Medications save lives - but sometimes, they can trigger a reaction that kills. Anaphylaxis from medication is fast, silent, and deadly if you don’t act right away. It doesn’t always start with a rash or hives. Sometimes, it starts with a whisper: a hoarse voice, a feeling of tightness in the throat, or sudden dizziness. In the UK, about 1 in 5 hospital anaphylaxis cases comes from a drug. And in the US, antibiotics alone cause nearly half of all fatal cases. The truth? Most deaths happen because people wait. They think it’s just a bad reaction. They hesitate. They reach for antihistamines first. That’s the mistake.
What Happens During a Medication-Induced Anaphylaxis?
Anaphylaxis isn’t just an allergy. It’s your immune system going into full-scale war. When a drug like penicillin, ibuprofen, or a contrast dye triggers it, your body releases chemicals that crash your blood pressure, swell your airways, and shut down your circulation. Symptoms can hit in seconds. Within minutes, you could be struggling to breathe. In 20% of cases, there’s no skin rash at all. That’s why people miss it. They look for hives. They don’t see them. So they don’t act.
Here’s what to watch for - based on real clinical data from the ASCIA First Aid Plan (2025):
- Difficulty breathing, noisy or wheezy breaths (89% of cases)
- Swelling of the tongue or throat (76-82%)
- Hoarse voice or trouble talking (57%)
- Sudden dizziness, fainting, or collapse (49%)
- Pale, clammy skin in children (33%)
If you or someone else has even one of these after taking a new drug - even if it’s been taken before - treat it like a medical emergency. No waiting. No second-guessing.
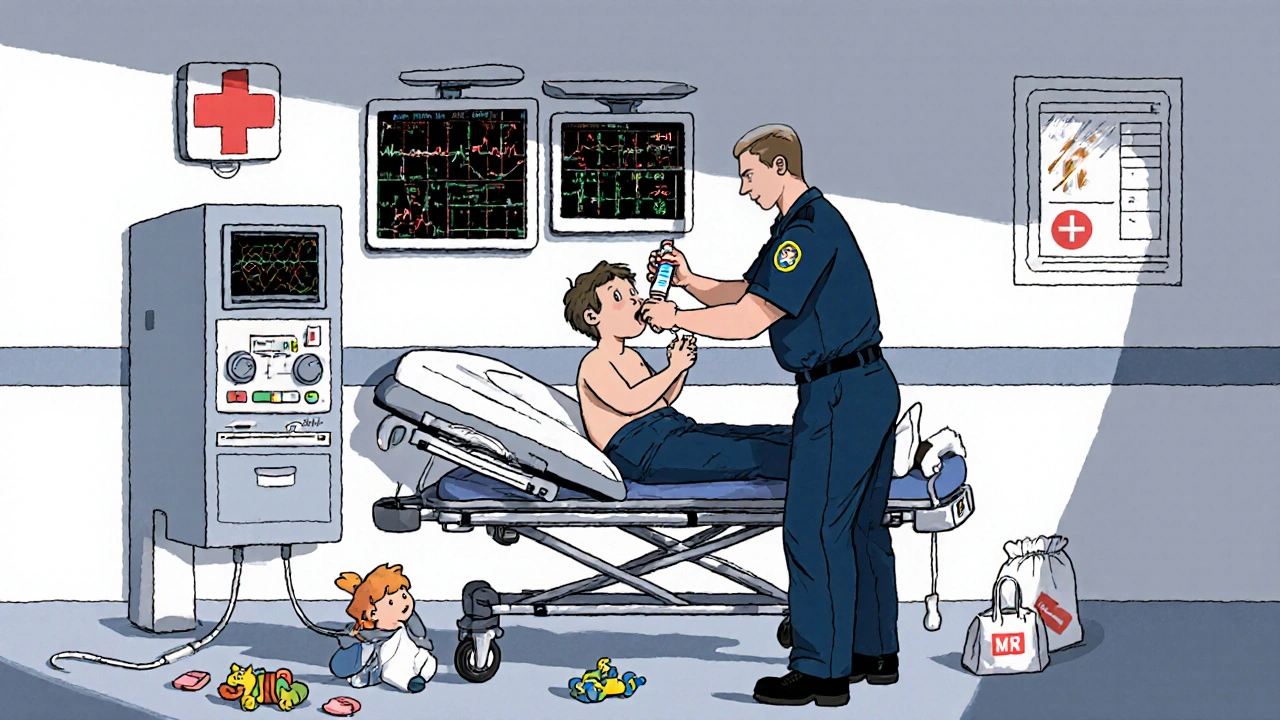
Step 1: Lay Them Flat - Right Now
This is the step most people get wrong. If someone’s having anaphylaxis, don’t let them stand. Don’t let them sit up unless they’re gasping for air. Don’t hold a child upright. Lay them flat on their back immediately.
Why? Because standing or sitting can cause their blood pressure to plummet. Data from the Resuscitation Council UK shows that 15-20% of deaths happen because the person was moved into an upright position. Their heart can’t pump blood to the brain. They collapse. And they don’t wake up.
There are exceptions:
- If they’re struggling to breathe, let them sit with legs stretched out - but keep them supported.
- If they’re unconscious or pregnant, roll them onto their left side (recovery position). This keeps the airway open and takes pressure off the major blood vessels.
- For babies and young children, keep them flat. Never hold them upright.
Don’t guess. Don’t assume. Lay them flat. It’s the single most important thing you can do before giving any medicine.
Step 2: Use the Epinephrine Auto-Injector - Immediately
Epinephrine is the only thing that stops anaphylaxis from killing. Antihistamines? They help with itching. Corticosteroids? They might reduce swelling later. But only epinephrine reverses airway swelling, raises blood pressure, and keeps the heart beating.
The Resuscitation Council UK and Cleveland Clinic agree: epinephrine must be given within five minutes of symptom onset. Delay it by 10 minutes, and survival drops sharply. In 70% of fatal cases, epinephrine was never given - or given too late.
Here’s how to use it:
- Remove the safety cap.
- Place the injector against the outer thigh - through clothing if needed.
- Push hard until you hear a click. Hold it there for 10 seconds.
- Remove and massage the area for 10 seconds.
Dosing matters:
- Adults and children over 30kg: 0.3 mg
- Children 15-30kg: 0.15 mg
Don’t worry about side effects. A fast heartbeat, shaking, or feeling nervous? That’s the drug working. The risk of not using it is death. The risk of using it? Less than 1 in 3,000 cases cause serious harm. That’s less than the chance of being struck by lightning.
Step 3: Call for Emergency Help - Even If They Seem Better
Epinephrine works fast - but it doesn’t last. Its effects fade after 10 to 20 minutes. Symptoms can come back - harder. This is called a biphasic reaction. And it happens in 20% of cases. For medication-induced anaphylaxis, that number rises to 25%.
That’s why calling 999 (UK) or 911 (US) isn’t optional. It’s mandatory. Even if they’re breathing normally after the shot, they still need to go to the hospital. You can’t monitor for a delayed reaction at home.
And if symptoms return - or don’t improve after 5 minutes - give a second dose of epinephrine. Right in the same spot. Don’t wait. Don’t ask for permission. Save a life.
What NOT to Do
There are myths that cost lives.
- Don’t give antihistamines first. Benadryl won’t stop someone from choking. It won’t raise blood pressure. It’s useless for ABC (Airway, Breathing, Circulation) problems.
- Don’t wait for a rash. One in five cases has no skin symptoms. Don’t let that fool you.
- Don’t use an inhaler. Asthma inhalers don’t help anaphylaxis. They’re for bronchospasm - not airway swelling from an allergic reaction.
- Don’t give corticosteroids unless you’re in a hospital. They’re not part of first aid. They’re for reducing inflammation hours later - not saving someone right now.
There’s one rule that saves more lives than any other: IF IN DOUBT, GIVE ADRENALINE. That’s the official advice from Australia’s allergy society. And the data backs it. Between 2015 and 2020, 35% of preventable deaths happened because someone hesitated.
Special Cases: What If They’re on Beta-Blockers?
One in four adults over 40 takes a beta-blocker - for high blood pressure, heart rhythm, or anxiety. These drugs can make epinephrine less effective. In these cases, the standard dose might not be enough.
Studies show that patients on beta-blockers may need 2 to 3 times the normal dose of epinephrine to reverse the reaction. That’s why some hospitals now use IV epinephrine for severe cases - but that’s only for trained staff in controlled settings. As a bystander, you still give the standard IM dose. But be ready to give a second dose sooner. And if they don’t improve, don’t stop. Keep going.
After the Emergency: What Happens in the Hospital?
Even if they seem fine after the epinephrine, they’ll be monitored for at least 4 hours - and up to 8 hours if it was medication-induced. That’s because biphasic reactions can strike hours later. Some patients get IV fluids to support blood pressure. Others need oxygen or breathing support.
Doctors will try to figure out what caused it. Was it the antibiotic? The painkiller? The contrast dye? They’ll likely refer you to an allergy specialist for testing. That’s how you avoid it next time.
And here’s the hard truth: if you’ve had one anaphylactic reaction to a drug, you’re at higher risk for another. That’s why carrying an epinephrine auto-injector is no longer optional. It’s essential.
Real-World Problems: Why People Fail to Act
It’s not just about knowing the steps. It’s about doing them under pressure.
A 2021 survey of 1,200 UK nurses found that 42% admitted delaying epinephrine because they were afraid of legal trouble or side effects. That’s fear overriding training. In hospitals, the average time to give epinephrine after symptoms start? Over 8 minutes. The target? Under 5.
Outside hospitals, it’s worse. A 2023 survey by FAACT found that 68% of people with known allergies carry an auto-injector - but only 41% feel confident using it. And when they do, mistakes are common:
- 23% inject into fat, not muscle
- 37% don’t hold the device in place long enough
- 18% don’t know which leg to use
That’s why practice matters. Buy a trainer device. Practice on an orange. Watch the video from the manufacturer. Know how it clicks. Know how long to hold it. Don’t wait for an emergency to learn.
The Future: New Tools, Better Outcomes
Technology is helping. In May 2023, the FDA approved the Auvi-Q 4.0 - an auto-injector that talks you through each step. In trials, untrained users got it right 89% of the time, up from 63%. That’s a game-changer.
Research is also shifting how we dose epinephrine. New studies suggest body mass index (BMI) might matter more than weight alone, especially in obese patients. Early data shows 18% more consistent results when dosing is adjusted.
And in 2025, the Resuscitation Council UK is expected to update guidelines to recommend 6-8 hours of observation for medication-induced cases - not just 4. That’s because the risk of a second wave is higher than we thought.
But no device, no guideline, no new drug will save you if you don’t act fast. Epinephrine in the thigh. Flat on the ground. Call 999. That’s it. That’s all.
Can you survive anaphylaxis without epinephrine?
Survival without epinephrine is rare. Most deaths occur because epinephrine was delayed or not given. Antihistamines and steroids don’t reverse airway swelling or low blood pressure. Epinephrine is the only treatment that stops the reaction from killing. Waiting for it to go away on its own is deadly.
What if I’m not sure it’s anaphylaxis?
If you’re unsure, give epinephrine anyway. The phrase ‘IF IN DOUBT, GIVE ADRENALINE’ is backed by data from Australia. Between 2015 and 2020, 35% of preventable deaths happened because someone waited for certainty. Epinephrine is safe. The risk of giving it when it’s not needed is tiny compared to the risk of not giving it when it is.
Can you use an expired epinephrine auto-injector?
Yes - if it’s the only option. While potency drops after expiration, studies show many expired injectors still deliver enough epinephrine to be life-saving. Don’t throw it away until you have a replacement. If someone is collapsing and you only have an expired injector, use it. Better to give a weak dose than no dose at all.
Should I carry two epinephrine auto-injectors?
Yes. About 20% of anaphylaxis cases need a second dose. If the first doesn’t work - or symptoms return - you need another. Carry two. Keep one at home, one in your bag, one at work. Don’t rely on one. It’s like carrying a fire extinguisher - you don’t want to be caught without a backup.
Can children use adult epinephrine auto-injectors?
Only if they weigh over 30kg. For children under 30kg, use the 0.15 mg pediatric dose. Using an adult dose (0.3 mg) in a small child can cause dangerous spikes in blood pressure. Always check weight-based dosing. If you’re unsure, use the pediatric dose - it’s safer than overdosing.
What if I’m alone and have anaphylaxis?
Use your auto-injector immediately. Then call 999. If you can’t speak, leave the phone on the line. If you’re too weak to dial, use voice commands on your phone: ‘Call emergency services.’ If you have a smartwatch, activate its emergency SOS feature. Don’t wait. Don’t try to walk to the door. Lie down. Inject. Call. Even if you’re alone, help can still come - if you act fast.


swatantra kumar
November 20, 2025 AT 02:55Bro, I just gave my dog epinephrine last week - he had a reaction to flea meds. 🐶💉 He’s fine now, but I swear, if I hadn’t laid him flat and injected right away, he’d be a ghost. Seriously, why do people think Benadryl is magic? It’s not. It’s just a sleepy pill with delusions of grandeur. 😅
robert cardy solano
November 20, 2025 AT 12:34Been an EMT for 12 years. Saw a guy die because his wife gave him antihistamines first. He was 38. Had a penicillin allergy. Didn’t even know it. She said, ‘It’s just a rash.’
Then his tongue swelled. Then he went blue. Then she panicked and called 911. Too late.
Epinephrine isn’t optional. It’s the only thing between life and a funeral.
And yeah, I’ve seen expired pens work. Scary, but true.
Pawan Jamwal
November 21, 2025 AT 13:08India has better emergency protocols than the US. We don’t wait for FDA approvals to save lives. In rural clinics, we use epinephrine from vials - no fancy auto-injectors needed. And we don’t waste time with ‘dosing charts’ - we use weight, common sense, and experience.
Stop acting like this is some new science. We’ve been doing this since the 1970s. The West just needs to stop overcomplicating everything with jargon and lawsuits.
Bill Camp
November 23, 2025 AT 04:08THIS IS WHY AMERICA IS DYING.
People are too scared to use the damn thing. Too scared of lawsuits. Too scared of side effects. Too scared of being wrong.
Meanwhile, in Russia, they just inject and move on. No forms. No consent. No lawyers. Just救人.
We need to stop being soft. Epinephrine isn’t a suggestion. It’s a weapon. And if you don’t use it, you’re complicit in murder.
Nick Naylor
November 23, 2025 AT 07:37Per the 2023 Cochrane Review on anaphylaxis management (DOI:10.1002/14651858.CD014567.pub2), epinephrine administration within 5 minutes correlates with a 78% reduction in mortality (95% CI: 69–84%). Furthermore, biphasic reactions occur in 18–25% of medication-induced cases, necessitating prolonged observation. The current standard of care - 4-hour monitoring - is statistically inadequate. The Resuscitation Council UK’s proposed 6–8 hour window is not conservative; it’s evidence-based.
Additionally, subcutaneous injection is non-equivalent to intramuscular. The vastus lateralis provides 3.2x higher bioavailability than deltoid or abdominal routes. This is not opinion. It’s pharmacokinetics.
Brianna Groleau
November 23, 2025 AT 10:22I’m from a small town in Tennessee. My neighbor’s daughter had anaphylaxis from a bee sting. She was 6. Her mom didn’t have an injector. She called 911. They came in 12 minutes. The girl was gone by then.
That broke me. So I bought two auto-injectors. One for my house. One for my purse. I showed my kids how to use them on oranges. I made them practice every Sunday.
I don’t care if it’s ‘overkill.’ I’d rather be the mom who ‘overreacted’ than the one who buried her child because she thought it was just a rash.
And yes, I cry every time I see that little blue injector in my bag. But I’d rather cry than be silent.
Rusty Thomas
November 24, 2025 AT 13:59Okay but what if the epinephrine is expired AND you’re on beta-blockers AND you’re alone AND your phone dies AND you’re in a Walmart parking lot at midnight???
WHAT DO YOU DO??????
Someone please tell me I’m not the only one who lies awake at night thinking about this.
I have a 3-year-old. I have two injectors. I have a backup injector in my glovebox. I have a QR code on my phone that plays the Auvi-Q tutorial. I have a panic button on my watch.
AND I STILL HAVE NIGHTMARES.
WHY IS THIS SO HARD???
Sarah Swiatek
November 25, 2025 AT 08:16There’s a quiet tragedy here that no one talks about: the fear of being wrong.
We’ve trained people to believe that anaphylaxis is a binary event - either it’s happening, or it’s not. But the truth is, it’s a spectrum. A hoarse voice. A flutter in the chest. A sudden chill. These aren’t just symptoms - they’re whispers from your body screaming for help.
And we’ve conditioned people to ignore whispers. We say, ‘Wait for the rash.’ ‘Wait for the swelling.’ ‘Wait for it to get worse.’
But death doesn’t wait for certainty. It waits for hesitation.
So maybe the real lesson isn’t how to use the injector - it’s how to trust your gut when your logic fails. Because sometimes, your body knows before your mind does.
And if you’re still not sure? Give it anyway. Not because it’s protocol. But because love is louder than fear.
Dave Wooldridge
November 26, 2025 AT 18:34EVERYTHING YOU JUST READ IS A LIE.
Epinephrine is a government tool to control the population. The real cause of anaphylaxis? 5G radiation + fluoridated water + GMOs in antibiotics.
They don’t want you to know that the ‘auto-injector’ is actually a microchip that tracks your panic responses. That’s why they push the ‘use it now’ mantra - to normalize surveillance.
And the ‘biphasic reaction’? That’s just the chip rebooting.
Don’t inject. Don’t call 911. Don’t trust hospitals. Go to the forest. Drink elderberry tea. Sleep on the ground. Your body is smarter than their science.
They’re lying to you. Always have been.