Lanoxin vs Other Heart Medications: Digoxin Comparison Guide
Recommended Treatment Approach
Select your condition and patient profile, then click "Compare Medications" to see the recommended treatment approach.
Lanoxin (Digoxin)
Cardiac glycoside for heart failure and atrial fibrillation. Strengthens heart contractions and slows heart rate.
- Positive inotropy
- Negative chronotropy
- Used when other drugs cause low BP
Beta-Blockers
Control heart rate and reduce workload on the heart. May be combined with digoxin for rate control.
- Rate control
- Reduce mortality
- May cause bradycardia
ACE Inhibitors
Lower blood pressure and reduce strain on the heart. Essential for heart failure management.
- Heart failure treatment
- Reduce mortality
- May cause cough
SGLT2 Inhibitors
Newer class that reduces hospitalizations and cardiovascular death in heart failure patients.
- Heart failure therapy
- Renal protection
- Weight loss
Important Notes
- Digoxin requires careful monitoring of serum levels and kidney function
- Combination therapy may be needed for optimal results
- Individual patient factors determine the best treatment approach
Quick Takeaways
- Lanoxin (digoxin) is a cardiac glycoside mainly for heart failure and atrial fibrillation.
- It works by strengthening heart contractions and slowing the heart rate.
- Key monitoring: serum digoxin level, kidney function, electrolytes.
- Common alternatives include beta‑blockers, ACE inhibitors, ARBs, mineralocorticoid receptor antagonists, calcium‑channel blockers, and SGLT2 inhibitors.
- Choose digoxin when you need rate‑control plus an inotropic boost, especially in sedentary patients or when other drugs cause low blood pressure.
What Is Lanoxin (Digoxin)?
Lanoxin is the brand name for digoxin, a cardiac glycoside extracted from the foxglove plant (Digitalis lanata). It has been used for more than a century to improve cardiac output in heart failure and to control ventricular response in atrial fibrillation. Because it narrows the gap between oxygen demand and supply, digoxin remains a niche but valuable option in modern cardiology.
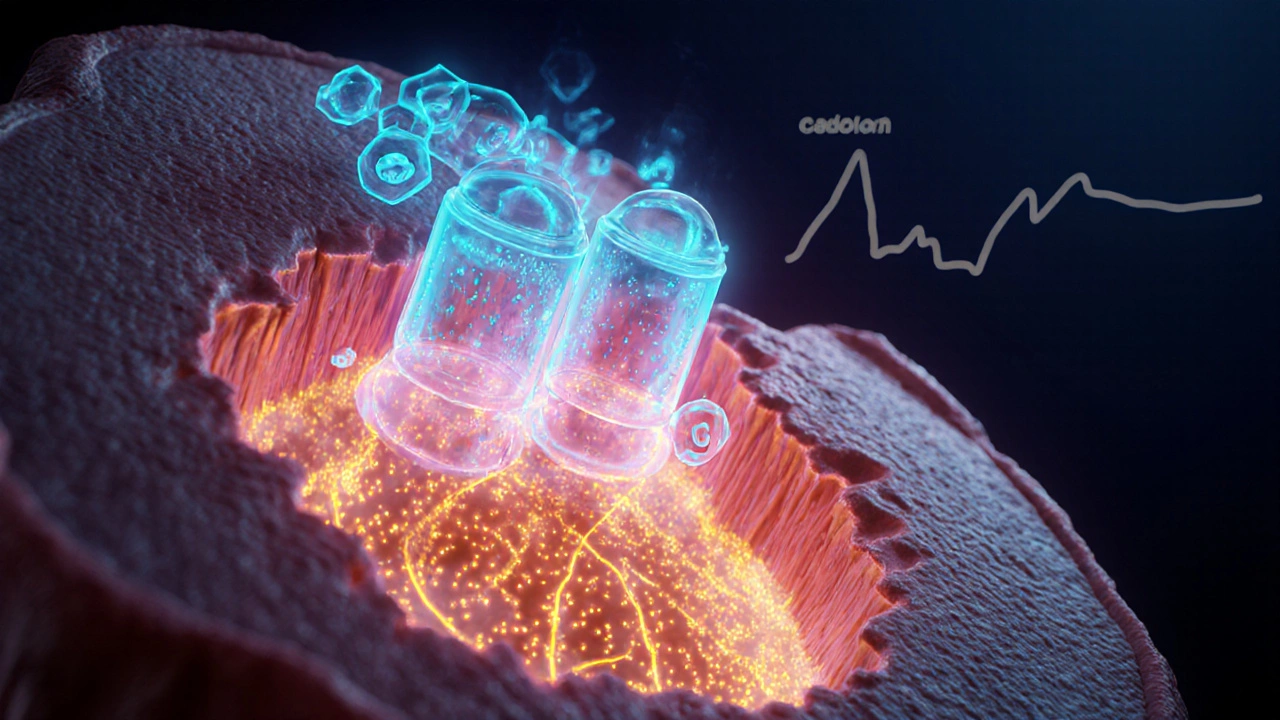
How Digoxin Works
Digoxin binds to the sodium‑potassium ATPase pump on cardiac cells, inhibiting the pump and causing a modest rise in intracellular calcium. The extra calcium strengthens each contraction (positive inotropy) and the drug also enhances vagal tone, slowing conduction through the AV node (negative chronotropy). The net effect is a stronger, slower‑pumping heart.
When Is Digoxin Typically Prescribed?
Guidelines reserve digoxin for patients who:
- Have systolic heart failure (EF<35%) and remain symptomatic despite ACE inhibitor/ARB and beta‑blocker therapy.
- Need rate‑control in atrial fibrillation but cannot tolerate high‑dose beta‑blockers or calcium‑channel blockers because of hypotension or bronchospasm.
- Are elderly, sedentary, or have reduced renal clearance where a low, steady digoxin level provides consistent benefit.
Typical dosing starts at 0.125mg daily for patients with a creatinine clearance <50ml/min, with serum levels targeted between 0.5-0.9ng/mL for heart failure and 0.8-2.0ng/mL for atrial fibrillation.
Key Safety Points
Digoxin has a narrow therapeutic window. Toxicity can appear as nausea, visual halos, confusion, or serious arrhythmias. The following checks are non‑negotiable:
- Therapeutic drug monitoring - check serum level 6-8hours after the first dose, then at steady state (≈1week).
- Renal function - dose‑adjust if eGFR<50ml/min.
- Electrolytes - hypokalemia, hypomagnesemia, or hypercalcemia dramatically raise toxicity risk.
- Drug interactions - be wary of amiodarone, quinidine, verapamil, and some antibiotics (e.g., clarithromycin) which raise digoxin levels.
Common Alternatives to Digoxin
Below are the most frequently used drug classes that can replace digoxin depending on the clinical goal.
- Beta‑blockers (e.g., metoprolol, carvedilol) - primary agents for heart failure mortality reduction and atrial fibrillation rate‑control.
- ACE inhibitors (e.g., enalapril, lisinopril) - improve remodeling and lower mortality in systolic heart failure.
- AngiotensinII receptor blockers (ARBs) (e.g., losartan, valsartan) - similar benefits to ACE inhibitors, useful when cough occurs.
- Mineralocorticoid receptor antagonists (e.g., spironolactone, eplerenone) - add survival benefit and lower hospitalization risk.
- Calcium‑channel blockers (e.g., diltiazem, verapamil) - good for rate‑control in atrial fibrillation but can depress contractility, so not first‑line in heart failure.
- SGLT2 inhibitors (e.g., dapagliflozin, empagliflozin) - newer class that cuts heart‑failure hospitalizations and can be added to standard therapy.

Side‑by‑Side Comparison
| Drug/Class | Mechanism | Primary Indication | Onset (hrs) | Half‑Life | Typical Monitoring | Common Side Effects |
|---|---|---|---|---|---|---|
| Digoxin | Inhibits Na⁺/K⁺‑ATPase → ↑ intracellular Ca²⁺ | Heart failure, atrial fibrillation | 1-2 (IV), 6-8 (oral) | 36-48 (renal) | Serum level, renal function, electrolytes | Nausea, visual halos, arrhythmias |
| Beta‑blocker (e.g., metoprolol) | β‑adrenergic blockade → ↓ heart rate & contractility | Heart failure, atrial fibrillation | 4-6 | 6-12 | Heart rate, blood pressure | Bradycardia, fatigue, bronchospasm |
| ACE inhibitor (e.g., enalapril) | Blocks conversion of Ang I → Ang II | Heart failure, hypertension | 4-6 | 12-24 | Renal function, potassium | Cough, hyperkalemia, angioedema |
| Calcium‑channel blocker (e.g., diltiazem) | Blocks L‑type Ca²⁺ channels → ↓ AV‑node conduction | Atrial fibrillation rate‑control | 3-4 | 30-40 | Heart rate, blood pressure | Constipation, edema, negative inotropy |
| SGLT2 inhibitor (e.g., dapagliflozin) | Inhibits renal glucose reabsorption → osmotic diuresis | Heart failure (reduced & preserved EF) | 12-24 | 12-13 | Renal function, glucose, volume status | UTI, genital infections, dehydration |
When to Pick Digoxin Over Alternatives
Even with newer agents, digoxin still shines in a few scenarios:
- Rate‑control plus inotropy - patients with low output heart failure who also need a slower ventricular rate benefit from a single pill.
- Renal‑friendly dosing - low‑dose digoxin is cleared renally and can be titrated precisely, useful when other drugs cause hypotension.
- Cost considerations - generic digoxin is cheap, making it attractive for patients with limited insurance coverage.
Conversely, avoid digoxin if you have:
- Significant electrolyte disturbances (especially low potassium).
- Advanced AV‑block without a pacemaker.
- History of digoxin toxicity.
Practical Tips for Switching or Adding Therapy
- Review kidney function and electrolytes before any dose change.
- If moving to a beta‑blocker, start low (e.g., metoprolol 12.5mg BID) and uptitrate every 2weeks.
- When adding an ACE inhibitor, monitor for cough and potassium; a rise above 5.5mmol/L calls for dose adjustment.
- For patients already on digoxin, check the serum level 5‑7days after starting or stopping interacting drugs like amiodarone.
- Educate patients to report visual disturbances, nausea, or palpitations immediately - these are red‑flags for toxicity.
Frequently Asked Questions
Is digoxin still used in 2025?
Yes. Although newer heart‑failure drugs have taken center stage, digoxin remains a guideline‑recommended option for patients who need both rate‑control and a modest boost in contractility, especially when cost or blood‑pressure concerns limit other choices.
How long does it take for digoxin to start working?
When taken orally, therapeutic effects usually appear within 6-8hours, but full steady‑state benefits may take up to a week. Intravenous loading can achieve a response in 1-2hours.
Can I take digoxin with a beta‑blocker?
Yes, many patients use both. The combination provides stronger rate‑control while preserving an inotropic effect. However, you should monitor heart rate and blood pressure closely to avoid excessive bradycardia.
What are the warning signs of digoxin toxicity?
Early signs include nausea, vomiting, loss of appetite, and visual changes such as yellow‑green halos. Later, patients may develop confusion, arrhythmias (e.g., premature ventricular beats), or heart block. Prompt lab testing and medical review are essential.
How does a Digoxin comparison help me choose a medication?
Seeing side‑by‑side data on mechanism, onset, monitoring, and side effects lets you weigh the pros and cons relative to your health status, other medicines, and lifestyle. It clarifies whether digoxin’s unique inotropic boost outweighs the monitoring burden compared with, say, a beta‑blocker or an SGLT2 inhibitor.







Michael Leaño
October 8, 2025 AT 12:14Great breakdown! I love how you highlighted the niche role of digoxin when other meds drop the blood pressure too low. For patients who are sedentary, this can be a real lifeline. Keep the info coming, it really helps us navigate the complexities of heart failure management.
Anirban Banerjee
October 9, 2025 AT 14:38In accordance with established clinical guidelines, the comparative analysis presented herein elucidates the pharmacodynamic distinctions between cardiac glycosides and contemporary antihypertensive agents. The exposition is thorough and adheres to a commendable standard of scholarly rigour.
Mansi Mehra
October 10, 2025 AT 17:02Overall the article is clear and useful. It mentions the need to monitor serum levels and kidney function, which is essential. The language is simple and direct, making it accessible.
Jagdish Kumar
October 11, 2025 AT 19:26Ah, the drama of the cardiovascular arena! One cannot simply dismiss digoxin as antiquated; it commands a certain aristocratic flair among the pantheon of heart drugs. Its ability to coax the myocardium into a more vigorous contraction while whispering the AV node into calmness is nothing short of poetic. Yet, the modern clinician must balance this elegance with the ever‑present risk of toxicity-an exquisite tightrope walk.
Aminat OT
October 12, 2025 AT 21:50Yo digoxin can be a real lifesaver for folks with low bp, no lie.
Amanda Turnbo
October 14, 2025 AT 00:14The guide is solid, but I’d caution readers to avoid over‑reliance on any single agent. Digoxin’s narrow therapeutic window demands diligent labs and patient education. Otherwise, the benefits quickly turn into hazards.
Jenn Zuccolo
October 15, 2025 AT 02:38One might contemplate the metaphysical implications of a drug that both strengthens and slows the heart. It is as if Digoxin teaches us to embrace paradox: vigor married to patience.
Courtney The Explorer
October 16, 2025 AT 05:02Patriots of cardiac care must recognize that our historic drug arsenal, including digoxin, remains vital. Innovation should not erase proven efficacy.
Ashleigh Connell
October 17, 2025 AT 07:26Loving the colorful breakdown! It's refreshing to see a guide that mixes science with a dash of creativity. Kudos for making a potentially dry topic feel approachable.
Erin Knight
October 18, 2025 AT 09:50While the article attempts to be comprehensive, it glosses over the grim reality of digoxin toxicity in the elderly. A more critical lens is needed.
Kavita Jadhav
October 19, 2025 AT 12:14I appreciate the balanced view that acknowledges both the strengths and the necessary cautions. Empathy for patients navigating these choices is crucial.
Tony Halstead
October 20, 2025 AT 14:38Allow me to expound at length on why digoxin retains its distinguished place in the therapeutic armamentarium. First, the drug’s unique mechanism-a direct inhibition of the Na⁺/K⁺‑ATPase pump-confers a modest but clinically meaningful increase in intracellular calcium, thereby augmenting contractility without precipitating the vasodilatory plunge observed with many contemporary agents. Second, its vagomimetic properties grant a gentle deceleration of the atrioventricular node, furnishing rate control that is especially valuable in atrial fibrillation when beta‑blockers threaten hypotension. Third, in the subset of patients with renal insufficiency, dose titration guided by serum digoxin concentrations can safely harness its benefits, a nuance that newer agents occasionally overlook. Fourth, the drug’s long half‑life permits once‑daily dosing, simplifying adherence for the elderly and those with complex polypharmacy regimens. Fifth, real‑world studies continue to demonstrate reduced hospitalizations for heart failure when digoxin is judiciously incorporated into a multimodal regimen that may also include ACE inhibitors, beta‑blockers, and SGLT2 inhibitors. Sixth, its cost‑effectiveness stands unrivaled, offering an accessible option in low‑resource settings where newer therapies remain prohibitively expensive. Seventh, despite its venerable history, digoxin’s safety profile is well‑characterized; with vigilant monitoring of serum levels, electrolytes, and renal function, the risk of toxicity can be mitigated. Eighth, patient preference often leans toward treatments with a proven track record, fostering confidence and adherence. Ninth, clinicians who master its nuanced dosing can tailor therapy to each individual’s hemodynamic milieu, embodying the art of personalized medicine. Tenth, the drug’s role as a bridge therapy-stabilizing patients while newer agents achieve therapeutic effect-cannot be overstated. Eleventh, digoxin’s paucity of drug‑drug interactions, compared to some modern agents, reduces the burden of medication reconciliation. Twelfth, its inclusion in guideline‑directed medical therapy underscores its enduring relevance. Thirteenth, the educational value of understanding digoxin’s physiology enriches medical training, preserving a link to the foundational principles of cardiology. Fourteenth, for clinicians seeking a therapeutic ally that complements rather than replaces other agents, digoxin serves as a versatile adjunct. Finally, remembering that medicine is both science and humanity, the continued, thoughtful use of digoxin exemplifies a respect for the time‑tested tools that have helped countless patients thrive.