Warfarin-Estrogen Interaction Calculator
Estrogen-Warfarin Interaction Calculator
Estimate how estrogen therapy may affect your warfarin dose. Based on article data showing 10-25% dose adjustments for INR monitoring.
Recommended Warfarin Dose Adjustment
Monitor INR at 3, 7, and 14 days after starting estrogen therapy.
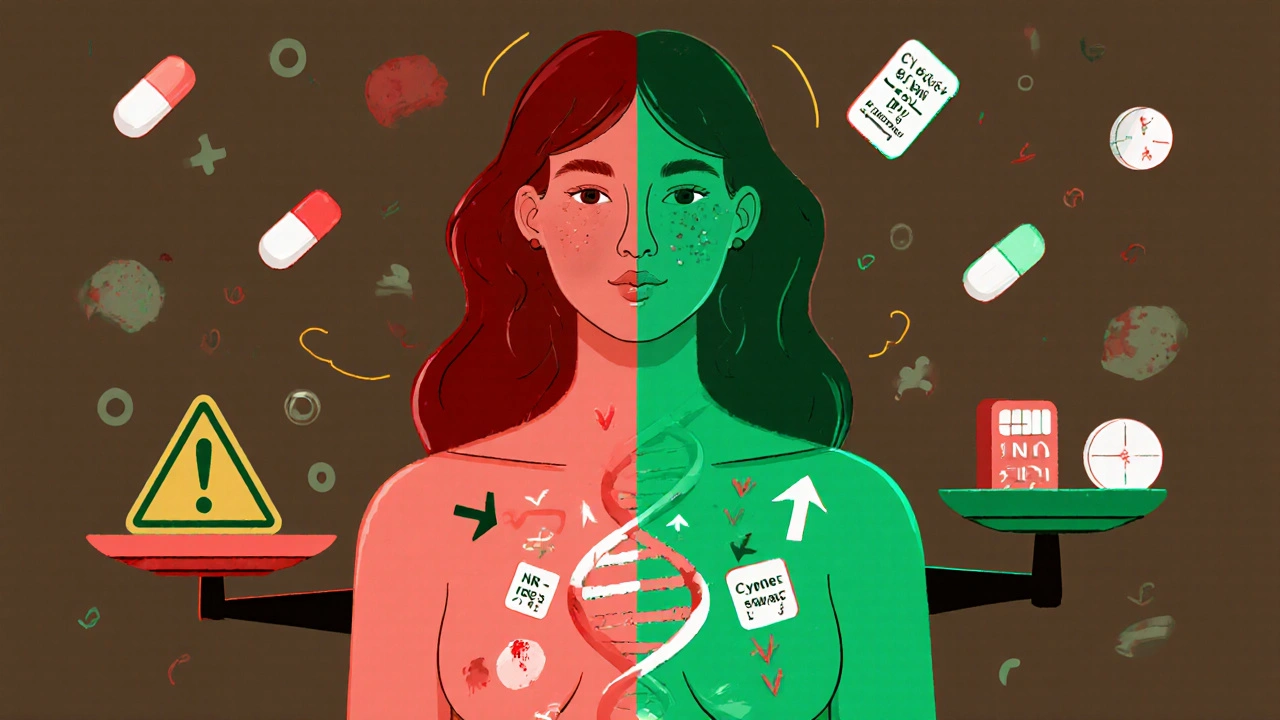
When you're on warfarin, even small changes in your routine can shake up your blood thinning levels. That’s why so many people get surprised when their INR jumps or drops after starting birth control, hormone replacement therapy, or even a menopause patch. It’s not just about food or alcohol - estrogen can quietly mess with how warfarin works in your body. And if you’re a woman between 18 and 45 taking both, you’re at nearly twice the risk of your INR going too high - which means a higher chance of dangerous bleeding.
How Estrogen Changes Warfarin’s Effect
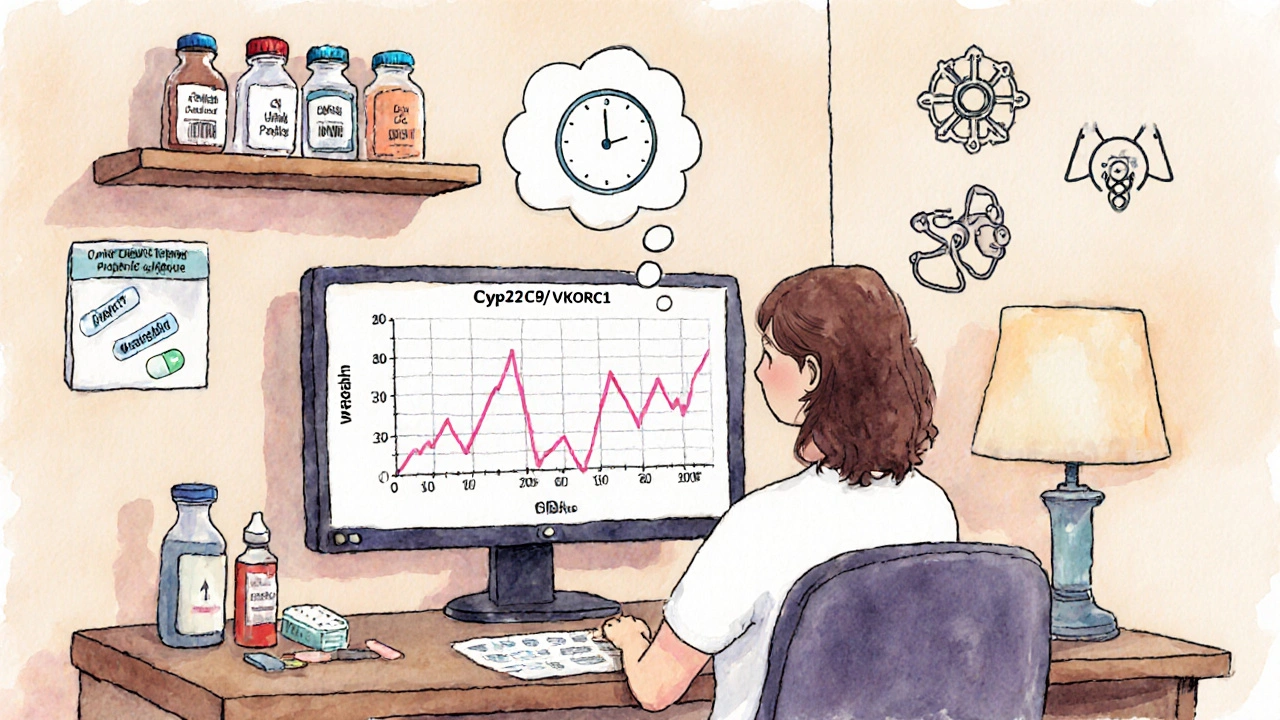
Warfarin doesn’t work the same way for everyone. It’s broken down in the liver by enzymes called CYP450, especially CYP2C9, CYP1A2, and CYP3A4. Estrogen compounds - whether natural like estradiol or synthetic like ethinyl estradiol - can either speed up or slow down these enzymes. That’s the core of the problem.
Here’s the twist: not all estrogens act the same. Natural estradiol, often used in hormone replacement therapy, tends to induce certain enzymes, which means your body clears warfarin faster. That can make your INR drop - sometimes below the safe range - increasing your risk of clots. On the other hand, synthetic ethinyl estradiol, found in most birth control pills, tends to inhibit CYP1A2 and CYP2C19. That slows warfarin breakdown, letting it build up in your blood. INR spikes. Bleeding risk rises.
This isn’t theoretical. A 2009 case study followed a 28-year-old woman whose INR jumped from 2.4 to 4.3 within five days of starting a combined oral contraceptive. Her warfarin dose had to be cut from 5 mg to 3.5 mg. Another patient in a 2022 Reddit thread reported her INR went from 2.5 to 3.8 after starting HRT. Her doctor lowered her dose by 20%. But then there’s the opposite - some women see their INR drop when they start birth control. That’s because estrogen’s effect isn’t always predictable. It depends on the type, dose, and your genetics.
Why Genetics Matter More Than You Think
If your body handles warfarin differently than your neighbor’s, it’s not just luck - it’s your DNA. About 30% of people carry a variant of the CYP2C9 gene (like *2 or *3) that makes them break down warfarin much slower. If you’re one of them and you add estrogen, your INR could climb dangerously high even with a small dose change.
Then there’s VKORC1 - the gene that controls how sensitive your blood is to warfarin. If you have the -1639G>A variant, you need 30-50% less warfarin just to stay in range. Add estrogen on top of that, and you’re playing Russian roulette with your INR.
That’s why the International Warfarin Pharmacogenetics Consortium developed a dosing algorithm that includes these genetic markers. In a study of over 5,000 patients, using genetic data improved dosing accuracy by 30-35%. It’s not standard everywhere yet - but if you’ve had unstable INR levels before, ask your doctor about testing. It could save you from hospital visits.
How Estrogen Compares to Other Drug Interactions
Warfarin has dozens of dangerous interactions. Antibiotics like ciprofloxacin or trimethoprim-sulfamethoxazole can spike INR by 2.5 to 3 times. Antidepressants like fluoxetine? That doubles your bleeding risk. Amiodarone? That can force you to cut your warfarin dose by 40%.
Estrogen interactions? They’re usually quieter. INR changes tend to be in the 0.5 to 1.5 range - not as dramatic, but still dangerous. Why? Because warfarin has such a narrow window. Going from 2.2 to 3.7 might seem small, but it’s enough to turn a minor bruise into internal bleeding. A 2010 analysis of 15,317 patients found women on estrogen-based contraceptives had 1.8 times the risk of INR over 4.0 compared to those not taking estrogen.
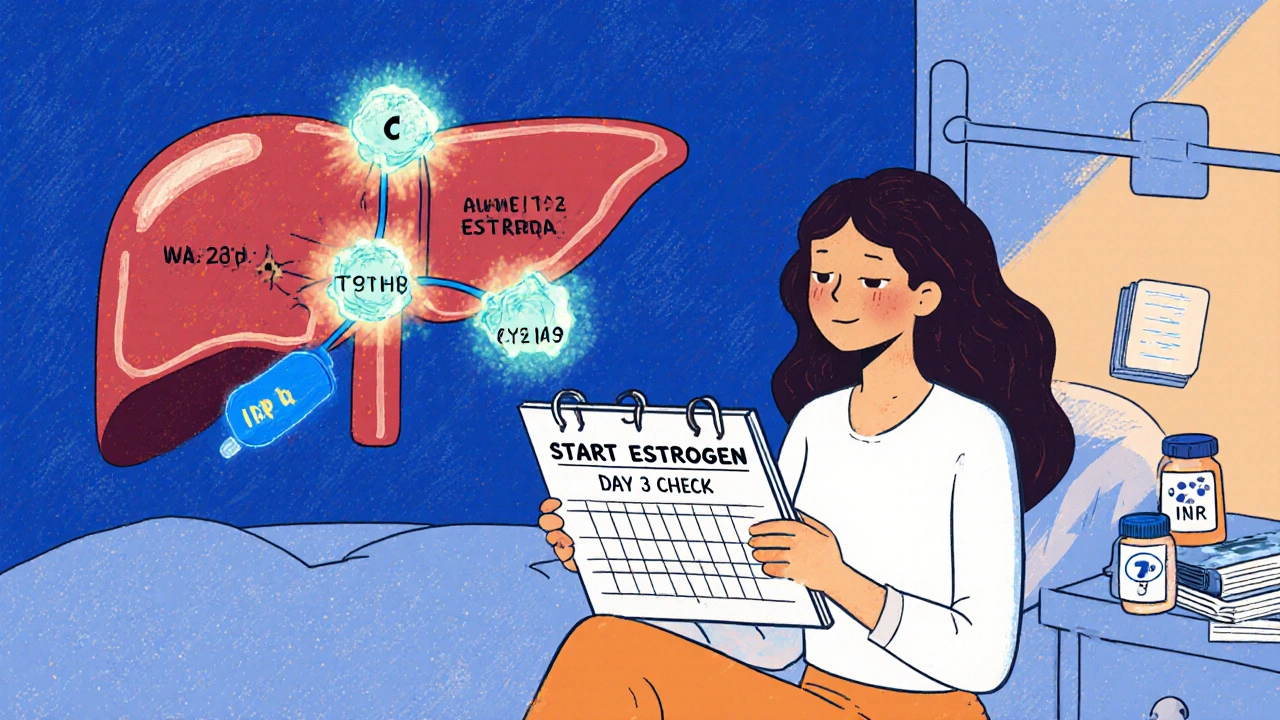
And here’s the catch: while antibiotics and antifungals cause immediate spikes, estrogen effects can be delayed. It might take 3 to 7 days for your INR to shift after starting or stopping estrogen. That’s why monitoring isn’t optional - it’s essential.
What Doctors Actually Do in Practice
Most anticoagulation clinics follow the same playbook when estrogen enters the picture:
- Check INR before starting estrogen therapy.
- Test again within 3 to 5 days after starting.
- Test again at 7 to 14 days.
- Adjust warfarin by 10-25% based on the trend - not just one number.
Pharmacists surveyed by the Anticoagulation Forum in 2021 reported managing at least one estrogen-warfarin interaction every year in 68% of cases. Nearly half of them adjusted warfarin doses by 15-25%. The key? Don’t assume the change is due to diet, illness, or missed pills. Ask: Did something hormonal start or stop?
Discontinuing estrogen is just as risky. If you stop birth control or HRT, your body may suddenly start metabolizing warfarin faster. INR can drop - fast. That’s when clots form. You need the same monitoring schedule after stopping as you do when starting.
What You Should Do Right Now
If you’re on warfarin and considering estrogen - whether for birth control, menopause, or gender-affirming care - here’s your action plan:
- Don’t start or stop estrogen without talking to your anticoagulation team.
- Ask for an INR check 3 days before starting estrogen.
- Request follow-up INR tests at days 3, 7, and 14 after starting.
- Keep a log: note your dose, your estrogen product, and any symptoms (bruising, nosebleeds, dark stools).
- Ask if genetic testing is right for you - especially if your INR has been hard to control.
And if you’re already on both? Don’t panic. But do get your INR checked now - even if you feel fine. A single test can catch a slow drift before it becomes a crisis.
Why Warfarin Is Still Used - Even With DOACs Around
You’ve probably heard about the newer blood thinners - apixaban, rivaroxaban, dabigatran. They don’t interact with estrogen the same way. That’s why they’re popular. In 2023, 68% of oral anticoagulant prescriptions in the U.S. were for these direct oral anticoagulants (DOACs), up from just 15% in 2013.
But warfarin isn’t going away. It’s still the only option for people with mechanical heart valves. It’s preferred for those with antiphospholipid syndrome or severe kidney disease. An estimated 1.8 million Americans will still be on warfarin in 2030. That means estrogen-warfarin interactions aren’t a fading concern - they’re a growing one.
And while DOACs are easier in many ways, they’re not perfect. They’re expensive. They don’t have a reliable reversal agent for all types. And they still interact with other drugs - just not estrogen. So if you’re on warfarin, you’re not alone. And you need to be smart about what you add to your regimen.
The Bottom Line
Estrogen doesn’t always make warfarin dangerous - but it can. And the risk isn’t the same for everyone. It depends on the type of estrogen, your genetics, your dose, and how your body responds. The good news? You can manage it. You don’t need to stop your hormones. You don’t need to fear your blood thinner. You just need to know when to test, when to adjust, and who to talk to.
Don’t wait for a bleeding episode or a clot to teach you this lesson. Get your INR checked. Ask questions. Track your numbers. And remember - your doctor isn’t the only expert here. You’re the one living with this every day. Your observations matter. Your questions matter. Your safety depends on it.
Can I take birth control pills while on warfarin?
Yes, but not without close monitoring. Combined oral contraceptives (containing ethinyl estradiol) can increase your INR, raising bleeding risk. Your doctor should check your INR before starting, then again at 3, 7, and 14 days after. Dose adjustments of 10-25% are common. Progestin-only pills are generally safer but still require monitoring.
Why did my INR drop after starting HRT?
Natural estrogen (like estradiol) can speed up how fast your liver breaks down warfarin, especially if you’re using patches or gels. This lowers your INR and increases clot risk. It’s less common than INR spikes, but it happens. If your INR drops below your target range, your warfarin dose may need to be increased - not decreased.
Do I need genetic testing if I’m on warfarin and estrogen?
It’s not required, but it’s highly recommended if you’ve had unstable INR levels, frequent dose changes, or bleeding/clotting events. Variants in CYP2C9 and VKORC1 explain why some people need much lower warfarin doses. Testing can help predict how estrogen will affect you and reduce trial-and-error dosing.
How long does it take for estrogen to affect my INR?
It usually takes 3 to 7 days for changes in estrogen levels to affect warfarin metabolism. That’s why INR checks at day 3, 7, and 14 are standard. Don’t wait for symptoms - test early. The same applies when you stop estrogen - effects can linger for up to two weeks.
Are there safer alternatives to estrogen for women on warfarin?
For birth control, progestin-only pills, IUDs (like Mirena), or implants are safer options with minimal interaction risk. For menopause, non-hormonal treatments like gabapentin or SSRIs can help with hot flashes. If hormones are necessary, low-dose transdermal estradiol may be preferred over oral pills, but still requires monitoring. Always discuss alternatives with your doctor.



Mansi Gupta
October 30, 2025 AT 16:15This is such an important post. I’ve been on warfarin for atrial fibrillation and started HRT last year-my INR went from 2.6 to 3.9 without any other changes. My doctor didn’t even ask about hormones until I mentioned it. I wish more providers knew this.
Erin Corcoran
October 31, 2025 AT 08:29OMG YES!! 😍 I’m on warfarin + birth control and my pharmacist literally printed me a flowchart. CYP2C9 inhibition + ethinyl estradiol = 🚨 INR spike city. They adjusted my dose by 20% and now I’m golden. Don’t ignore the hormonal factor-it’s not just ‘diet’ or ‘alcohol’ anymore. 🙌
shivam mishra
November 1, 2025 AT 12:44As a clinical pharmacist in Delhi, I’ve seen this 5+ times in the last year. Most patients assume their INR changes are due to turmeric or garlic-but no, it’s the estrogen patch they started for hot flashes. Natural estradiol induces CYP3A4, so INR drops. Synthetic EE inhibits CYP1A2, so INR rises. It’s not random-it’s pharmacokinetics. Always check before and at 3, 7, 14 days. Genetic testing? If you’ve had 3+ INR fluctuations, get it done. Saves lives.
Scott Dill
November 2, 2025 AT 20:46Bro. I was on warfarin for a pulmonary embolism and started estrogen for gender transition. My INR went from 2.3 to 4.1 in 4 days. I thought I was just stressed or eating too much kale. Turns out? Estrogen. My hematologist was like ‘Ohhhhh that’s why.’ Now I get tested every 10 days. This post saved my life. Thank you.
Arrieta Larsen
November 4, 2025 AT 06:29My mom’s on warfarin and started HRT. Her INR dropped to 1.1. They increased her dose, but she got a clot. Now she’s on apixaban. Estrogen + warfarin is a minefield. If you can switch to a DOAC, do it. No joke.
Mike Gordon
November 6, 2025 AT 06:11My INR went from 2.5 to 3.7 after I started the pill. No symptoms. No bruising. Just a routine test. I almost missed it. Now I log everything. Dose. Pill. INR. Mood. Sleep. Coffee. Everything. Turns out estrogen + warfarin isn’t a myth-it’s a silent timer waiting to go off.
Kathy Pilkinton
November 7, 2025 AT 22:09So let me get this straight-you’re telling me women have to jump through 17 hoops just to take birth control while on a life-saving drug… but men can take testosterone with zero monitoring? Hmm. Fascinating. How many more ‘quiet’ interactions are we ignoring because they involve hormones? 🙄
Holly Dorger
November 8, 2025 AT 03:32hi. i’ve been on warfarin since 2020 and started transdermal estradiol last year. i didn’t know about the 3-7-14 rule. i just got my inr checked once after starting. it was fine. but then 3 weeks later i had a nosebleed that wouldn’t stop. turned out my inr was 5.2. i’m so glad i found this. i’m going to ask my doctor about genetic testing now. thank you for writing this. it’s so clear.
Amanda Nicolson
November 9, 2025 AT 11:42Imagine this: you’re a woman in your 30s, on warfarin after a DVT, and your doctor says, ‘Just avoid kale and alcohol.’ Meanwhile, you’re on birth control, and your INR is slowly climbing like a slow-motion horror movie. No one asks about your hormones. No one connects the dots. You start getting nosebleeds every morning. You think it’s stress. You think it’s dry air. You think you’re just ‘being dramatic.’ Until one day, you’re in the ER with a hemorrhage and your INR is 6.8. And then, finally, someone says, ‘Did you start anything new?’ And you say, ‘Oh, the pill.’ And suddenly, it all makes sense. This isn’t just medical advice. It’s a lifeline for the invisible, ignored, and underestimated. Please. Share this. Someone’s life depends on it.