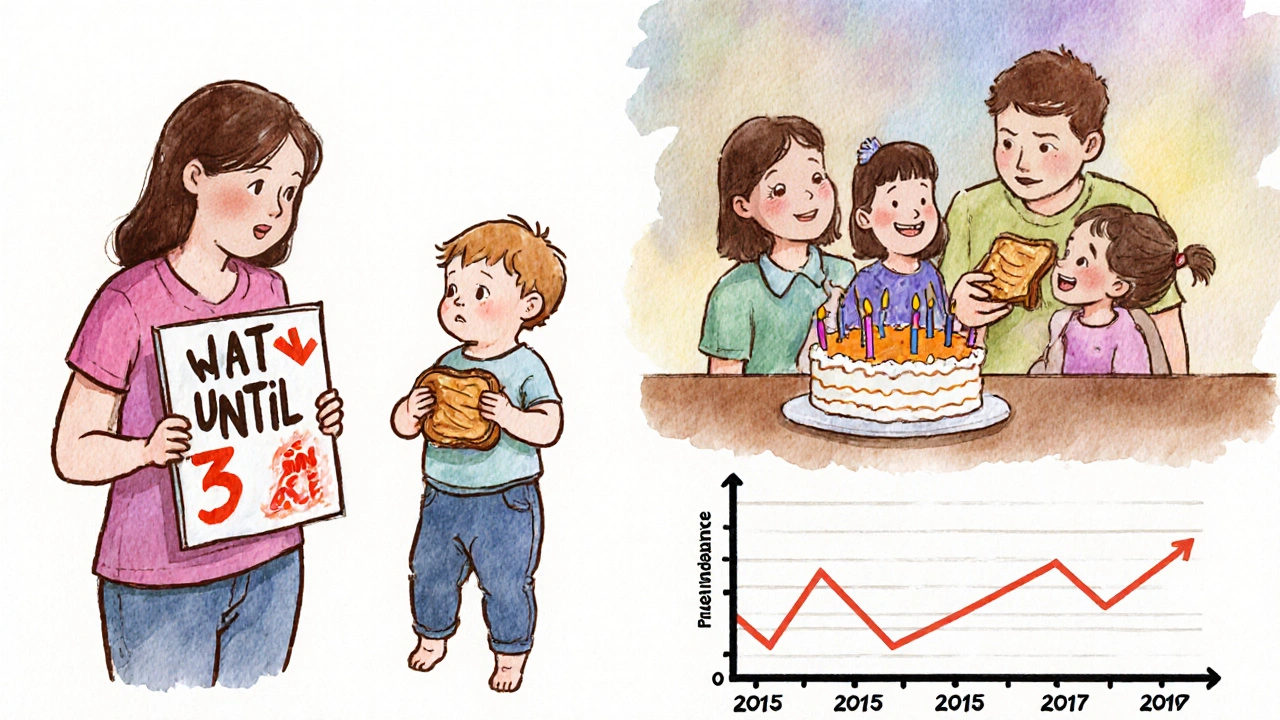
For years, parents were told to wait until their child was two or three before introducing peanuts. The logic seemed simple: delay exposure, reduce risk. But by 2015, peanut allergies had more than quadrupled since the 1990s. Something was wrong. Then came the LEAP study - a landmark trial that flipped everything on its head. It showed that waiting didn’t protect kids. It made them more likely to develop a life-threatening allergy.
Why Early Introduction Works
The science is clear: introducing peanut protein to babies between 4 and 6 months old can cut their risk of developing a peanut allergy by up to 98%. This isn’t a guess. It’s based on data from over 600 infants in the LEAP study, followed by real-world results across the U.S. and Australia. The key isn’t just introducing peanuts - it’s introducing them early, consistently, and safely.
Before 2015, the American Academy of Pediatrics advised delaying peanut exposure. That advice coincided with a sharp rise in peanut allergies. After the LEAP findings, the National Institute of Allergy and Infectious Diseases (NIAID) released new guidelines in 2017. They didn’t just tweak the rules - they rewrote them. Now, the goal isn’t avoidance. It’s early, controlled exposure.
Here’s how it works: your baby’s immune system learns what’s safe when it’s still young and flexible. If peanut protein enters the gut early, the body sees it as food - not a threat. Delay exposure, and the immune system may misread it as dangerous. That’s when allergies form.
Three Risk Levels, One Simple Rule
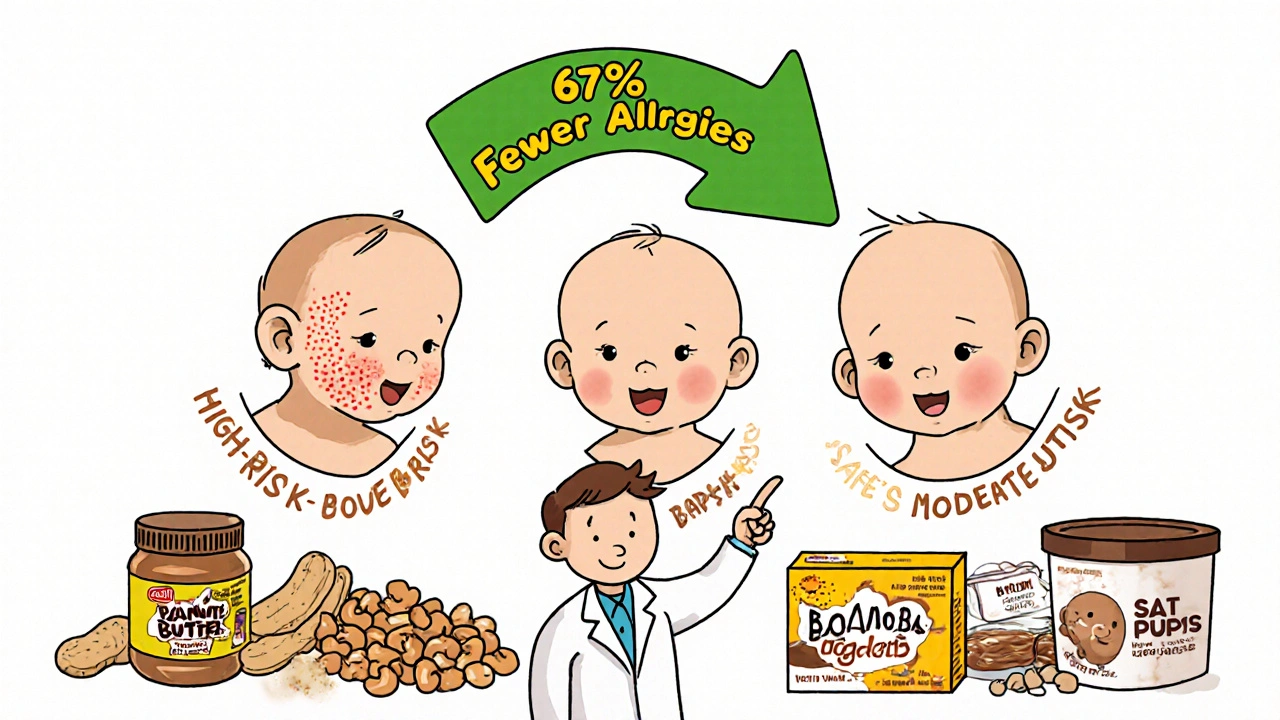
Not all babies need the same approach. The NIAID guidelines split infants into three groups based on risk:
- High-risk: Babies with severe eczema, egg allergy, or both. These kids need medical evaluation before starting.
- Moderate-risk: Babies with mild to moderate eczema. These can start peanut at home around 6 months.
- Low-risk: Babies with no eczema or food allergies. Introduce peanut anytime after starting solids, usually around 6 months.
For high-risk infants, the first peanut exposure should happen under medical supervision. A pediatrician or allergist may do a skin prick test or blood test to check for sensitization. If the result is negative, parents are told to give 2 grams of peanut protein - about two teaspoons of smooth peanut butter - three times a week.
That’s not a one-time thing. Consistency matters. One dose won’t do it. You need three times a week, for months. The LEAP study used peanut butter mixed with warm water, or a peanut-based snack called Bamba. You can also mix peanut butter into oatmeal, yogurt, or pureed fruits.
What Not to Do
Whole peanuts? Never. Choking risk is too high. Peanut butter must be smooth, not chunky. Avoid peanut flour or crunchy peanut butter until the child is older. Don’t try to introduce peanut on its own - mix it into something familiar. And never wait until your baby is older than 11 months if they’re high-risk. The window for prevention closes fast.
A 2022 study found that only 38.7% of high-risk infants in the U.S. actually got early peanut exposure, even though guidelines had been out for five years. Why? Fear. Confusion. Lack of clear advice from doctors. Many parents are scared of anaphylaxis. But the risk of a reaction during supervised introduction is extremely low - far lower than the risk of developing a lifelong allergy.
Oral Immunotherapy (OIT) Is Not Prevention
Don’t confuse early introduction with oral immunotherapy (OIT). OIT is for kids who already have a peanut allergy. It involves giving tiny, increasing doses of peanut under strict medical care to build tolerance. It’s not a cure. It’s management. And it’s risky - reactions are common during treatment.
Early introduction is prevention. It’s for babies without allergies. It’s safe, simple, and proven. OIT is treatment. It’s complex, expensive, and only for those who already react to peanuts. Mixing them up can cost you time - and your child’s health.
Real Results, Real Numbers
The data speaks for itself:
- Peanut allergy rates in U.S. children dropped from 2.2% in 2015 to 1.6% in 2023 - that’s about 300,000 fewer kids with peanut allergies.
- Among high-risk infants with severe eczema, early introduction led to a 67% reduction in allergy rates.
- For mild eczema, the drop was 85%. For moderate eczema, 87%.
- A 2023 study in JAMA Pediatrics found a 35% lower chance of developing peanut allergy after the 2017 guidelines were adopted.
The LEAP study followed kids for years. Even after they stopped eating peanuts for 12 months, most still didn’t react. That’s not just desensitization - it’s true tolerance. The immune system learned to accept peanut as food.
Barriers Still Exist
Despite the science, gaps remain. A 2023 study found Black and Hispanic infants were 22% less likely to get early peanut exposure than White infants. That’s not a medical issue - it’s a system issue. Parents in underserved communities often don’t get clear guidance. Pediatricians may not be up to date. Some still tell families to wait.
And then there’s the confusion about what to feed. Not all peanut products are equal. Smooth peanut butter, diluted with water or breast milk, is ideal. Peanut puff snacks designed for babies (like Bamba or Peanut Butter Puffs) are also safe. Avoid products with added sugar, salt, or honey. And never use whole peanuts, peanut butter straight from the jar, or crunchy varieties.
What’s Next?
Researchers are now testing whether introducing multiple allergens - peanut, egg, milk - together gives even better protection. The EAT study extension showed promising results. The NIAID-funded PRESTO trial, expected to wrap up in 2026, will refine dosing and timing for high-risk babies.
One thing is certain: the era of avoidance is over. The new standard is early, consistent, and guided exposure. It’s not just safer. It’s life-changing.
How to Get Started
If your baby is high-risk (severe eczema or egg allergy):
- See your pediatrician by 3-4 months.
- Ask about referral to an allergist for testing.
- If testing is negative, start with 2g of peanut protein (2 tsp smooth peanut butter) three times a week.
- Begin the first dose in the doctor’s office if recommended.
- Continue until age 5 - don’t stop after a few weeks.
If your baby is moderate-risk (mild eczema):
- Start around 6 months, at home.
- Use smooth peanut butter mixed into puree or cereal.
- Give 2g three times a week.
If your baby is low-risk:
- Introduce peanut anytime after starting solids - usually 6 months.
- No testing needed.
- Just make sure it’s smooth and safe.
Always watch for signs of reaction: hives, vomiting, swelling, trouble breathing. If any occur, stop and call your doctor.
Can I give my baby peanut butter straight from the jar?
No. Whole or chunky peanut butter is a choking hazard. Always thin smooth peanut butter with warm water, breast milk, or formula. Mix it into cereal, yogurt, or pureed fruit. The goal is to make it safe and easy to swallow.
Is it too late to start if my baby is 8 months old?
It’s not ideal, but not hopeless. The best window is 4-6 months, but studies show benefits up to 11 months - especially for high-risk infants. Don’t wait until 12 months or older. The protective effect drops sharply after that. Talk to your pediatrician or allergist about testing and safe introduction.
Do I need to test my baby before introducing peanut?
Only if your baby is high-risk - meaning they have severe eczema or an egg allergy. In those cases, a skin prick or blood test is recommended before the first exposure. For moderate or low-risk babies, testing isn’t needed. You can start at home with smooth peanut butter.
What if my baby has a reaction during introduction?
Stop immediately and contact your doctor. Mild reactions like a few hives or a rash may mean you need to pause and try again later under supervision. Serious reactions - swelling, vomiting, trouble breathing - require emergency care. Never attempt early introduction alone if your baby is high-risk. Always consult a professional first.
Can I prevent peanut allergy by avoiding it during pregnancy?
No. Studies show no benefit from avoiding peanuts during pregnancy or breastfeeding. In fact, maternal diet has no proven effect on preventing peanut allergy in babies. The only proven strategy is introducing peanut to the infant between 4 and 11 months of age.
Are peanut allergy prevention products worth buying?
Specialized peanut puff snacks or pouches are safe and convenient, but not necessary. You can use regular smooth peanut butter diluted with water or breast milk. The key is the amount and frequency - 2g of peanut protein three times a week - not the brand. Avoid products with added sugar, salt, or honey.
Final Takeaway
Peanut allergy isn’t inevitable. It’s preventable. The science is solid. The guidelines are clear. The window is small - but open. For high-risk babies, early introduction can mean the difference between a lifelong allergy and a safe, normal diet. For others, it’s just good practice. Don’t wait. Don’t overthink it. Talk to your doctor. Start early. And give your child the gift of safety - one spoonful at a time.







Cynthia Boen
November 25, 2025 AT 19:22Why are we trusting a study funded by peanut companies? This feels like corporate propaganda dressed up as science.
Gina Banh
November 27, 2025 AT 04:55My son was high-risk-severe eczema, egg allergy. We did the skin test at 4 months, started 2 tsp peanut butter diluted in oatmeal three times a week. No reaction. Now he’s 3 and eats PB&J like a normal kid. This isn’t magic. It’s medicine.
Douglas Fisher
November 28, 2025 AT 10:40My daughter had a mild rash after her first peanut exposure-just a few little red dots. We paused for a week, then tried again with half the amount. She’s fine now. I wish more pediatricians would tell parents this isn’t a gamble-it’s a protocol.
Deirdre Wilson
November 29, 2025 AT 03:09I gave my baby Bamba like the article said-little puffy snacks. He loved it. Like, really loved it. Like he thought it was candy. I didn’t even know peanut could be so fun. Now he’s obsessed with snacks. Maybe I made a monster.
hannah mitchell
November 29, 2025 AT 17:26My sister waited until 18 months. He’s allergic. I started at 5 months. He eats peanut butter straight off the spoon. I’m not bragging. I’m just saying… follow the science.
Stephanie Deschenes
December 1, 2025 AT 09:57It’s not just about peanut butter. It’s about changing how we think about food and fear. We’ve been scared of allergens for decades. But the body isn’t the enemy. Ignorance is. Early exposure isn’t risky-it’s responsible.
Dan Rua
December 3, 2025 AT 01:22My pediatrician didn’t even mention this until my son was 8 months. I had to Google it myself. 😔 We started then-still better than never. Thank you for sharing this. 🙏
Jesús Vásquez pino
December 4, 2025 AT 10:26Wait so you’re telling me my cousin’s kid got anaphylaxis at 2 because she waited? And now you want me to feed my 4-month-old peanut butter? That’s insane. I’m not a lab rat.
Jaspreet Kaur
December 5, 2025 AT 00:38Life is a series of small risks and big rewards. We protect our kids from germs and then scare them with peanut butter. Maybe the real allergy is to trust. Let them eat. Let them live. Let them be.
Amanda Meyer
December 5, 2025 AT 01:23While the LEAP study is compelling, we must acknowledge systemic disparities in implementation. The 22% gap in exposure among Black and Hispanic infants is not a statistical anomaly-it is a failure of public health infrastructure. Without equitable access to allergists and culturally competent guidance, guidelines remain theoretical. We need policy, not just pamphlets.
Bethany Buckley
December 6, 2025 AT 07:35It’s fascinating how the paradigm shift from avoidance to exposure mirrors the epistemological evolution in immunology-from Cartesian dualism to systems biology. The gut-brain axis, dendritic cell priming, and oral tolerance induction are not merely clinical interventions-they are ontological reconfigurations of human immunity. 🌱✨
Albert Guasch
December 7, 2025 AT 03:38Based on the NIAID 2017 guidelines, the introduction of peanut protein within the window of 4–11 months, at a dose of 2 grams of peanut protein per administration, three times weekly, has demonstrated statistically significant primary prevention efficacy in high-risk populations (p < 0.001). This is not anecdotal. It is evidence-based medicine at its finest.
Ginger Henderson
December 8, 2025 AT 22:30So… we’re just supposed to trust doctors now? I remember when they said smoking was good for babies. 😏