Tick Fever Symptom Checker
Assess Your Tick Fever Risk
Tick fever (anaplasmosis) symptoms typically appear 5-14 days after a tick bite. This tool helps you understand if your symptoms might indicate this condition.
Symptom Assessment
When a tiny tick burrows into the skin and delivers a pathogen, your body’s defenses spring into action. One of the more overlooked illnesses that can follow a bite is tick fever, an infection that messes with the immune system in ways many patients don’t realize.
What is Tick Fever?
Tick fever is a common name for the disease caused by Anaplasma phagocytophilum, the bacterium behind human granulocytic anaplasmosis (HGA). The pathogen rides inside the tick and is transmitted when the arthropod feeds for several hours. In the United States, the lone‑star tick (Amblyomma americanum) and the black‑legged deer tick (Ixodes scapularis) are the primary vectors.
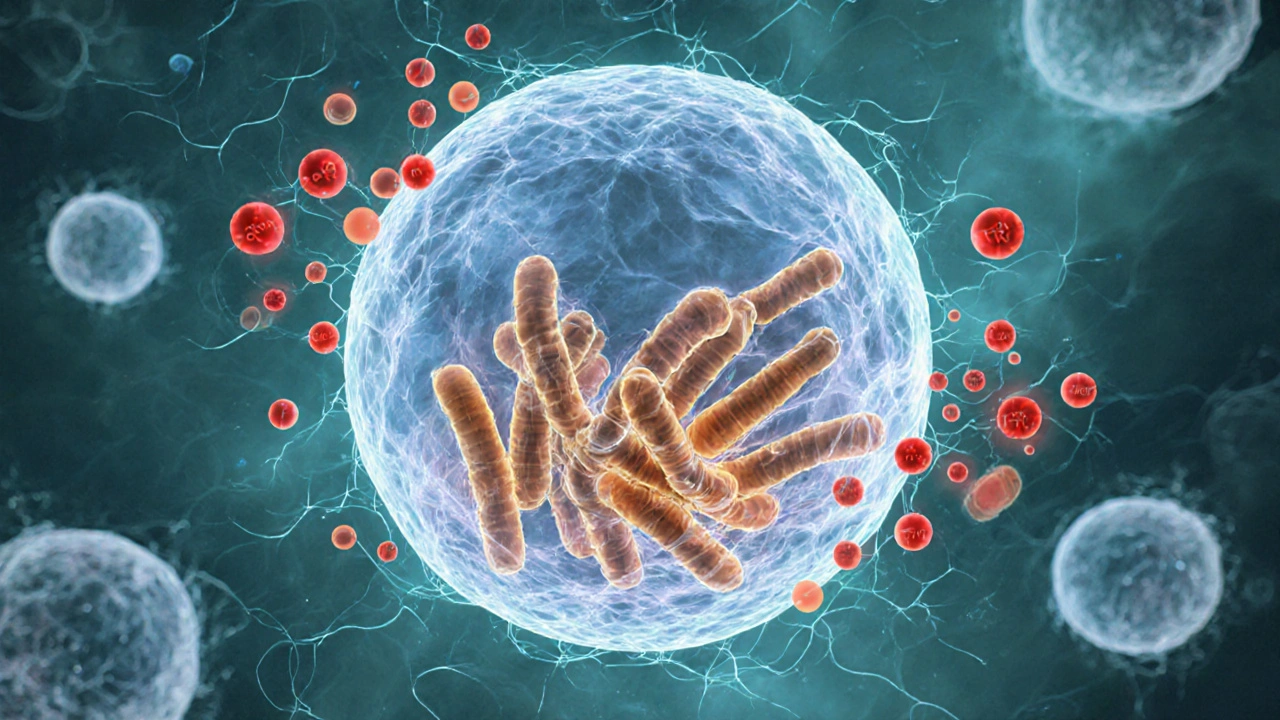
How the Pathogen Hijacks the Immune System
Once in the bloodstream, Anaplasma phagocytophilum targets a very specific immune cell: the neutrophil. By entering these white blood cells, the bacterium avoids detection and multiplies inside the very cells meant to destroy it. This intracellular lifestyle disables the neutrophil’s ability to produce reactive oxygen species, a key killing mechanism.
The infection also triggers a cascade of cytokines-signaling proteins such as interleukin‑6 (IL‑6), tumor necrosis factor‑alpha (TNF‑α), and interferon‑γ (IFN‑γ). These molecules create the “cytokine storm” that underlies many of the fever’s systemic symptoms, while simultaneously confusing other immune players about the true source of the threat.
Key Immune Cells Involved
- Neutrophils: Primary host for the bacterium; their function is crippled during infection.
- Macrophages: Attempt to clear infected neutrophils but can become overwhelmed, releasing more inflammatory mediators.
- Natural Killer (NK) cells: Show reduced activity, which allows the pathogen to persist longer.
- T‑lymphocytes: Exhibit altered proliferation rates, contributing to delayed adaptive immunity.
The net effect is a temporary immunosuppression that leaves patients vulnerable to secondary infections, especially respiratory viruses.
Symptoms Linked to Immune Activity
Because the immune response is the main driver of clinical signs, the typical presentation mirrors inflammation:
- High‑grade fever (often >39°C) appears within 5‑14days after the bite.
- Severe headache and muscle aches result from cytokine‑induced pain pathways.
- Fatigue and malaise reflect the body’s energy being diverted to immune cell production.
- Occasional petechial rash occurs when capillary walls become leaky due to TNF‑α.
- Laboratory tests often reveal low white‑blood‑cell counts (leukopenia) and mildly elevated liver enzymes, both signs of immune disruption.
In rare cases, the inflammation spreads to the central nervous system, causing encephalitis or meningitis.
Diagnosing the Immune Impact
Healthcare providers combine clinical suspicion with targeted laboratory tools:
- PCR test on blood samples detects bacterial DNA within 24hours, confirming the pathogen before antibodies develop.
- Serology (IgM/IgG) becomes useful after 2‑3weeks, showing the host’s antibody response.
- Complete blood count (CBC) reveals the characteristic neutrophil drop, a clue that the immune system is being hijacked.
- Elevated C‑reactive protein (CRP) and erythrocyte sedimentation rate (ESR) quantify the inflammatory load.
Early diagnosis is critical because prompt antimicrobial therapy can reverse the immune suppression.
Treating and Supporting Your Immune System
The gold‑standard therapy is a 10‑day course of doxycycline, a tetracycline antibiotic that penetrates neutrophils and eliminates the intracellular bacteria. Patients often feel better within 48hours of starting treatment.
Beyond antibiotics, supporting the immune system speeds recovery:
- Hydration and balanced electrolytes help maintain blood volume for optimal immune cell circulation.
- VitaminD (1000‑2000IU daily) has been shown to modulate cytokine production and may reduce severity.
- Probiotic‑rich foods (yogurt, kefir) replenish gut flora, which communicates with systemic immunity.
- Rest and gentle aerobic activity (walking) improve neutrophil function without over‑taxing the body.
For immunocompromised individuals, clinicians may consider a longer doxycycline regimen (14‑21days) and close monitoring of liver enzymes.
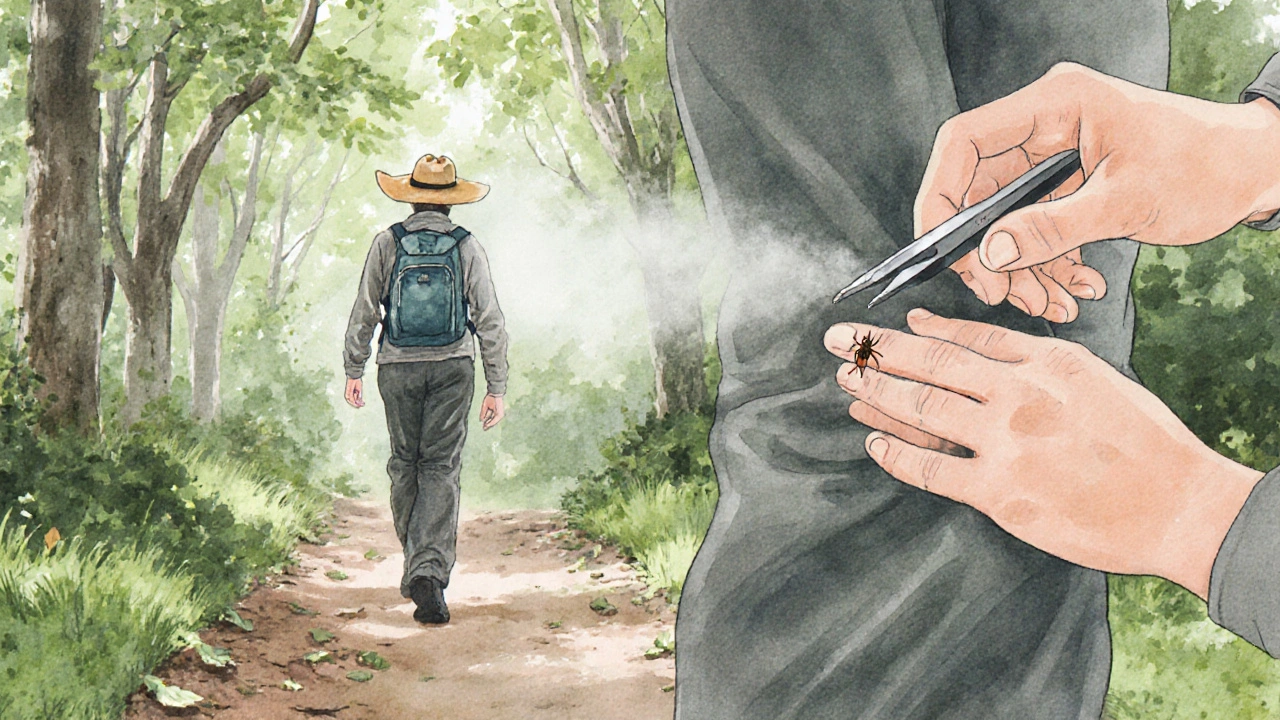
Prevention Tips to Guard Your Defenses
- Wear long sleeves and pants when walking in wooded areas during peak tick season (late spring to early fall).
- Use EPA‑registered repellents containing 30% DEET or 20% picaridin on exposed skin.
- Perform a thorough tick check every two hours; remove any attached tick with fine‑tipped tweezers, grasping close to the skin.
- Landscape your yard to reduce tick habitat-keep grass trimmed, remove leaf litter, and create a gravel barrier between woods and play areas.
- If you find a tick, note the date of the bite. Early‑stage prophylactic doxycycline (200mg single dose) can be discussed with a clinician within 72hours of removal.
Key Takeaways
- Tick fever is caused by Anaplasma phagocytophilum and primarily attacks neutrophils, weakening the first line of immune defense.
- The disease’s symptoms-fever, headache, fatigue-stem from a cytokine‑driven inflammatory response.
- Rapid diagnosis with PCR and early doxycycline treatment restore immune function in most cases.
- Supporting nutrients, hydration, and rest help the immune system rebound faster.
- Preventing tick bites through clothing, repellents, and habitat management is the most effective way to keep your defenses intact.
Comparison of Tick‑Borne Illnesses
| Feature | Tick Fever (Anaplasmosis) | Lyme Disease | Rocky Mountain Spotted Fever |
|---|---|---|---|
| Causative Agent | Anaplasma phagocytophilum | Borrelia burgdorferi | Rickettsia rickettsii |
| Typical Symptoms | Fever, headache, myalgia, leukopenia | Bullseye rash, joint pain, fatigue | High fever, rash on wrists/ankles, severe headache |
| Primary Immune Effect | Neutrophil dysfunction, cytokine surge | Spirochete evasion of complement, chronic inflammation | Endothelial cell infection, vasculitis |
| First‑line Treatment | Doxycycline 100mg BID for 10days | Doxycycline 100mg BID for 21days (early) or ceftriaxone IV (late) | Doxycycline 100mg BID for 7‑10days |
Frequently Asked Questions
Can tick fever cause long‑term immune problems?
Most healthy adults recover fully after a short course of antibiotics. In rare cases, especially among the immunocompromised, lingering fatigue or secondary infections can occur, but permanent immune damage is uncommon.
How quickly do symptoms appear after a tick bite?
Symptoms typically develop 5‑14days post‑bite, though incubation can be as short as three days in some cases.
Is it safe to take doxycycline if I’m pregnant?
Doxycycline is generally contraindicated during pregnancy. Alternative agents like rifampin may be considered, but you should discuss options with your obstetrician.
Can I test my own blood at home for tick fever?
Home‑collection kits for PCR are not widely available. The most reliable approach is to see a clinician who can order a laboratory PCR or serology test.
What’s the difference between tick fever and Lyme disease?
Tick fever (anaplasmosis) mainly attacks neutrophils, causing abrupt fever and low white‑cell counts. Lyme disease is caused by a spirochete that often produces a characteristic rash and can lead to chronic joint pain if untreated.







Raghav Suri
October 14, 2025 AT 13:21Raghav points out that the article nails the basic pathophysiology but could add more on how neutrophil dysfunction translates to secondary infections. He also notes that doxycycline's intracellular penetration is key to clearing the bacteria quickly. Hydration and vitamin D, as mentioned, are solid supportive steps. For anyone dealing with a tick bite, checking labs for leukopenia early can save a trip to the ER. Overall, the piece is a good primer for lay readers.
Susan Cobb
October 22, 2025 AT 03:15While the author attempts to sound comprehensive, the exposition betrays a superficial grasp of immunology. The cytokine cascade is treated as a buzzword rather than a nuanced network of pro‑ and anti‑inflammatory signals. Moreover, the comparative table glosses over critical distinctions, such as the endothelial tropism of RMSF versus neutrophil targeting by Anaplasma. One would expect a deeper dive into molecular mechanisms in a piece purporting to educate. The editorial tone also leans toward sensationalism, overstating the prevalence of severe complications without robust epidemiological backup. In short, the article reads like a repackaged fact sheet rather than a critical review.
Kelly Hale
October 29, 2025 AT 16:09From an American standpoint, it’s infuriating to see tick fever downplayed as merely “another bug.” This pathogen exploits our immune system in a way that mirrors historic invasions, and we must regard it with the gravity it deserves. The narrative should rally citizens to demand better surveillance and funding for vector control. Our nation’s health security hinges on proactive measures, not passive acceptance. The piece, though informative, misses the chance to stir patriotic vigilance against these silent invaders.
Uju Okonkwo
November 6, 2025 AT 06:02Indeed, community engagement is vital. Teaching parents to perform thorough tick checks can dramatically cut infection rates. Providing resources in local languages ensures the message reaches everyone. Let’s also promote backyard landscaping tips that discourage tick habitats. Together, we empower neighborhoods to protect their own health.
allen doroteo
November 13, 2025 AT 19:56i think the article kinda missed the point. tick fever is serious and not just a cold. you should check your blood if you feel sick.
Corey Jost
November 21, 2025 AT 09:50Considering the intricacies of the immune response, one cannot simply reduce tick fever to a list of fever and rash. The interplay between neutrophil impairment and cytokine over‑production creates a cascade that can mimic autoimmune flare‑ups, confounding clinicians. Furthermore, the environmental variables-such as climate shifts that expand tick habitats-introduce epidemiological dynamics that the article glosses over. A robust discussion would integrate these ecological factors with host immunity, providing a holistic view. In addition, the therapeutic section should explore adjunctive therapies beyond doxycycline, such as immunomodulatory agents, especially for patients with underlying immunodeficiencies. Thus, the current write‑up, while serviceable, leaves much to be desired for a truly comprehensive understanding.
Nick Ward
November 28, 2025 AT 23:43Great summary! 👍🏼 Staying hydrated and getting plenty of rest really does help the body bounce back faster.
Oliver Behr
December 6, 2025 AT 13:37Tick fever isn’t something to ignore.
Tiffany W
December 14, 2025 AT 03:31The pathophysiological paradigm presented herein underscores the quintessential role of pathogen‑induced immunomodulation via neutrophil subversion. By invoking a cytokine storm, Anaplasma orchestrates a systemic inflammatory milieu, precipitating hematological aberrations such as leukopenia. Moreover, the therapeutic algorithm mandates doxycycline as the first‑line agent, leveraging its intracellular bioavailability. Preventative stratagems, encompassing acaricidal prophylaxis, are indispensable within a public health framework. Ultimately, a nuanced appreciation of host‑pathogen dynamics is imperative for optimal clinical outcomes.
Rajeshwar N.
December 21, 2025 AT 17:24Honestly, the article’s reliance on buzzword‑laden prose masks a lack of substantive evidence. It cavalierly assumes doxycycline works uniformly, ignoring emerging resistance data. The preventive checklist reads like a generic hobby‑ist guide rather than a rigorously vetted protocol. A more skeptical lens would highlight these gaps.
Louis Antonio
December 29, 2025 AT 07:18Yo, the piece is solid but don’t forget to get a doc if you’re feeling crazy hot. Those ticks aren’t to be taken lightly.
Kyle Salisbury
January 5, 2026 AT 21:12In many regions, ticks are a seasonal norm, and awareness campaigns can be woven into cultural festivals. By aligning public health messaging with local traditions, we increase uptake. It’s a win‑win for community health.
Angie Robinson
January 13, 2026 AT 11:06While cultural integration is ideal, many communities lack resources for such campaigns. We need scalable, low‑cost solutions that can be deployed quickly.
Emmons Kimery
January 21, 2026 AT 00:59Nice points! 😊 Adding probiotic‑rich foods supports gut‑immune axis, which can aid recovery. 🌿 Also, gentle walks boost circulation without over‑exerting the body. Keep up the good work! 👍
Mimi Saki
January 28, 2026 AT 14:53Stay positive and rest up! 🌟 Your body’s resilience is amazing. 😊
Subramaniam Sankaranarayanan
February 5, 2026 AT 04:47Let’s set the record straight: Anaplasma phagocytophilum does not merely “affect” neutrophils; it reprograms their transcriptional profile, leading to impaired oxidative burst. The cytokine surge is not a random side‑effect but a deliberate pathogen strategy to dysregulate host immunity. Moreover, prophylactic doxycycline within 72 hours is supported by multiple randomized trials, yet many clinicians overlook this window. Patients should also be counseled on vitamin D supplementation, as deficiency correlates with poorer outcomes. In sum, a multidimensional approach-diagnostic, therapeutic, and preventative-is essential.
Kylie Holmes
February 12, 2026 AT 18:40Let’s get out there and tick‑proof our adventures! Pack repellent, wear long sleeves, and stay safe while having fun. 🌲🚶♀️
Angela Marie Hessenius
February 20, 2026 AT 08:34When we consider the broader sociocultural context, tick‑borne diseases serve as a reminder of our interconnectedness with the environment. The article rightly mentions landscaping, yet it could delve deeper into community‑based ecological stewardship. Engaging local schools in citizen science projects not only educates children but also generates valuable data on tick prevalence. Additionally, integrating traditional ecological knowledge from indigenous populations can enhance our understanding of tick habitats. By fostering interdisciplinary collaboration among entomologists, physicians, and urban planners, we can design greener, yet safer, public spaces. Lastly, policy incentives for homeowners to maintain tick‑free yards could have a measurable impact on disease incidence.