Estrogen and Warfarin Interaction: What You Need to Know
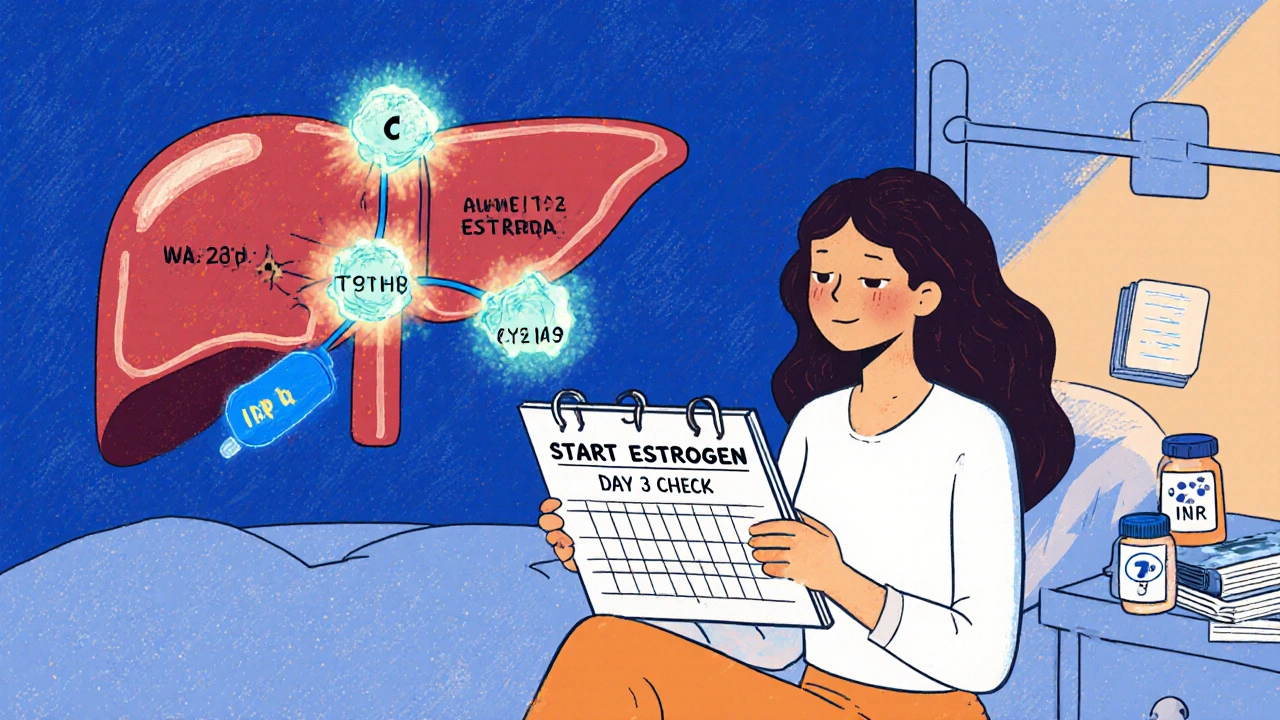
When you take estrogen, a hormone used in birth control, menopause treatment, or gender-affirming care. Also known as estradiol, it can change how your body processes blood thinners like warfarin. This isn’t just a footnote in a drug leaflet—it’s something that can make your INR spike or drop, putting you at risk for clots or bleeding. If you’re on warfarin, a blood thinner used to prevent strokes, clots, and heart complications. Also known as Coumadin, it’s one of the most common medications with tricky interactions. Adding estrogen into the mix isn’t always dangerous, but it demands attention.
Estrogen can make warfarin work harder. That means your blood takes longer to clot, and your INR goes up. You might not feel anything at first—no bruising, no dizziness—but a small cut could bleed longer than normal, or worse, you could have an internal bleed. On the flip side, if you stop estrogen—like after switching birth control or ending hormone therapy—your warfarin might suddenly become less effective. That’s when clots can form without warning. People on long-term estrogen therapy, especially postmenopausal women or those on gender-affirming treatment, often need more frequent blood tests. One study from the Journal of Thrombosis and Haemostasis tracked over 1,200 patients and found that estrogen users had a 30% higher chance of needing a warfarin dose change within 30 days of starting or stopping.
It’s not just about the dose. The type of estrogen matters. Oral estrogen—like pills—has a stronger effect than patches or gels. Why? Because pills go through your liver first, where they boost clotting factors that warfarin tries to suppress. Patches skip that step, so they’re usually safer. And if you’re on a combination therapy—say, estrogen plus progestin—watch out. Progestin can muddy the waters, sometimes balancing the effect, sometimes making it worse. Also, don’t forget other meds. Antibiotics, antifungals, even some herbal supplements like St. John’s Wort can change how warfarin works. Your pharmacist isn’t just there to hand out pills—they’re your first line of defense.
What should you do? If you’re starting estrogen while on warfarin, get your INR checked within 3–5 days. Same if you stop. Don’t wait for symptoms. Keep a log of your doses, your INR numbers, and any new symptoms—unusual bruising, nosebleeds, dark stools, sudden headaches. Talk to your doctor before switching brands or forms of estrogen. And if you’re using over-the-counter supplements or herbal remedies, tell your provider. They might not ask, but they need to know.
This isn’t about avoiding estrogen or warfarin. It’s about managing them together safely. Thousands of people take both without issues—because they’re informed, they test regularly, and they communicate with their care team. The posts below give you real-world comparisons, case-based advice, and clear guidance on how hormonal therapies interact with other drugs. You’ll find what works, what doesn’t, and what to watch for—no fluff, no jargon, just what you need to stay safe.
Estrogen Interactions with Warfarin: What You Need to Know About Blood Thinners and Hormones
Estrogen can alter how warfarin works in your body, causing dangerous INR swings. Learn how birth control, HRT, and genetics affect your blood thinner, and what steps to take to stay safe.





