INR Fluctuations: What Causes Them and How to Manage Them
When you're on a blood thinner like warfarin, a vitamin K antagonist used to prevent dangerous blood clots. Also known as Coumadin, it requires regular monitoring to stay effective and safe. Your INR, the International Normalized Ratio, measures how long it takes your blood to clot is one of the most important numbers in your health routine. If your INR is too low, you risk clots that can cause strokes or heart attacks. Too high, and you could bleed internally—sometimes without warning. INR fluctuations, unexpected changes in your clotting time that aren't due to missed doses are common, but they shouldn’t be ignored.
What causes these swings? It’s rarely just one thing. Your diet plays a big role—eating lots of leafy greens like spinach or kale can drop your INR because they’re full of vitamin K, which warfarin fights against. Alcohol, even a few drinks, can spike your INR. Some antibiotics, antifungals, and even herbal supplements like St. John’s wort or ginkgo biloba can interfere with how your body breaks down warfarin. Even small changes in your sleep, stress levels, or how well your liver is working can throw your INR off. And here’s the thing: your body isn’t static. As you age, gain or lose weight, or start a new medication, your warfarin needs change. That’s why a single dose rarely lasts forever.
Managing INR fluctuations isn’t about perfection—it’s about awareness. Keep a simple log: what you ate, any new meds, how much you drank, and your INR results. Share this with your doctor at every checkup. Don’t switch brands of warfarin without telling your provider—generic versions aren’t always interchangeable in practice. If your INR jumps or drops suddenly, don’t panic, but don’t wait either. Call your clinic. Most people on warfarin need testing every 2 to 6 weeks, but if your INR is unstable, you might need it weekly until things settle. The goal isn’t to hit the same number every time—it’s to stay in your target range, which for most people is between 2.0 and 3.0, though it can vary based on your condition.
Below, you’ll find real-world comparisons and practical guides from people who’ve walked this path. From how certain antibiotics affect INR levels, to what happens when you mix warfarin with common pain relievers, to how diet changes can make or break your stability—these posts cut through the noise. No theory. No fluff. Just what works, what doesn’t, and what you need to know before your next blood test.
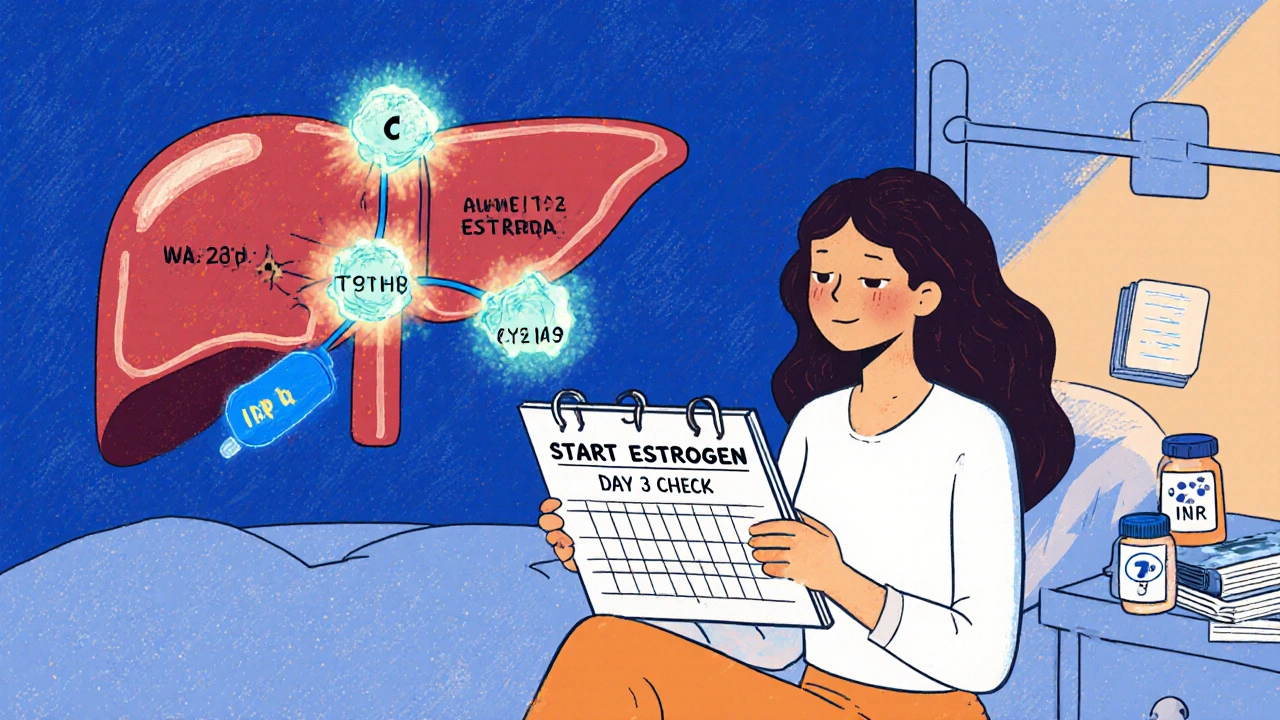
Estrogen Interactions with Warfarin: What You Need to Know About Blood Thinners and Hormones
Estrogen can alter how warfarin works in your body, causing dangerous INR swings. Learn how birth control, HRT, and genetics affect your blood thinner, and what steps to take to stay safe.





