Every year, thousands of people accidentally take two doses of the same medicine-sometimes twice in one day. It’s not because they’re careless. It’s because they’re tired, distracted, or confused. Maybe they forgot if they already took their pill. Maybe two caregivers gave the medicine without knowing the other did. Or maybe they used a kitchen spoon to measure liquid medicine and didn’t realize how much was actually in it. This isn’t rare. In fact, medication double-dosing is one of the most common causes of accidental overdose at home, especially among older adults and young children.
According to the National Council on Patient Information and Education, about half of all medication-related accidents happen right in our homes. And it’s not just prescription drugs. Over-the-counter painkillers, vitamins, and supplements can cause the same problem. Take acetaminophen, for example. It’s in more than 200 different products-from cold medicine to sleep aids. Someone might take Tylenol for a headache, then later take a cold tablet without realizing it also contains acetaminophen. That’s how you get a dangerous buildup in the liver. The U.S. Food and Drug Administration says medication errors cause at least one death every day. Most of them? Preventable.
Why Double-Dosing Happens
It’s easy to assume people just forget. But the real reasons are more complex. One major cause? Multiple caregivers. In homes with children, grandparents, or aging parents, it’s common for more than one person to help with medicine. A parent gives a child medicine at 8 a.m. Then, the grandparent sees the child still looking sick at 10 a.m. and gives another dose. No one knows the first one happened. This scenario accounts for over 40% of pediatric double-dosing cases, according to Children’s Healthcare of Atlanta.
For older adults, the problem often comes from complexity. The average senior takes four to five prescription drugs daily. Add in supplements, pain relievers, and sleep aids, and it’s easy to lose track. A 2023 survey by WesleyLife found that 63% of seniors worry about whether they already took their pill-at least once a week. And 28% admitted they’d accidentally taken a double dose in the past year.
Another hidden risk? Measurement. Kitchen spoons aren’t reliable. A teaspoon can hold anywhere from 2.5 mL to 7.3 mL. If a child’s medicine calls for 5 mL and you use a regular spoon, you might be giving nearly 50% more than intended. That’s enough to cause vomiting, drowsiness, or even liver damage in young kids.
What Actually Works to Stop Double-Dosing
There’s no single magic fix. But combining a few simple, proven methods cuts the risk dramatically.
Use a Pill Organizer
This is the most common and effective tool. A weekly pill box with separate compartments for morning, afternoon, evening, and bedtime makes it obvious what’s been taken. If the morning slot is empty, you know you didn’t take it. If it’s still full, you know you did. St. Louis Children’s Hospital recommends this exact setup. And it works: WesleyLife’s 2023 survey found that 68% of seniors use weekly organizers, and those who do cut double-dosing by 35%.
Look for organizers with clear labels and easy-to-open lids. Some even have alarms built in. But even a basic plastic box from the pharmacy helps. The key is consistency-use it every day, no exceptions.
Set Digital Reminders
Smartphone apps like Medisafe, MyTherapy, or even the built-in calendar on your phone can send alerts. These aren’t just beeps-they track what’s been taken. If you miss a dose, the app asks if you took it later. If you say yes, it updates your log. That stops the cycle of guessing.
A 2022 study in the Journal of Medical Internet Research found users of these apps had an 87% improvement in adherence. Even better? When family members help set up the app, success rates jump. A daughter setting up her dad’s reminders is far more effective than him trying to do it alone.
Combine Tools-It’s the Best Combo
Using just a pill box? You cut errors by 35%. Using just a phone app? Maybe 40%. But using both? That jumps to 62% reduction. That’s not a coincidence. The pill box gives you a visual cue. The app gives you a digital log. Together, they cover the gaps. If you forget to check the box, the app reminds you. If you miss the alert, the box shows you what’s missing.
Write It Down
Keep a simple list: medication name, dose, time, and purpose. Include everything-even vitamins and OTC drugs. Update it every time you start or stop something. This isn’t just for you. It’s for the pharmacist, the doctor, and anyone else who helps with your meds. A 72-year-old patient in a Right at Home case study avoided warfarin toxicity after starting a written journal. She realized she’d taken her morning pill during daylight saving time confusion. The list saved her.
Measure Accurately
Never use a kitchen spoon. Always use the syringe, cup, or dropper that came with the medicine. If you lost it? Ask your pharmacy for a new one-they’ll give it to you free. For kids, this is non-negotiable. Children’s Healthcare of Atlanta found that 86% of emergency visits for medicine poisoning involved kids taking medicine that wasn’t theirs. But even more dangerous? Giving the wrong amount because someone used a spoon.
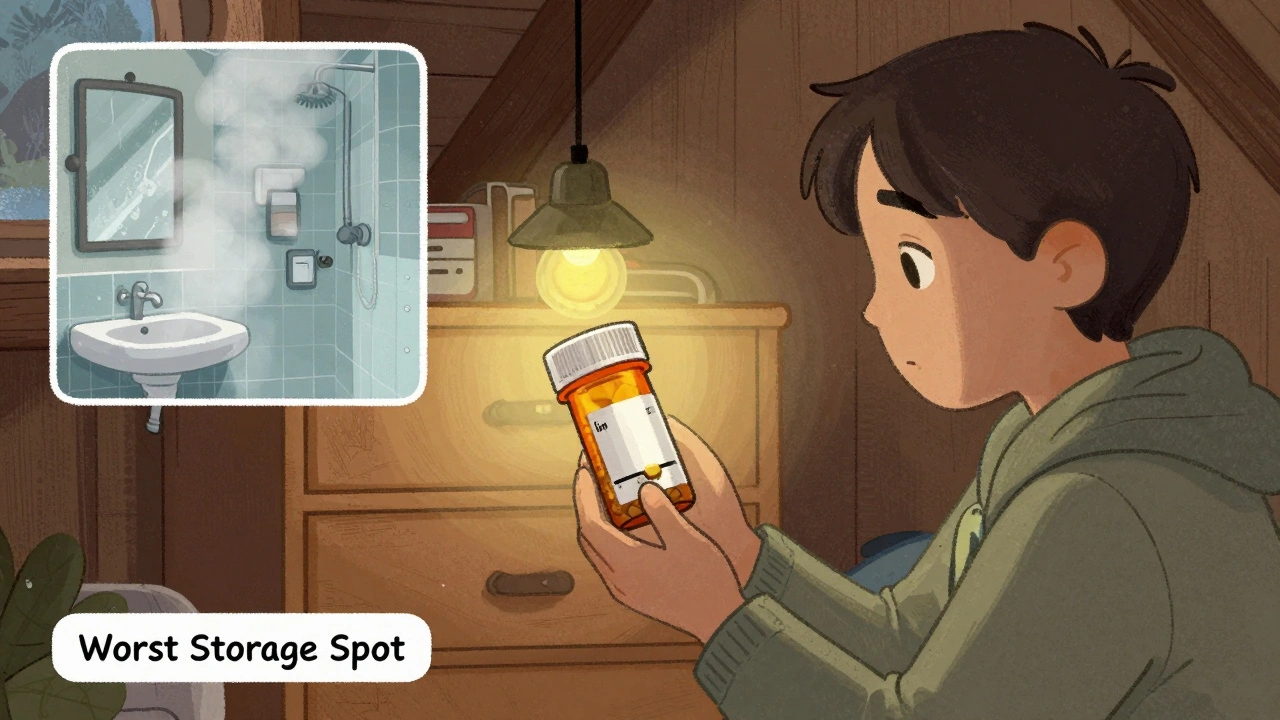
Store Medicine Safely
Keep all medicines out of reach and sight of children. Use locked cabinets if possible. Don’t leave pills on counters, nightstands, or in purses. A child can grab a bottle in seconds. And don’t assume labels are clear. Many medications look identical. A pill that’s meant for high blood pressure might look just like the one for anxiety. That’s why keeping a written list matters.

Special Cases: Kids and Seniors
For children, assign one person as the official medicine giver. It could be mom, dad, grandma-but only one. That person writes down every dose given. If someone else wants to give medicine, they check the list first. This simple rule cuts double-dosing by nearly 50%, according to pediatric pharmacologists at St. Louis Children’s Hospital.
For seniors, avoid switching pill organizers mid-month. If you start a new box on Monday, stick with it. Don’t jump to a different one because the old one ran out. Confusion spikes when routines change. Also, avoid taking medicine with alcohol. It can make side effects worse and mask signs of overdose.
When Things Go Wrong
Even with all these steps, mistakes happen. If you or someone you care for takes too much medicine, don’t wait. Don’t Google it. Don’t hope it’ll pass. Call the Poison Control Center immediately: 1-800-222-1222. It’s free, confidential, and staffed by trained experts. They’ll tell you what to do next-whether it’s watching for symptoms, going to the ER, or doing nothing. And they can help even if you’re not sure what was taken.
Pharmacists are another key resource. Many double-dosing cases happen because people don’t realize two medicines have the same active ingredient. A pharmacist can scan your entire list-prescription and OTC-and flag overlaps. In 2023, EssexCare Pharmacy found that 32% of their double-dosing cases involved hidden duplicates. You’d never catch that on your own.

What’s Coming Next
Technology is getting smarter. Smart pill dispensers now lock after each dose and send alerts to family members if a dose is missed. A 2023 Johns Hopkins study showed these devices cut double-dosing by 76%. AI systems are also being tested-they learn your routine and send alerts like, “You usually take your pill at 8 a.m. It’s now 11 a.m. Did you forget?”
But here’s the truth: the most effective tools are still the simple ones. A pill box. A written list. A phone alarm. A trusted person who knows what’s been given. The future of medication safety isn’t about fancy gadgets. It’s about systems that work even when you’re tired, stressed, or confused.
Start Today
You don’t need to overhaul your whole routine. Pick one thing:
- Get a weekly pill organizer today. Most pharmacies give them for free.
- Set one daily reminder on your phone for your most important pill.
- Write down every medicine you take-right now-and keep it in your wallet.
- Ask your pharmacist to check for duplicate ingredients.
Do one. Then do another next week. Small steps save lives. And in medication safety, there’s no such thing as overdoing prevention.
What should I do if I accidentally take two doses of my medication?
Call the Poison Control Center at 1-800-222-1222 immediately. Don’t wait for symptoms. Don’t try to figure it out on your own. The experts there will tell you whether you need to go to the ER, monitor for side effects, or do nothing at all. Keep this number saved in your phone and posted near your medicine.
Can I use a kitchen spoon to measure liquid medicine?
No. Kitchen spoons vary in size by 20% to 65%. A teaspoon might hold as little as 2.5 mL or as much as 7.3 mL. If your child’s medicine calls for 5 mL, you could be giving nearly double the dose-or half. Always use the measuring device that came with the medicine. If you lost it, ask your pharmacy for a new one. They’ll give it to you free of charge.
Why do I keep forgetting if I took my pill?
It’s normal, especially if you take multiple pills a day or your routine changes. Stress, fatigue, and distractions make memory unreliable. That’s why visual tools like pill organizers and written logs are so important. They replace memory with physical proof. If you see the pill is gone from the box, you know you took it. No guessing needed.
Are over-the-counter medicines safe to take with my prescriptions?
Not always. Many OTC drugs contain the same active ingredients as prescription ones. For example, acetaminophen is in Tylenol, cold medicines, sleep aids, and even some cough syrups. Taking two at once can lead to liver damage. Always check the “Active Ingredients” list on the label. If you’re unsure, ask your pharmacist. They can scan all your meds and flag hidden duplicates.
How can I help an aging parent avoid double-dosing?
Start with a weekly pill organizer and set up a daily phone reminder together. Write down every medication, including vitamins and supplements. Assign one person to be the official medicine giver. Visit the pharmacy together and ask the pharmacist to review all medications for overlaps. Keep the list updated and check it weekly. Small habits make big differences.
Is it safe to use a pill organizer for all medications?
Most are, but not all. Some pills are sensitive to light, moisture, or heat. Check with your pharmacist. For example, sublingual tablets, certain antibiotics, or insulin injections shouldn’t be stored in standard organizers. If a pill looks different after being in the box, or if it smells odd, don’t take it. When in doubt, ask.
What if I travel or my routine changes?
Travel and schedule changes are top triggers for double-dosing. Always pack extra pill organizers. Bring your written medication list. Set travel alerts on your phone. If you’re staying with someone else, give them a copy of your list. Never rely on memory when your routine is disrupted. Even one missed step can lead to a mistake.





Betty Kirby
February 16, 2026 AT 03:31People treat medication like it's candy. You think you're being careful, but you're just lazy. Pill organizers aren't optional. They're the bare minimum. If you can't be bothered to sort your pills into a box with labeled compartments, you shouldn't be in charge of your own health. No excuses. Your grandmother had a handwritten log on her fridge. You have a phone with 87 apps. Use one of them.
Erica Banatao Darilag
February 16, 2026 AT 15:09I just wanted to say thank you for writing this. My mother has dementia and I’ve been terrified of her double-dosing. We started using a pill organizer last month and I’ve noticed she’s calmer, less confused. It’s not perfect, but it’s the first time in years I feel like we’re not just winging it. I’ll keep updating the list every Sunday. Small steps, like you said.
Josiah Demara
February 17, 2026 AT 22:14Let’s be real - this whole post is just a PSA dressed up as a life hack. The real issue is that our healthcare system is broken. Why are people taking 5+ prescriptions? Why are OTC meds not regulated like controlled substances? Why is the FDA letting acetaminophen be in 200 products without a unified dosing standard? This isn’t about memory. It’s about corporate greed and regulatory failure. You want to prevent overdoses? Ban combination products. Force single-ingredient labeling. Stop treating symptoms and fix the system.
And no, a pill box won’t save you if your doctor keeps prescribing overlapping meds. I’ve seen it. I’ve worked in pharmacy. This isn’t a personal responsibility issue. It’s institutional negligence.
Charlotte Dacre
February 18, 2026 AT 05:42So let me get this straight - we’re living in the future, yet we still need a physical box with little holes to remember if we took our pill? And we’re calling this progress? I’m just waiting for the day someone dies because their smart fridge forgot to text them about their blood pressure med.
Also, why is no one talking about how pharmacies don’t even warn you when you’re buying two meds with the same ingredient? I bought NyQuil and Advil last week. No one said a word. Guess what? They both had acetaminophen. I’m not dumb. I just didn’t know. That’s on the system.
Esha Pathak
February 18, 2026 AT 09:08Life is a river, and memory is a leaf floating on its surface - carried by currents we cannot control. The pill organizer? It is not a tool. It is a raft. The digital reminder? A compass. But the true medicine is not in the box or the app. It is in the stillness between the doses - the pause, the breath, the moment you ask yourself: ‘Am I doing this for me, or because I am afraid?’
When the body is tired, the soul remembers. The mind forgets. Trust the silence. Let the pill box be a mirror, not a master.
ॐ
Mike Hammer
February 19, 2026 AT 10:54My grandma used to take her meds with a shot of whiskey. ‘Helps it go down,’ she’d say. She never double-dosed. Just never forgot. I think she had a sixth sense for it. Anyway, I got the free pill box from CVS last week. Put all my stuff in it - even the gummy vitamins. Now I can’t lie to myself. If it’s still there, I didn’t take it. Simple. No app. No list. Just a plastic box and a little honesty.
Also, never use a spoon. I did once. Kid ended up in the ER. Not worth it.
Kapil Verma
February 21, 2026 AT 00:02Why are Americans so incompetent with basic medicine? In India, we have a system - one person handles all meds, and the family keeps a handwritten ledger in Hindi and English. No phones. No apps. Just pen and paper. You think your smartphone is smart? We’ve been doing this for centuries. You don’t need tech. You need discipline. And maybe a little humility.
Also, why is this even a topic? In our village, if you double-dose, your relatives come over and slap you. Problem solved.
Michael Page
February 21, 2026 AT 04:43I’ve been taking three different blood pressure meds for six years. I still forget sometimes. I don’t feel guilty. I feel tired. This isn’t about laziness. It’s about cognitive load. We ask people to manage complex systems while they’re grieving, working two jobs, or raising kids alone. The pill box helps. But it’s not a fix. It’s a Band-Aid on a broken system.
I read this whole thing. I didn’t cry. But I did pause. And that’s rare.
Mandeep Singh
February 22, 2026 AT 19:46Let me tell you something - this is why America is falling apart. You give people a pill box and think that’s enough? You think a plastic container with compartments will fix a society that can’t even agree on what a teaspoon is? I’ve seen people in India take 17 pills a day - and they remember every one. Why? Because they’re taught discipline from childhood. They’re taught responsibility. Not by apps. Not by alarms. By culture.
And you want to know what really prevents double-dosing? A mother who watches. A son who checks. A daughter who writes it down. Not technology. Human connection. That’s what’s missing. Not your fancy organizer. Not your damn app. Your family. You’ve outsourced care to plastic and pixels. And now you’re surprised people are dying?
Stop looking for gadgets. Start looking in the mirror. Who’s holding your hand when you forget? If the answer is ‘no one,’ then you already lost.
And before you say ‘I live alone’ - that’s your problem, not mine.
Kaye Alcaraz
February 23, 2026 AT 16:04One action. One change. That’s all it takes. Start today. Not tomorrow. Not next week. Today. Get the pill organizer. Write down one medication. Set one reminder. That’s it. No need to overhaul your life. Just one step. Then another. You don’t have to be perfect. You just have to begin. And you will. Because you care. And that’s enough.