongoing relief, ask your doctor about steroid nasal sprays like Flonase or saline rinses instead.
Should I stop my blood thinner if I get frequent nosebleeds?
Never stop a blood thinner without talking to your doctor. The risk of a stroke or clot from stopping the medication is often much higher than the risk of nosebleeds. Instead, work with your doctor to adjust your dose, switch medications, or add nasal protection strategies like moisturizers and humidifiers.
Can children get nosebleeds from medications too?
Yes. Children are more vulnerable because their nasal lining is thinner and they often pick their noses. Medications like ibuprofen or antihistamines can increase bleeding risk. Always check with a pediatrician before giving any OTC meds to a child who gets frequent nosebleeds.
What’s the best way to moisturize my nose to prevent nosebleeds?
Apply a thin layer of petroleum jelly (Vaseline) inside each nostril twice a day-morning and night. Saline nasal sprays or gels work well too. Avoid alcohol-based sprays, which dry out tissue. Humidifiers in the bedroom also help maintain moisture in the air.
How do I know if my nosebleeds are caused by meds and not something else?
If your nosebleeds started or got worse after beginning a new medication, and they’re not linked to trauma or allergies, meds are likely the cause. Other signs: bleeding from other areas (gums, skin), frequent episodes (3+ per week), or if they happen in dry conditions. A doctor can check your INR, platelet count, or rule out other conditions like high blood pressure or nasal polyps.








Dan Alatepe
December 26, 2025 AT 22:20Angela Spagnolo
December 27, 2025 AT 12:54Sarah Holmes
December 28, 2025 AT 08:23Jay Ara
December 29, 2025 AT 22:40Michael Bond
December 31, 2025 AT 18:55Kuldipsinh Rathod
January 1, 2026 AT 20:39SHAKTI BHARDWAJ
January 3, 2026 AT 16:04Matthew Ingersoll
January 3, 2026 AT 21:26carissa projo
January 4, 2026 AT 02:02josue robert figueroa salazar
January 4, 2026 AT 15:44david jackson
January 4, 2026 AT 21:41Jody Kennedy
January 5, 2026 AT 14:20christian ebongue
January 7, 2026 AT 07:57Prasanthi Kontemukkala
January 8, 2026 AT 02:29Alex Ragen
January 9, 2026 AT 13:21