Hormonal Birth Control and Blood Thinners: Risks, Interactions, and What You Need to Know
When you're on hormonal birth control, a medication that uses synthetic hormones like estrogen and progestin to prevent pregnancy. Also known as oral contraceptives, it works by stopping ovulation, thickening cervical mucus, and thinning the uterine lining. And you're also taking blood thinners, medications like warfarin, apixaban, or rivaroxaban that reduce your blood’s ability to clot. Also known as anticoagulants, they’re prescribed for conditions like atrial fibrillation, deep vein thrombosis, or after a pulmonary embolism. That’s not just a coincidence — it’s a common combo. But mixing them isn’t harmless. The estrogen in many birth control pills can raise your risk of blood clots. Add that to a blood thinner, and your body’s balancing act gets tricky. You might think, "I’m on a blood thinner, so I’m protected," but that’s not how it works. Blood thinners don’t cancel out the clotting risk from hormones — they just try to manage it. And sometimes, they don’t manage it well enough.
Here’s what actually happens: estrogen increases clotting factors like Factor VII and fibrinogen. Blood thinners try to lower those same factors. It’s like turning up the heat while running the AC. The result? Unpredictable clotting or bleeding. Studies show women on combined hormonal birth control have up to a 3- to 4-fold higher risk of venous thromboembolism compared to non-users. That risk jumps even higher if you’re over 35, smoke, are obese, or have a family history of clots. And if you’re already on warfarin, your INR levels can swing wildly — too low, and you risk clots; too high, and you risk bleeding. Some newer blood thinners like apixaban are less affected by hormonal changes, but they’re not magic. You still need monitoring. And if you’re on a progestin-only pill or IUD, your risk is much lower — but not zero. The key is knowing your personal risk profile, not just following a general rule.
It’s not just about pills. Hormonal IUDs, patches, rings, and implants all carry similar risks. So do some gender-affirming hormone therapies that use estrogen. And if you’re taking other meds — like antibiotics or seizure drugs — they can mess with how your body processes either the birth control or the blood thinner. One wrong interaction, and you could end up in the ER. That’s why doctors don’t just hand out prescriptions for both. They look at your full history: age, weight, smoking status, past clots, liver function, even your diet. If you’re on both, you need regular check-ups. Not every year — maybe every 3 to 6 months. And you need to know the signs: swelling in one leg, sudden shortness of breath, unexplained bruising, or bleeding that won’t stop. These aren’t "maybe" symptoms. They’re red flags.
Below, you’ll find real comparisons, case-based insights, and practical guidance from people who’ve walked this path. We cover how hormonal birth control interacts with common blood thinners, what alternatives exist, and how to talk to your doctor without sounding paranoid. No fluff. No guesswork. Just what works — and what doesn’t — when your body’s trying to prevent pregnancy and prevent clots at the same time.
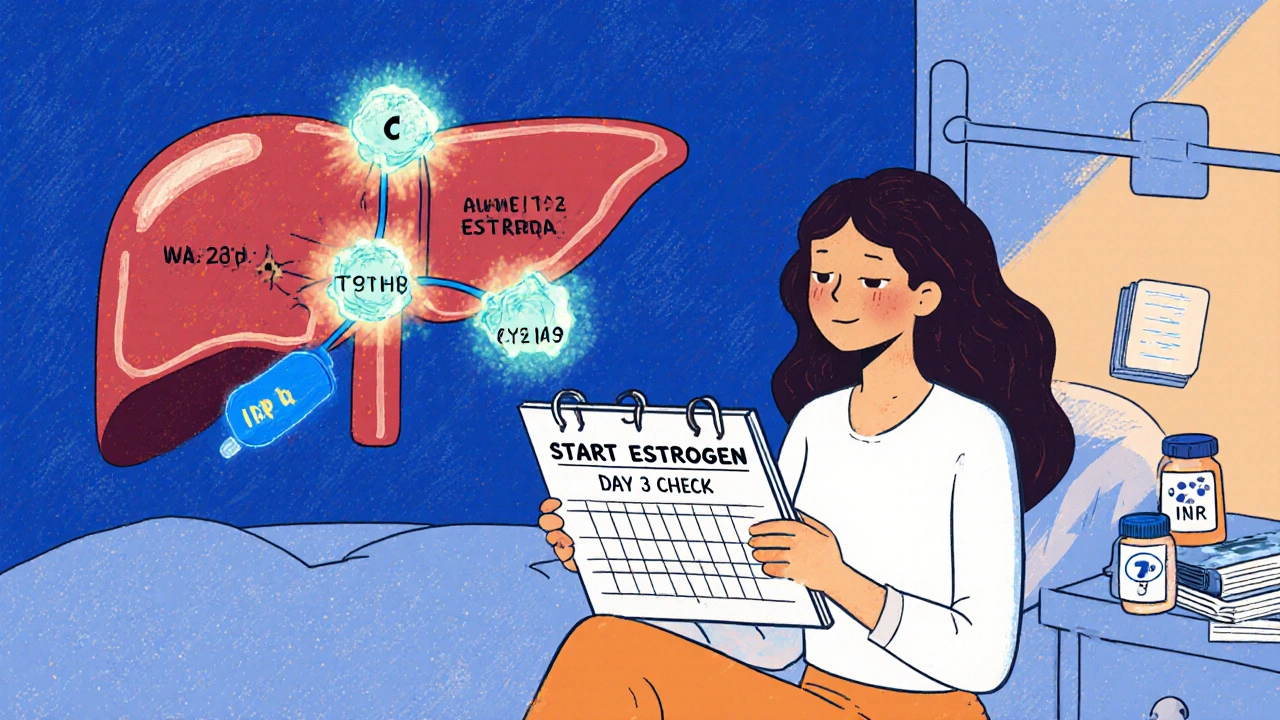
Estrogen Interactions with Warfarin: What You Need to Know About Blood Thinners and Hormones
Estrogen can alter how warfarin works in your body, causing dangerous INR swings. Learn how birth control, HRT, and genetics affect your blood thinner, and what steps to take to stay safe.





