Acetaminophen Safety Calculator
This calculator helps determine if your acetaminophen (Tylenol) intake is safe based on your liver health and alcohol consumption. Remember: acetaminophen is in over 600 medications including cold remedies, sleep aids, and prescription painkillers.
Every year, more than 500 people in the U.S. die from acetaminophen overdose - not because they tried to hurt themselves, but because they didn’t know they were taking too much. It’s not a mystery drug. It’s in Tylenol. It’s in Vicodin. It’s in Nyquil. It’s even in some cold medicines you grab off the shelf without a second thought. And if you have liver disease, even a normal dose can be dangerous.
Why Acetaminophen Is Riskier Than You Think
Acetaminophen (also called paracetamol) is one of the most common pain relievers in the world. It’s in over 600 different medicines - from sleep aids to flu tablets. Most people think it’s harmless because it’s sold over the counter. But that’s exactly the problem. The body breaks down acetaminophen in the liver. Normally, it’s processed safely. But when you take too much - even just a little over the limit - the liver gets overwhelmed. It starts producing a toxic byproduct called NAPQI. Healthy livers can neutralize this with glutathione, an antioxidant. But if you have liver disease, your glutathione levels are already low. That means even small doses can cause damage. The official maximum daily dose for healthy adults is 4,000 mg. But that number is misleading. For someone with cirrhosis, hepatitis, or fatty liver disease, the safe limit is closer to 2,000 mg. Some experts, including liver specialists at UCI Health, say that even 3,000 mg is too much if you drink alcohol regularly.The Hidden Danger: Multiple Medications
Most overdoses aren’t intentional. They happen when people stack medications without realizing they all contain acetaminophen. Imagine this: You have a headache, so you take two extra-strength Tylenol pills (500 mg each). That’s 1,000 mg. Later, you feel chills and take a cold medicine - say, Nyquil. It also has 325 mg of acetaminophen per dose. You take two doses. That’s another 650 mg. By bedtime, you’ve taken 1,650 mg. Then you wake up with a sore throat, so you take another Tylenol. Now you’re at 2,150 mg. You’re still under 4,000 mg - so you think you’re fine. But you’re not. If you have liver disease, that 2,150 mg could be enough to trigger liver injury. And if you had a glass of wine with dinner? The risk jumps again. The same thing happens with prescription painkillers. Vicodin and Percocet combine acetaminophen with opioids. People think they’re just taking pain meds - they don’t realize each pill might contain 300-650 mg of acetaminophen. Taking four pills a day could put you over 2,600 mg - already above the safe limit for someone with liver damage.What’s the Real Safe Dose?
There’s no one-size-fits-all answer. Here’s what the evidence says:- Healthy adults: Max 4,000 mg per day. But even this is risky if you drink alcohol or take other liver-metabolized drugs.
- People with liver disease: Stick to 2,000 mg per day or less. Some doctors recommend 1,500 mg as a safer target.
- People who drink alcohol regularly: Don’t exceed 2,000 mg per day. Alcohol depletes glutathione and makes the liver more vulnerable.
- Tylenol Extra Strength: The manufacturer’s label says 3,000 mg max per day - not 4,000. Always check the bottle.
- Children: Dose by weight: 10-15 mg per kg every 4-6 hours. Never exceed 80 mg/kg per day. Use the syringe that comes with the medicine - never a kitchen spoon.
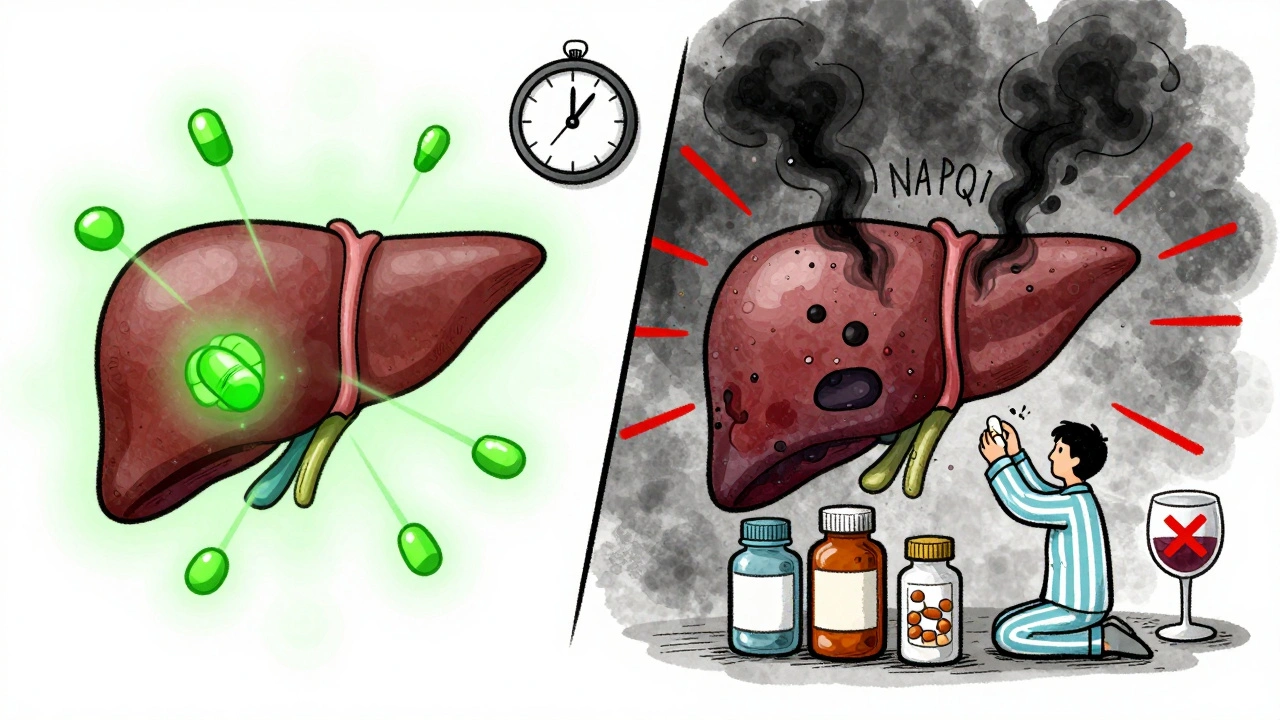
How Alcohol Makes Things Worse
Drinking alcohol while taking acetaminophen is like pouring gasoline on a small fire. Even moderate drinking - one or two drinks a day - increases the risk of liver damage. Alcohol activates the same liver enzyme (CYP2E1) that turns acetaminophen into NAPQI. More enzyme activity = more toxin. At the same time, alcohol reduces your body’s ability to make glutathione. So you’re producing more poison while losing your main defense against it. Studies show that people who drink alcohol regularly can develop liver injury from doses as low as 2,000-3,000 mg per day - well below the standard 4,000 mg limit. That’s why doctors tell patients with liver disease: no alcohol. Ever.What If You’ve Already Taken Too Much?
If you suspect you’ve taken too much acetaminophen - even if you feel fine - don’t wait. Call poison control or go to the ER. The antidote, acetylcysteine (NAC), works best if given within 8 hours of overdose. But it can still help up to 16 hours later. Waiting until you feel sick is too late. Liver damage often shows up as nausea or fatigue - symptoms that feel like the flu. By the time jaundice or confusion appears, it’s already serious. The standard NAC treatment is:- Oral: 140 mg/kg first dose, then 70 mg/kg every 4 hours for 17 doses.
- IV: 150 mg/kg over 15 minutes, then 50 mg/kg over 4 hours, then 100 mg/kg over 16 hours.
Who’s at Highest Risk?
Not everyone who takes acetaminophen is equally at risk. These groups need extra caution:- People with chronic liver disease: Hepatitis B or C, cirrhosis, NAFLD - all increase vulnerability.
- Chronic alcohol users: Even if they don’t have diagnosed liver damage, their livers are already stressed.
- People on seizure meds or TB drugs: Medications like phenytoin, carbamazepine, or rifampin speed up acetaminophen metabolism, increasing toxin production.
- Malnourished or elderly patients: Lower glutathione stores mean less protection.
- Pregnant women: Acetaminophen is still considered safe in pregnancy, but only if dosed correctly. Always check with your doctor.

How to Stay Safe
Here’s what you should do right now:- Check every medicine label. Look for “acetaminophen,” “APAP,” or “paracetamol.” It’s on almost every pain and cold medicine.
- Add up all sources. If you’re taking more than one product, write down how much acetaminophen each contains. Total it.
- Set a daily cap. If you have liver disease, stick to 2,000 mg or less. If you drink, stick to 2,000 mg or less.
- Avoid alcohol completely. No exceptions.
- Use the lowest effective dose. Don’t take 650 mg if 325 mg works.
- Ask your pharmacist. When you get a new prescription, ask: “Does this contain acetaminophen?”
- Keep a medication log. Write down what you take and when. It helps you avoid double-dosing.
What About Alternatives?
If you have liver disease and need pain relief, what can you use instead?- Physical therapy, heat, or ice - often just as effective for joint or muscle pain.
- Topical creams like lidocaine or capsaicin - no liver metabolism.
- NSAIDs like ibuprofen - but be careful. They can harm kidneys and raise blood pressure. Not always safer for liver patients.
- Non-drug options: Meditation, acupuncture, or cognitive behavioral therapy for chronic pain.
Final Reality Check
Acetaminophen isn’t evil. It’s a useful medicine. But it’s not harmless. It’s like a chainsaw - great when used right, deadly when misused. And because it’s so common, we forget how dangerous it can be. If you have liver disease, your liver is already working hard. Don’t ask it to handle more than it can. Even a single extra pill can tip the balance. The numbers don’t lie: 1,600 cases of acute liver failure each year in the U.S. are caused by acetaminophen. Half of those are unintentional. That’s preventable. Start today. Read your labels. Talk to your doctor. Cut back. Your liver will thank you.Can I take Tylenol if I have fatty liver disease?
Yes, but only in very low doses - no more than 2,000 mg per day, and ideally less. Fatty liver disease reduces your liver’s ability to detoxify acetaminophen. Even normal doses can cause harm. Always check with your doctor before taking any pain reliever.
Is it safe to take acetaminophen with alcohol?
No. Never. Even one drink with acetaminophen increases the risk of liver damage. Alcohol and acetaminophen both stress the liver and reduce its protective antioxidants. The combination can cause serious injury - even if you don’t feel sick. If you drink regularly, avoid acetaminophen completely.
What happens if I accidentally take too much?
Don’t wait for symptoms. Call poison control or go to the ER immediately. Liver damage from acetaminophen can take 24-48 hours to show up. By then, it may be too late. The antidote, acetylcysteine, works best within 8 hours - but can still help up to 16 hours after overdose. Time matters.
How do I know if a medicine has acetaminophen in it?
Look for “acetaminophen,” “APAP,” or “paracetamol” on the label. It’s often listed in small print. Prescription drugs like Vicodin or Percocet contain it too. If you’re unsure, ask your pharmacist. Never assume a cold medicine or sleep aid is safe just because it doesn’t say “Tylenol.”
Can children with liver disease take acetaminophen?
Children with liver disease should avoid acetaminophen unless directed by a pediatric liver specialist. Dosing is based on weight, but their livers are more sensitive. Even standard pediatric doses can be dangerous. Always use the syringe provided - never a household spoon - and never exceed the doctor’s recommended amount.
Is there a blood test to check for acetaminophen toxicity?
Yes. A serum acetaminophen level test can show how much is in your blood. But it’s only useful if taken 4-24 hours after ingestion. Doctors use the Rumack-Matthew nomogram to interpret the results and decide if treatment is needed. If you suspect an overdose, don’t wait for the test - start treatment immediately if you’re within the 8-hour window.
What are the early signs of acetaminophen liver damage?
Early signs are vague: nausea, vomiting, loss of appetite, and tiredness - symptoms that look like the flu. By the time your skin or eyes turn yellow (jaundice), your liver is already damaged. If you’ve taken acetaminophen and feel unusually unwell, get checked - even if you don’t think you took too much.
Can liver damage from acetaminophen be reversed?
If caught early - within 8-10 hours of overdose - the liver can often repair itself completely with acetylcysteine treatment. But if damage is advanced, it can lead to acute liver failure, requiring a transplant. Prevention is far better than treatment.
If you or someone you know has liver disease, make acetaminophen safety a priority. Read labels. Track doses. Talk to your doctor. One extra pill might seem harmless - but for a damaged liver, it could be the difference between recovery and crisis.







Casey Lyn Keller
December 2, 2025 AT 14:42Storz Vonderheide
December 2, 2025 AT 21:45Kevin Estrada
December 4, 2025 AT 08:12Colin Mitchell
December 4, 2025 AT 11:15Stacy Natanielle
December 5, 2025 AT 19:35kelly mckeown
December 7, 2025 AT 18:44Tom Costello
December 9, 2025 AT 17:40dylan dowsett
December 10, 2025 AT 07:14Susan Haboustak
December 11, 2025 AT 00:42Chad Kennedy
December 12, 2025 AT 05:42