Why Spacers Are a Game-Changer for Kids with Asthma
Many parents think their child’s inhaler is enough. But if your child is using a metered-dose inhaler (MDI) without a spacer, they’re probably not getting the full dose of medicine. That’s because kids-especially those under five-can’t coordinate pressing the inhaler and breathing in at the same time. A spacer solves this. It’s a simple plastic tube that attaches to the inhaler and holds the medicine like a little cloud until the child breathes it in. No timing needed. No rushing. Just breathe normally.
Studies show that with a spacer, up to 73% of children use their inhaler correctly. Without one, that number drops to under 30%. The difference isn’t just theoretical. In real life, kids using spacers have fewer ER visits, fewer hospital stays, and better control over their symptoms. One parent in Liverpool told me their 4-year-old went from two emergency trips a month to none after they started using the spacer right. That’s not luck. That’s science.
Spacers work by slowing down the medicine spray so it doesn’t just hit the back of the throat. Instead, it floats in the chamber, letting the child inhale it slowly into the lungs where it’s needed. This also means less medicine sticks to the mouth or throat, which cuts down on side effects like hoarseness or thrush. For kids on daily steroid inhalers, that’s a big deal.
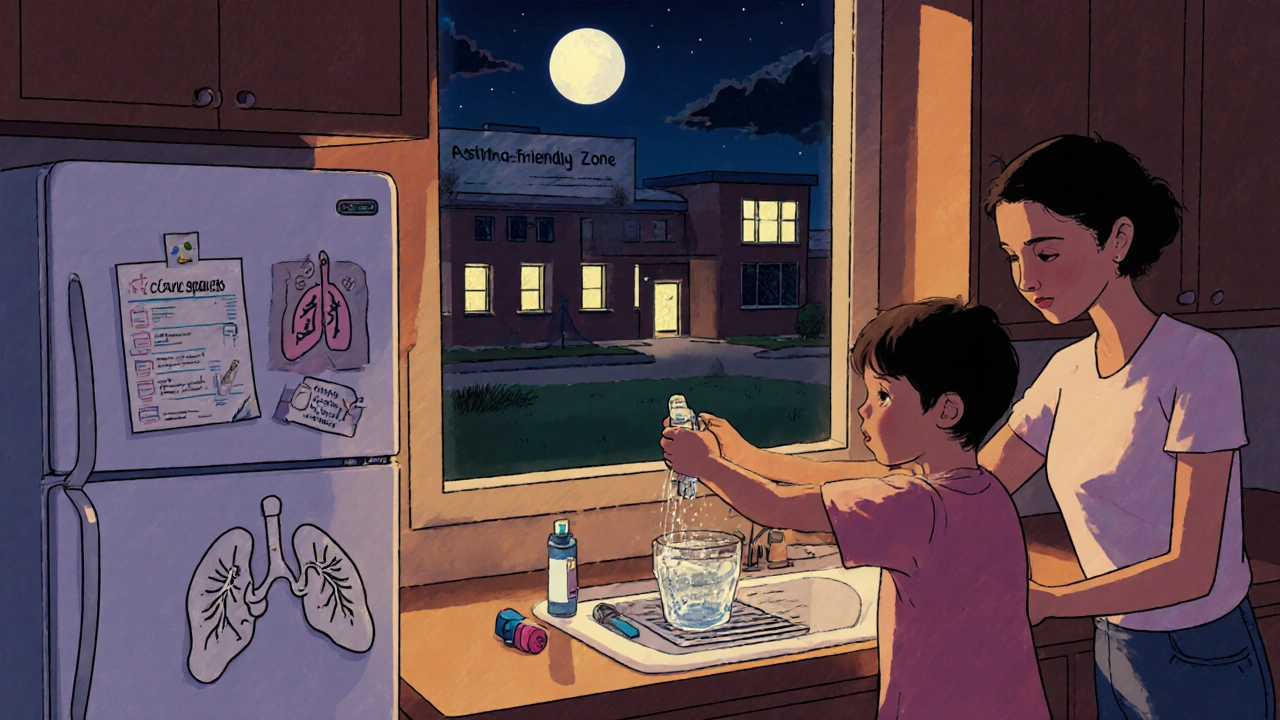
How to Use a Spacer the Right Way
Using a spacer isn’t hard-but getting it right matters. Here’s the step-by-step that works for most kids:
- Have your child sit upright. No slouching.
- Attach the inhaler to the spacer. Make sure it’s snug.
- Put the mouthpiece in their mouth, or fit the mask over nose and mouth if they’re under five.
- Press the inhaler button once-only once. Don’t pump it multiple times.
- Have them breathe in and out slowly through their mouth for four breaths. Count it out: one... two... three... four.
- Wait 30 seconds before giving a second puff, if prescribed.
Here’s what most people get wrong: they wipe the spacer dry after washing it. Don’t. Static electricity builds up and traps the medicine. Instead, wash it with a drop of dish soap and water, then let it air-dry without rinsing. The tiny soap film reduces static and helps the medicine move through. Do this once a week. If the spacer gets wet during use-say, from saliva or moisture-don’t use it. Wet spacers don’t work. Keep a spare one handy, especially for school.
For toddlers, use a mask. For older kids, switch to a mouthpiece. But don’t rush the transition. If your 8-year-old still prefers the mask and it works, stick with it. The goal isn’t to grow out of the mask-it’s to get the medicine into the lungs.
Why Schools Are Critical for Asthma Control
Asthma is the leading cause of school absenteeism in the UK and US. One in 11 children has asthma. That means in a typical classroom of 30 kids, at least two are managing it every day. But schools aren’t always prepared. Many don’t have spacers on hand. Some don’t know how to use them. Others assume parents will handle everything.
That’s a dangerous assumption. Asthma attacks don’t wait for school hours to end. They happen during PE, lunchtime, or recess. A child with a severe attack can’t walk to the nurse’s office if they’re gasping for air. Having a spacer and inhaler immediately available can mean the difference between a quick fix and a 999 call.
As of 2023, 42 U.S. states require schools to keep asthma medication on-site. The UK doesn’t have a national mandate, but NHS guidelines strongly recommend it. Schools with asthma-friendly policies-meaning trained staff, accessible spacers, and clear care plans-see 37% fewer asthma-related absences. That’s not just about attendance. It’s about letting kids be kids. Running, laughing, playing without fear.
But here’s the gap: rural schools have 45% less access to spacers than urban ones. Even in cities, many schools keep spacers locked away in the nurse’s office. That’s not good enough. Spacers should be stored at room temperature, out of direct sunlight, and ready to grab. Teachers, coaches, and lunch monitors should know where they are and how to use them.

What a Good Asthma Care Plan Includes
A written asthma action plan isn’t just paperwork. It’s a lifeline. It tells everyone-parents, teachers, school nurses, even babysitters-exactly what to do when symptoms flare up. The best ones are simple, visual, and color-coded: green (doing well), yellow (caution), red (emergency).
Every care plan should include:
- The child’s name, date of birth, and emergency contacts
- Names and dosages of all asthma medications
- Instructions for daily controller meds and rescue inhalers
- How to use the spacer with each inhaler
- Early warning signs (coughing, wheezing, fatigue, reduced play)
- When to use the rescue inhaler
- When to call 999 or go to A&E
- Signature of the child’s doctor and parent/guardian
Many schools now require this plan before allowing a child to carry their own inhaler. That’s smart. But it’s not enough to just collect the form. The plan needs to be reviewed every 6 months, updated after any hospital visit, and shared with new teachers each term. A plan that sits in a drawer is useless.
One school in Manchester started posting digital copies of care plans on a secure staff portal. Teachers could access them on their phones during PE or trips. Within a year, asthma-related incidents dropped by 52%. The key? Accessibility. Knowledge. Action.
The Teenage Problem: Why Older Kids Stop Using Spacers
Here’s the hard truth: as kids get older, they stop using spacers-even when they know they should. One study found that teens (14-18) are 80% less likely to use their inhaler correctly than kids aged 4-8. Why? Peer pressure. Embarrassment. Convenience.
Spacers are bulky. They’re not cool. A 15-year-old doesn’t want to pull out a plastic tube in front of friends before PE. So they skip it. Or worse-they use the inhaler alone, which doesn’t work well. That’s why asthma control often gets worse in adolescence.
The fix isn’t to shame them. It’s to adapt. There are now compact, sleek spacers designed for teens. Some fit in a pocket. Others come in fun colors. Some even have a small carrying case with a clip. A school nurse in Birmingham started letting teens keep a mini-spacer in their PE bag. No one had to see it. No one had to ask. The result? Usage jumped from 22% to 71% in six months.
Also, talk to them. Not like a parent. Like a friend. Ask: “What’s the hardest part about using your inhaler?” Listen. They might say, “I hate that it makes me sound weird.” Or, “I forget it’s in my bag.” Then solve it with them. Maybe they need a reminder app. Maybe they need a new spacer that looks like a phone charger. The goal isn’t to make them use a spacer because the doctor said so. It’s to make them feel in control.
What’s Changing in Asthma Care (2025)
The tools are getting smarter. In 2024, the CDC launched a national program to distribute free spacers to schools in underserved areas. The NHS is rolling out training modules for school staff, with certificates for those who complete them. And there’s new tech on the horizon.
Researchers at the University of Manchester are testing a smartphone app that connects to a smart spacer. The spacer has a tiny sensor that detects when it’s used. The app sends a quiet alert to the child’s phone if they haven’t used it in 48 hours. It also gives feedback: “You breathed too fast-try slower next time.” Parents and nurses get weekly summaries. It’s not about surveillance. It’s about support.
NIH is funding a £2.5 million trial of this tech in 50 UK schools through 2025. Early results show kids who used the app improved their technique by 65%. The best part? Teens loved it. It felt like a game, not a chore.
Meanwhile, manufacturers are designing spacers with better anti-static materials and easier-to-clean parts. The old plastic ones that trap medicine? They’re being phased out. New ones last longer, work better, and cost about the same.
What You Can Do Right Now
If your child has asthma, here’s what to do this week:
- Check their spacer. Is it cracked? Wet? Dirty? Replace it if needed.
- Wash it with dish soap and let it air-dry-no rinsing.
- Ask your GP or asthma nurse for a written care plan if you don’t have one.
- Give a copy to the school. Ask if they have a spare spacer on hand.
- Practice the 4-breath technique with your child. Make it a routine, like brushing teeth.
- If your teen refuses the spacer, ask if they’d try a smaller, sleeker version.
Don’t wait for an attack to happen. Asthma is manageable. But only if the tools are used right-and everyone knows how.
Can my child use an inhaler without a spacer?
Yes, but it’s not ideal-especially for children under 12. Without a spacer, most of the medicine hits the back of the throat and gets swallowed instead of reaching the lungs. This reduces effectiveness and increases side effects like hoarseness or thrush. For young kids, it’s nearly impossible to coordinate pressing the inhaler and breathing in at the same time. Spacers are recommended for all children using metered-dose inhalers, according to the Global Initiative for Asthma (GINA) and the American Academy of Pediatrics.
How often should I clean my child’s spacer?
Wash the spacer once a week with a drop of dish soap and warm water. Don’t rinse it after washing-just let it air-dry. Rinsing removes the tiny soap film that prevents static, which can trap medicine inside. Never wipe it dry with a towel. Static buildup means less medicine gets to the lungs. If the spacer gets wet during use, don’t use it until it’s dry. Keep a spare on hand for emergencies.
Does my child’s school have to have asthma spacers available?
In the UK, there’s no national law requiring schools to stock spacers, but NHS guidelines strongly recommend it. Many schools do keep spacers and inhalers on-site for emergencies. In the US, 42 states require schools to have asthma medication available. Even if your school doesn’t have one, you can provide a spare spacer and ensure staff know how to use it. A written asthma action plan helps make this clear.
Why does my teenager refuse to use a spacer at school?
Teens often feel embarrassed using spacers around friends. They think it makes them look different or weak. Spacers are bulky, and many older models look outdated. Solutions include switching to a compact, modern spacer that fits in a pocket, letting them keep it in their PE bag, or using a discreet case. Talk to them about their concerns-not to push them, but to help them find a solution that works for their life. Some teens respond better to tech-based reminders, like apps that track usage.
What’s the difference between a spacer and a nebulizer?
Both deliver asthma medication, but they work differently. A nebulizer turns liquid medicine into a mist you breathe in through a mask or mouthpiece. It takes 10-15 minutes and needs electricity. A spacer works with a handheld inhaler and delivers the same medicine in seconds. Studies show spacers are just as effective as nebulizers for mild to moderate asthma attacks-and they’re cheaper, quieter, and easier to carry. For kids under five, spacers are now the first-line recommendation over nebulizers.
Can my child carry their own inhaler and spacer to school?
Yes, if they’re old enough to use them correctly and the school allows it. Most schools require a written asthma action plan signed by a doctor and parent before permitting self-carry. Even if your child carries their own, the school should still have a spare on hand for emergencies. Some teens prefer carrying a mini-spacer in their pocket or bag. Make sure they know how to store it properly and clean it regularly.


Mark Kahn
November 21, 2025 AT 02:11Love this breakdown! My 6-year-old used to cough through every PE class until we got a spacer. Now she runs like a cheetah. Seriously, if your kid’s on an inhaler and you’re not using a spacer, you’re basically giving them a fancy aerosol spray. Do the thing.
Anne Nylander
November 22, 2025 AT 02:15OMG YES!! I just learned about the no-rinse thing and my kid’s spacer hasn’t been sticky since!! 🙌 Also, my school didn’t have one so I left a spare with the nurse-she cried. Not kidding. Teachers need this info.
Leo Tamisch
November 23, 2025 AT 22:55Interesting. But let’s be real-this is just another corporate wellness push disguised as medical advice. The real issue? Air pollution, processed food, and overmedication. Spacers? Cute. But what about the root causes? 🤔
Pravin Manani
November 25, 2025 AT 07:35From an immunology perspective, the spacer’s aerosol dispersion kinetics significantly enhance bronchial deposition efficiency by reducing oropharyngeal impaction. The static-electrostatic interface mitigation via non-rinsed surfactant residue is a brilliant low-cost innovation-aligns with GINA’s 2023 guidelines on pediatric MDI delivery optimization.
Noah Fitzsimmons
November 27, 2025 AT 05:55Wait, so you’re telling me a $5 plastic tube is more effective than a $200 nebulizer? And schools don’t have them? Someone’s making bank on nebulizers. Who’s the distributor? I need to know.
Chris Vere
November 28, 2025 AT 07:15The science here is sound but the human element is often overlooked. Children are not problems to be fixed with devices. They are beings learning to navigate a world that often treats their bodies as malfunctioning machines. The spacer is a tool, yes-but compassion, patience, and presence are the real medicine. Let us not confuse efficiency with care.
Daisy L
November 30, 2025 AT 06:06AMERICA IS LEADING THE WAY WITH 42 STATES MAKING THIS MANDATORY-AND THE UK? STILL TINKERING WITH ‘RECOMMENDATIONS’?!?!? This isn’t a ‘nice-to-have’-it’s a LIFE-SAVING STANDARD. Why are we letting bureaucracy kill kids?!?!
Franck Emma
December 1, 2025 AT 00:05My kid’s asthma got worse after school started. No spacer. No plan. No help. Now he’s on steroids. I’m done being polite.
Kartik Singhal
December 2, 2025 AT 19:54Smart spacer tech? 🤨 Sounds like Big Pharma’s next surveillance play. Next thing you know, the app will report you to the school if your kid misses a puff. They’re already tracking our kids’ heart rates via smartwatches. This isn’t progress-it’s control.
Cooper Long
December 4, 2025 AT 18:25In many African communities, we use traditional breathwork and herbal steam to manage respiratory conditions. The spacer is a useful tool, but we must not forget the wisdom of ancestral practices. Balance is key.
Sheldon Bazinga
December 6, 2025 AT 00:37Spacers? Yeah, right. I bet the real reason kids are having more attacks is because schools won’t let them vape. That’s the real epidemic. Also, why do they always use ‘LIVERPOOL’ as an example? Like we don’t know how the UK works. 😒
Sandi Moon
December 7, 2025 AT 04:31Let me guess-the ‘smart spacer’ will be mandatory in 2026, funded by the WHO, and enforced by AI-powered school nurses. Next, they’ll implant microchips in children’s lungs to monitor ‘breath compliance.’ This isn’t medicine. It’s the beginning of the New World Order.