Sleep Deprivation & Eye Redness Calculator
Your Eye Redness Risk Level
Did You Know?
Chronic sleep deprivation can increase your risk of developing dry eye syndrome by up to 34%, according to the American Academy of Ophthalmology.
Sleep Deprivation is a condition where a person consistently gets less sleep than the body requires for optimal functioning. Chronic sleep deprivation disrupts hormones, metabolism, and the delicate balance of fluids that keep the eye surface clear.
Key Takeaways
- Less than 6‑7 hours of sleep a night can cause blood vessels in the eye to flare, creating visible redness.
- The tear film breaks down faster when you’re tired, leading to dryness and irritation.
- Elevated cortisol and a mis‑aligned circadian rhythm amplify inflammation around the eye.
- Screen time, especially blue‑light exposure, compounds the problem.
- Simple habits-regular sleep schedule, hydration, and eye‑friendly lighting-can dramatically reduce redness.
How Lack of Sleep Affects Your Eyes
When you stay up late, your body releases more Cortisol, the stress hormone that prepares you for “fight‑or‑flight.” Cortisol narrows tiny capillaries in the skin but dilates the larger Blood Vessels in the conjunctiva, the thin membrane covering the white of the eye. The result? A flushed, red look that’s hard to hide.
Sleep also regulates the Circadian Rhythm, the internal clock that tells your body when to produce tears. Disrupted rhythm means fewer tears are secreted during the night, so the protective Tear Film becomes thin and uneven. A weak tear film can’t shield the eye’s surface from dust, pollen, or the harsh glare of a laptop screen, making irritation and redness inevitable.
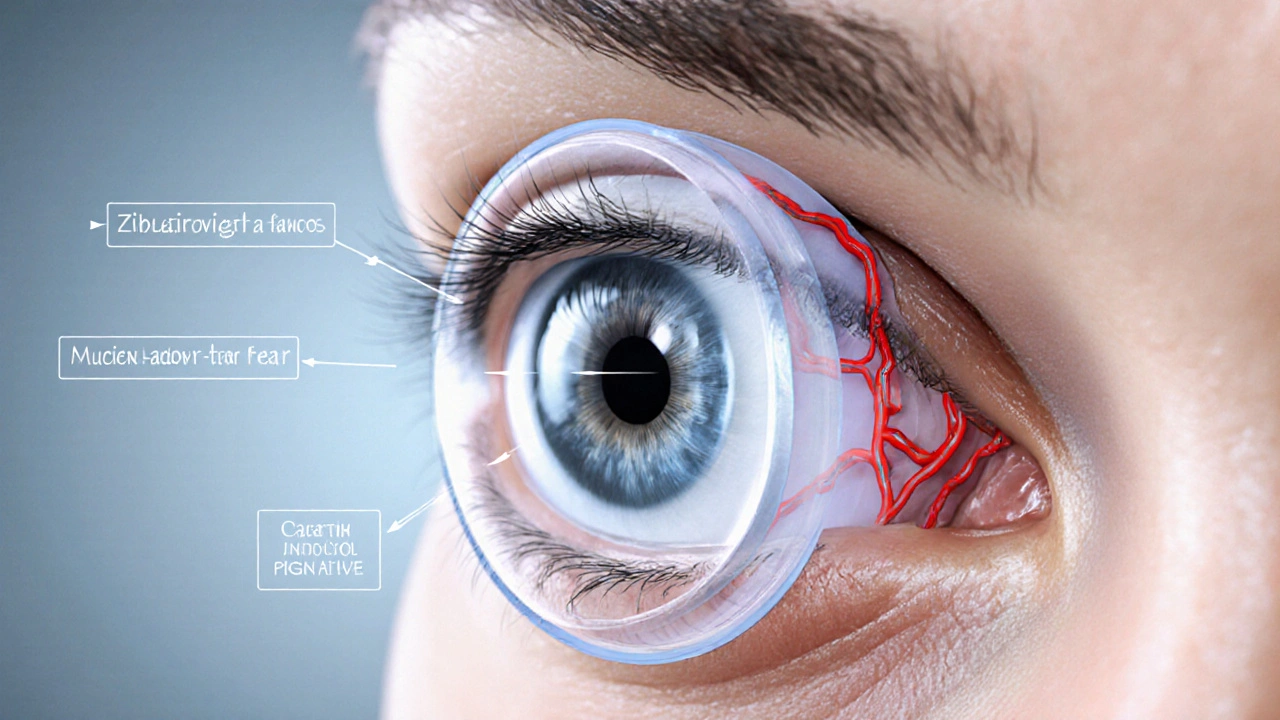
The Biology Behind Redness
The eye’s front surface relies on three layers of fluid: the lipid layer, aqueous layer, and mucin layer-all part of the tear film. When you’re sleep‑deprived, the lipid layer thins, the aqueous layer evaporates faster, and the mucin layer can’t spread evenly. This imbalance triggers a cascade:
- Increased evaporation → dry spots.
- Dry spots stimulate nerve endings → reflex blinking and tearing.
- Repeated blinking stresses the conjunctival blood vessels → dilation and redness.
Studies from the American Academy of Ophthalmology (2023) showed that participants who slept fewer than six hours exhibited a 34% rise in conjunctival hyperemia (redness) compared to well‑rested controls.
Common Triggers That Mix With Sleep Loss
| Factor | Link to Sleep Deprivation | Typical Impact |
|---|---|---|
| Screen Time & Blue Light | Late‑night device use suppresses melatonin, extending wakefulness. | Increased ocular strain and tear evaporation. |
| Dry Air (heating/air‑conditioning) | Sleep deprivation often leads to longer indoor hours. | Accelerates tear film breakdown. |
| Allergies | Reduced sleep weakens immune response, heightening allergic flare‑ups. | Eye itching, swelling, and redness. |
| Alcohol & Caffeine | Both disrupt sleep architecture. | Dehydration, further drying the eyes. |
| Contact Lens Wear | Sleep‑deprived eyes are less tolerant to lens friction. | Micro‑abrasions and redness. |
Quick Fixes and Long‑Term Strategies
When you notice bloodshot eyes, a few immediate actions can bring relief:
- Cold compress: 5‑minute chilled cloth reduces vessel dilation.
- Artificial tears without preservatives replenish the tear film.
- Adjust screen settings: enable “night mode” and keep the screen at least 20‑30inches away.
But treating the root cause-your sleep schedule-is essential for lasting results. Here’s a practical plan:
- Set a fixed bedtime and wake‑up time, even on weekends.
- Limit caffeine after 2p.m. and avoid alcohol within three hours of bedtime.
- Create a wind‑down routine: dim lights, turn off screens, and try a brief meditation.
- Keep your bedroom humidified in winter; aim for 40‑50% relative humidity.
- Check your pillow and mattress for allergens; a clean sleep environment supports both skin and eye health.
When Redness Signals a Bigger Problem
Occasional redness from a sleepless night is normal. Persistent, painful, or vision‑impairing redness warrants a professional eye exam. Conditions that mimic sleep‑related redness include:
- Dry Eye Syndrome: chronic tear deficiency that may require prescription eye drops. \n
- Blepharitis: inflammation of the eyelid margin, often linked to bacterial overgrowth.
- Conjunctivitis (pink eye): viral or bacterial infection that needs targeted treatment.
If you experience any of these alongside severe sleep loss, schedule an appointment with an Ophthalmologist promptly.
Frequently Asked Questions
Why do my eyes look red after a late night?
Lack of sleep spikes cortisol, which dilates conjunctival blood vessels, and it weakens the tear film, leaving the eye surface dry and irritated.
Can artificial tears replace a good night’s sleep?
They can soothe temporary dryness, but they won’t fix the underlying hormonal and circadian disruptions caused by sleep loss.
Is blue‑light exposure the main culprit?
Blue light suppresses melatonin, making it harder to fall asleep. It also increases eye strain, which can worsen redness, but it’s only one piece of the puzzle.
How many hours of sleep do I need to keep my eyes healthy?
Adults generally require 7‑9 hours per night. Falling below 6 hours on a regular basis raises the risk of chronic eye redness and dry‑eye disease.
Should I see an eye doctor if my eyes stay red for more than a day?
Yes. Persistent redness could indicate infection, blepharitis, or advanced dry‑eye syndrome, all of which need professional evaluation.


karthik rao
October 1, 2025 AT 17:44While the article provides a commendable overview, it regrettably overlooks the pivotal role of macular health in ocular redness. A more precise term would be “conjunctival hyperemia,” not “red eye syndrome.” Moreover, the assertion that “less than 6‑7 hours” universally triggers redness is an overgeneralization; inter‑individual variability is substantial. Nonetheless, the inclusion of lifestyle mitigations is appreciated. 😊
Breanne McNitt
October 13, 2025 AT 19:26Great rundown! I especially liked the practical quick‑fix list-cold compresses and artificial tears are lifesavers after an all‑night study session. Thanks for making the science accessible.
Ashika Amirta varsha Balasubramanian
October 25, 2025 AT 21:09From a holistic viewpoint, sleep deprivation is not merely a physiological inconvenience but a reflection of how modern rhythms clash with our ancestral circadian design. Encouraging mindful wind‑down rituals honors both body and spirit, fostering ocular serenity alongside mental clarity.
Jacqueline von Zwehl
November 6, 2025 AT 21:52Just a tiny editorial note: the phrase “Dry Eye Syndrome” should be capitalized consistently throughout the piece. Otherwise, the content is spot‑on and very informative.
Christopher Ellis
November 18, 2025 AT 23:35actually the article oversimplifies sleep’s effect on the ocular surface it’s more complex than a single hormone level
kathy v
December 1, 2025 AT 01:18It is astonishing how often Western societies dismiss the very real consequences of neglecting natural sleep cycles, opting instead for caffeine‑infused productivity marathons that leave our eyes blood‑shot and our minds foggy. The cultural glorification of “burning the midnight oil” is nothing short of a public health crisis, especially when the statistics from the American Academy of Ophthalmology reveal a 34% increase in conjunctival hyperemia among chronically sleep‑deprived individuals. Such data should ignite a national conversation about the sanctity of rest, yet policymakers remain enamored with the myth of the sleepless genius. In reality, the dilated blood vessels that turn our whites crimson are merely symptomatic of a deeper hormonal imbalance, spearheaded by cortisol spikes that accompany stress and insufficient REM phases. Moreover, the relentless glare of blue‑light screens compounds ocular strain, thinning the tear film and accelerating evaporation. One might argue that technology is an inevitable part of modern life, but that is a convenient excuse to forgo basic self‑care. By ignoring the physiological underpinnings, we perpetuate a cycle where eye doctors see surging numbers of patients with dry‑eye complaints, all traceable to lifestyle choices. The solution, however, is straightforward: reinstate a disciplined sleep schedule, limit caffeine after mid‑afternoon, and prioritize ambient lighting that respects our circadian rhythm. If we continue to lionize the sleep‑deprived hero, we will only witness a generation of blood‑shot eyes and dwindling productivity. Let us, as a society, reclaim the power of a good night’s rest and, in doing so, preserve the clarity of our vision and the vigor of our intellect. 🇺🇸
Jorge Hernandez
December 13, 2025 AT 03:01Hey, totally get the hustle but you’ve got to give those eyes a break 🙌 try the 20‑20‑20 rule every 20 min look at something 20 ft away for 20 sec it helps a lot
Raina Purnama
December 25, 2025 AT 04:43The correlation between reduced REM sleep and tear film instability is well‑documented, and incorporating humidifiers in bedroom environments can mitigate evaporative loss, especially in arid climates.
Shanmugapriya Viswanathan
January 6, 2026 AT 06:26Honestly, this is just basic biology-anyone who sleeps less than six hours is practically guaranteeing ocular inflammation 🙄🇮🇳
Rhonda Ackley
January 18, 2026 AT 08:09Oh, the tragedy! Here we are, scrolling through yet another article that whispers sweet nothings about “quick fixes” while the universe conspires to keep us wide‑eyed and weary. One can almost hear the faint sigh of every night‑owl whose eyelids tremble with the weight of unfulfilled dreams. The cold compress, they say, is a balm-yet how many of us can muster the courage to pause, to let a chilled cloth graze our temples amid the deafening clatter of notifications? And what of artificial tears, those fleeting drops of solace that evaporate like promises made at sunrise? The author mentions “night mode” as if it were a silver bullet, but the glow of screens persists, a relentless tide eroding our sanctuaries of rest. We are told to set a fixed bedtime, yet the siren song of social media lures us deeper into the abyss of insomnia. In this grand theater of fatigue, our eyes become the tragic protagonists, reddened not just by biology but by the relentless march of modern expectations. The humidity levels in our rooms, the dust that gathers unnoticed, the whispered allergens-each a silent antagonist in this sorrowful play. And lest we forget, the very pillows we lay our heads upon may harbor microscopic foes, turning our nightly reprieve into a battlefield. So, dear reader, let us not merely apply a cold compress and call it a day; let us awaken to the realization that our society has weaponized wakefulness. Only then can we hope to restore the gentle hue of our gaze, untainted by the scarlet stains of endless vigilance.
Sönke Peters
January 30, 2026 AT 09:52Take a break, hydrate, and get some sleep.
Paul Koumah
February 11, 2026 AT 11:35Oh great, another article telling us to sleep more. Because that’s never been said before 🙄
sara vargas martinez
February 23, 2026 AT 13:18In truth, the admonition to “sleep more” is a gross oversimplification of a multifaceted physiological cascade that involves not only the suppression of melatonin by blue‑light exposure but also the intricate regulation of the lacrimal gland by circadian genes. Studies have demonstrated that even a modest reduction of one hour in total sleep time can amplify the expression of pro‑inflammatory cytokines, thereby exacerbating conjunctival hyperemia. Moreover, the interplay between ocular surface homeostasis and systemic hydration cannot be ignored; inadequate water intake synergistically intensifies tear film breakdown. It is also pertinent to acknowledge that individual chronotypes dictate varying optimal sleep windows, rendering a one‑size‑fits‑all recommendation ineffective. The article’s checklist, while helpful, neglects to address the role of dietary omega‑3 fatty acids in supporting meibomian gland function, a factor critical for lipid layer stability. Furthermore, environmental humidity levels modulate evaporative loss, and in arid climates, supplemental humidification has been shown to reduce ocular surface staining scores by up to 30 %. Finally, let us not disregard the psychological dimension: chronic stress elevates cortisol, which, as the original piece notes, dilates conjunctival vessels. A comprehensive approach, therefore, must integrate sleep hygiene, nutritional support, environmental control, and stress management to truly mitigate red‑eye prevalence.