For decades, benzodiazepines have been one of the most common prescriptions for anxiety, panic attacks, and insomnia. They work fast-sometimes in under an hour. That’s why so many people turn to them when they’re overwhelmed, can’t sleep, or feel like their mind is racing out of control. But what most people don’t realize is that these pills, while effective in the short term, come with risks that can change your life if you use them too long.
How Benzodiazepines Actually Work
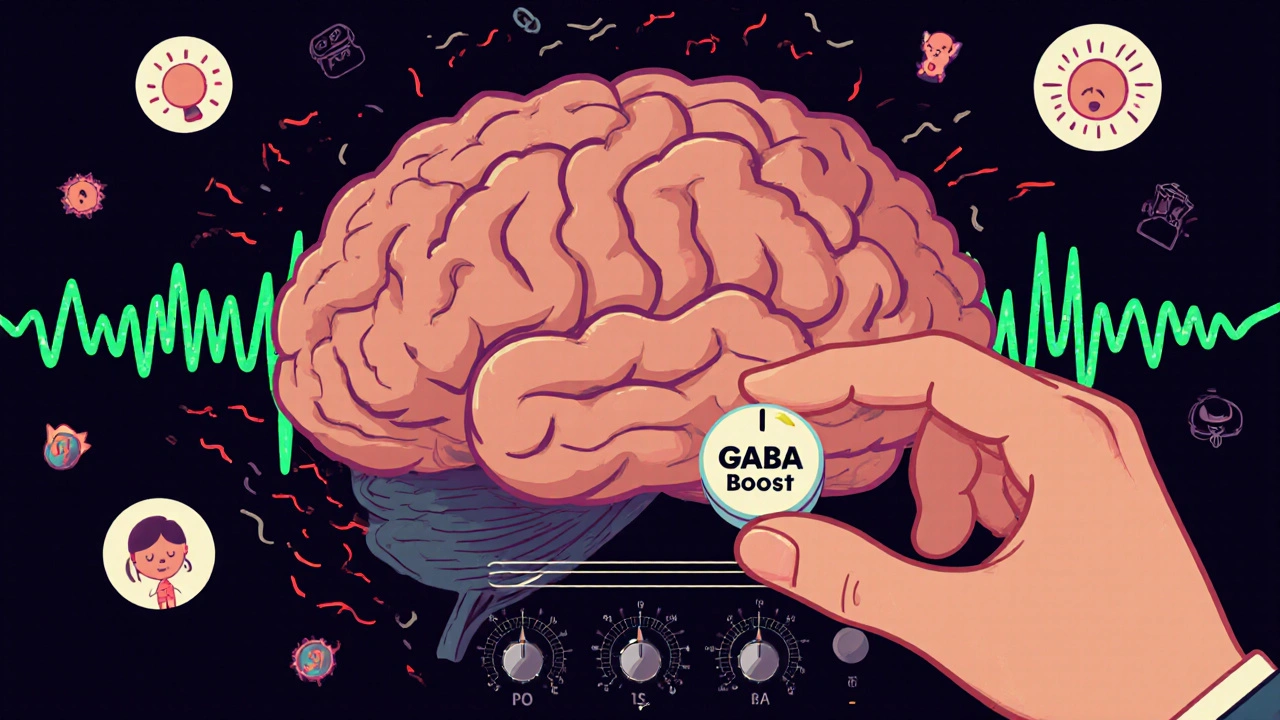
Benzodiazepines don’t just make you feel calm. They physically change how your brain works. They boost the effect of a natural chemical called GABA, which slows down overactive nerve signals. Think of your brain like a radio with the volume turned too high. Benzodiazepines turn the volume down. That’s why they help with panic, muscle spasms, seizures, and even alcohol withdrawal.
Not all benzodiazepines are the same. Some wear off quickly-like triazolam, used for sleep. Others last for days, like diazepam, often prescribed for anxiety or muscle spasms. The length of time they stay in your body matters. Short-acting ones are better for sudden insomnia because they don’t leave you groggy the next day. Long-acting ones are used when you need steady control over anxiety or to manage withdrawal from alcohol.
Doctors choose specific drugs based on what you need. Alprazolam (Xanax) for panic attacks. Lorazepam (Ativan) for acute anxiety or before surgery. Diazepam (Valium) for seizures or muscle tension. Each has a job. But they all share the same core mechanism: calming the nervous system.
The Real Benefits: When They Make a Difference
There’s no denying benzodiazepines work when you need them most. If you’re having a panic attack so bad you can’t breathe, a single dose of alprazolam can bring you back to earth in minutes. For someone with severe insomnia after a trauma, a short course of temazepam can restore sleep when nothing else does.
Emergency rooms rely on them. In status epilepticus-a seizure that won’t stop-midazolam is often the first line of defense. It stops the brain from firing uncontrollably. In intensive care units, it helps sedate patients on ventilators. For people going through alcohol withdrawal, diazepam prevents dangerous tremors, hallucinations, and seizures.
Compared to antidepressants like SSRIs, which can take weeks to kick in, benzodiazepines are instant. That’s why they’re still used, even as guidelines tighten. A 2023 study in JAMA Internal Medicine found that combining them with cognitive behavioral therapy reduced long-term dependence by 58%. That’s the sweet spot: short-term help while building lasting skills.
The Hidden Risks: Dependence Isn’t Rare-It’s Common
Here’s the problem most people don’t see coming: your brain adapts. After just a few weeks of regular use, your body starts to need the drug to feel normal. That’s physical dependence. It’s not addiction. It’s biology.
Studies show 30% to 50% of people who take benzodiazepines daily for more than four weeks develop dependence. That’s not a small number. That’s nearly half. And it doesn’t mean you’re weak or irresponsible. It just means your brain changed.
Withdrawal isn’t just feeling anxious again. It can be terrifying. People report rebound insomnia worse than before, muscle spasms, heart palpitations, tingling in the hands, and even seizures. One user on a support forum described it as “your body screaming for the drug you didn’t think you were addicted to.”
And it’s not just about stopping cold turkey. Even tapering too fast can trigger symptoms. The Ashton Manual-the gold standard for safe withdrawal-says most people need 3 to 6 months to get off long-term benzos. Some need over a year. That’s not a quick fix. That’s a slow, careful process with medical support.

Who’s Most at Risk?
Not everyone who takes benzodiazepines ends up dependent. But certain groups are far more vulnerable.
- People over 65: The American Geriatrics Society warns against using them in older adults. They increase fall risk by 50% and raise dementia likelihood by 32% with long-term use.
- Those with a history of substance use: Even if it’s alcohol or smoking, past dependence makes you more likely to misuse benzos.
- Women: In the U.S., women get 8.3 prescriptions per 100 people-nearly double the rate for men. Why? Often because anxiety disorders are diagnosed more frequently in women, and doctors reach for quick solutions.
- People using them for months or years: The longer you take them, the harder it is to stop. After 90 days, your risk of dependence jumps sharply.
And it’s not just about dosage. It’s about duration. Even low doses become risky if taken daily for more than a few weeks.
What About Alternatives?
There are better long-term options. For anxiety, SSRIs and SNRIs (like sertraline or venlafaxine) take longer to work-4 to 6 weeks-but they don’t cause dependence. For insomnia, cognitive behavioral therapy for insomnia (CBT-I) is more effective over time than any sleep pill.
CBT-I teaches you how to break the cycle of lying awake, worrying about sleep, and then getting more anxious. It’s not magic. It’s work. But studies show it works for 70% of people-and the benefits last for years.
For acute anxiety, mindfulness, breathing exercises, and even regular exercise can be powerful tools. They don’t give you instant relief, but they rewire your brain’s stress response over time.
And yes, there are “Z-drugs” like zolpidem (Ambien) for sleep. But they carry the same dependence risks as benzodiazepines. They’re not safer-just newer.
How to Use Them Safely (If You Must)
If your doctor prescribes a benzodiazepine, ask these questions:
- What’s the goal? Is this for a panic attack next week, or for daily use for months?
- How long should I take it? Get a clear end date-no vague “as needed” without limits.
- What’s the plan if I want to stop? Don’t wait until you’re stuck.
- Are there non-drug options I can try alongside this?
Never take more than prescribed. Never mix with alcohol or opioids. Never stop suddenly. And if you’ve been on them for more than a month, talk to your doctor about tapering before you even think about quitting on your own.
Some clinics now use electronic alerts to flag prescriptions over 90 days. Kaiser Permanente cut long-term benzo use by 37% just by adding that system. That’s the kind of change that saves lives.
The Bigger Picture: Why This Matters Now
In 2021, over 76 million benzodiazepine prescriptions were filled in the U.S. That’s more than 12% of adults. In France, the rate is six times higher. Globally, the market is worth over $1.7 billion-and growing.
But the tide is turning. The FDA added a boxed warning in 2020 about abuse and dependence. The UK’s NICE guidelines now say don’t start benzodiazepines for anxiety at all. Australia and Canada have tightened prescribing rules too.
The future isn’t about banning them. It’s about using them like a fire extinguisher-not a daily drink. For panic attacks, seizures, or surgery, they’re lifesavers. For chronic anxiety or insomnia? There are safer, longer-lasting solutions.
It’s not about fear. It’s about balance. You deserve relief. But you also deserve to stay in control of your own brain.
Can you get addicted to benzodiazepines if you take them as prescribed?
Yes. Addiction implies compulsive use despite harm, but physical dependence can happen even when you follow your doctor’s orders. After just 4 weeks of daily use, your brain adapts to the drug. Stopping suddenly can cause withdrawal symptoms like anxiety, insomnia, tremors, or seizures. This isn’t weakness-it’s biology. That’s why guidelines recommend short-term use only.
How long is it safe to take benzodiazepines?
Most medical organizations, including the American Psychiatric Association and the NHS, recommend no more than 2 to 4 weeks for anxiety and insomnia. Beyond that, tolerance builds, meaning you need higher doses for the same effect. Long-term use increases dependence risk dramatically and reduces the medication’s effectiveness. For chronic conditions, non-drug therapies like CBT are more effective and safer.
What are the signs of benzodiazepine dependence?
Signs include needing higher doses to feel the same effect, feeling anxious or irritable when the drug wears off, experiencing trouble sleeping or muscle tension without it, and having strong urges to take it even when you don’t need it. If you’ve tried to stop and felt worse-like panic, shaking, or dizziness-you’re likely dependent. Don’t try to quit alone.
Can benzodiazepines cause memory problems?
Yes. Benzodiazepines can cause anterograde amnesia-meaning you can’t form new memories while taking them. People report forgetting conversations, driving to places and not remembering how they got there, or missing chunks of time during the day. This is more common with higher doses or long-acting versions like diazepam. It’s not just about being sleepy-it’s a direct effect on brain memory circuits.
Is it possible to stop taking benzodiazepines safely?
Yes-but only with medical supervision. Cold turkey can trigger seizures or severe withdrawal. The safest method is a slow taper, reducing your dose by 5-10% every 1-2 weeks. For long-term users, this can take months or even over a year. The Ashton Manual is the most trusted guide for this process. Support from a doctor, therapist, or peer group improves success rates dramatically.
Are there any benzodiazepines that are safer than others?
No benzodiazepine is truly safer in the long term. All carry dependence risk. But short-acting ones like lorazepam or oxazepam are easier to taper because they leave the body faster. Long-acting ones like diazepam can be used for tapering because they provide steadier levels, reducing withdrawal spikes. The key isn’t which drug-it’s how long you use it and how you stop.







Scott Macfadyen
November 18, 2025 AT 03:19Benzodiazepines are like emotional duct tape-works great until you try to peel it off and your skin comes with it. I saw my uncle go from ‘just taking one at night’ to needing three just to sit still. No one warned him. No one told him it wasn’t a sleep aid-it was a trap disguised as relief.
Chloe Sevigny
November 18, 2025 AT 20:53The pharmacological mechanism of GABAergic potentiation, while efficacious in acute neuromodulatory contexts, engenders neuroadaptive tolerance that fundamentally alters synaptic homeostasis. The clinical literature is unequivocal: prolonged exposure induces downregulation of benzodiazepine-sensitive GABA-A receptor subunits, rendering endogenous inhibitory neurotransmission insufficient without exogenous ligand support. This is not addiction-it is neurobiological recalibration. The real failure lies in prescriptive inertia, not patient compliance.
Denise Cauchon
November 20, 2025 AT 02:31Canada’s got it right-we don’t hand out these chemical pacifiers like candy. In the US, they’re giving them out like free samples at Costco. My cousin’s mom was on Xanax for 8 years because her doctor said ‘it’s fine.’ She’s now in rehab because her brain forgot how to chill without a pill. Shame on the system that lets this happen. 🇨🇦 vs 🇺🇸-it’s not even a contest.
Andrea Johnston
November 22, 2025 AT 00:18People think they’re in control until they’re not. I’ve seen too many smart, capable people become hollowed-out zombies on benzos. They say ‘I’m just taking it as prescribed’ like that’s some magical shield against biology. It’s not. It’s a countdown clock. And if your doctor didn’t give you an exit strategy, they didn’t care enough to save you from yourself.
Victoria Malloy
November 22, 2025 AT 16:44I was on lorazepam for 6 weeks after my mom died. I didn’t realize I was dependent until I tried to stop and felt like my bones were vibrating. I tapered slowly with my therapist’s help-it took 5 months. It was brutal, but I’m glad I did it. You can heal without pills. It just takes time and patience.
Alex Czartoryski
November 24, 2025 AT 09:45Let’s be real-CBT-I is great and all, but when you’ve been awake for 72 hours and your brain is screaming, you don’t care about sleep hygiene. You want a pill that shuts it off. That’s not weakness. That’s survival. The problem isn’t the drug-it’s that we don’t have better emergency tools. Benzos are the fire extinguisher because we never built the fire alarm system.
Gizela Cardoso
November 25, 2025 AT 22:45My dad was prescribed Valium after his heart surgery. He took it for 18 months. We didn’t realize he was dependent until he started forgetting our names. He tapered with a neurologist and now sleeps better than he has in 20 years. It’s not about avoiding benzos-it’s about treating them like explosives, not aspirin.
kim pu
November 26, 2025 AT 10:04they said 'short term' but then the scrip auto-renewed for 3 yrs. i was just trying to sleep, not become a human ghost. now i'm 4 months into tapering and my dreams are like horror movies. also why is the ashton manual not a textbook??