CYP450 Enzyme Interactions: How Medications Affect Each Other
When you take more than one medication, your body doesn’t treat them like separate events—it’s all one chemical conversation happening in your CYP450 enzymes, a family of liver proteins that break down drugs and other substances. Also known as cytochrome P450 enzymes, these are the main gatekeepers deciding how fast your body processes pills, from antidepressants to blood pressure drugs. If one drug slows down these enzymes, another drug can build up to dangerous levels. If one speeds them up, your meds might not work at all. This isn’t theory—it’s why some people get sick after adding a new supplement or why their painkiller suddenly stops helping.
These enzymes don’t work in isolation. They’re affected by antibiotics, like clarithromycin or erythromycin, which can block enzyme activity, by antifungals, such as ketoconazole, known to sharply reduce drug metabolism, and even by common things like grapefruit juice or St. John’s wort. That’s why gender-affirming hormones, ED meds like sildenafil, or even over-the-counter painkillers can behave unpredictably when mixed with other substances. The same enzymes that break down your blood pressure pill also handle your antidepressant, your cholesterol drug, and your sleep aid. Change one, and the whole system shifts.
It’s not just about pills. Your diet, your liver health, even your genes play a role. Some people naturally have slower CYP450 activity—meaning they’re more sensitive to side effects. Others process drugs so fast they need higher doses just to feel the effect. That’s why a drug that works perfectly for your friend might leave you dizzy or nauseous. And when you’re taking something like finasteride for hair loss, or mefenamic acid for pain, or even doxycycline for an infection, you’re still riding the same biochemical highway. The risk isn’t always obvious, but the consequences can be serious: liver stress, heart rhythm issues, or meds that just stop working.
What you’ll find below are real-world examples of how these interactions play out. From how Kamagra Oral Jelly reacts with heart meds, to why Fucidin cream might be safer than other topical antibiotics for some people, to how gender-affirming hormones interact with HIV drugs—these aren’t abstract concepts. They’re the kind of details that keep you safe. You don’t need to memorize every enzyme subtype. But you do need to know when to ask your pharmacist: ‘Could this change how my other meds work?’ Because the answer could mean the difference between feeling better—and ending up in the hospital.
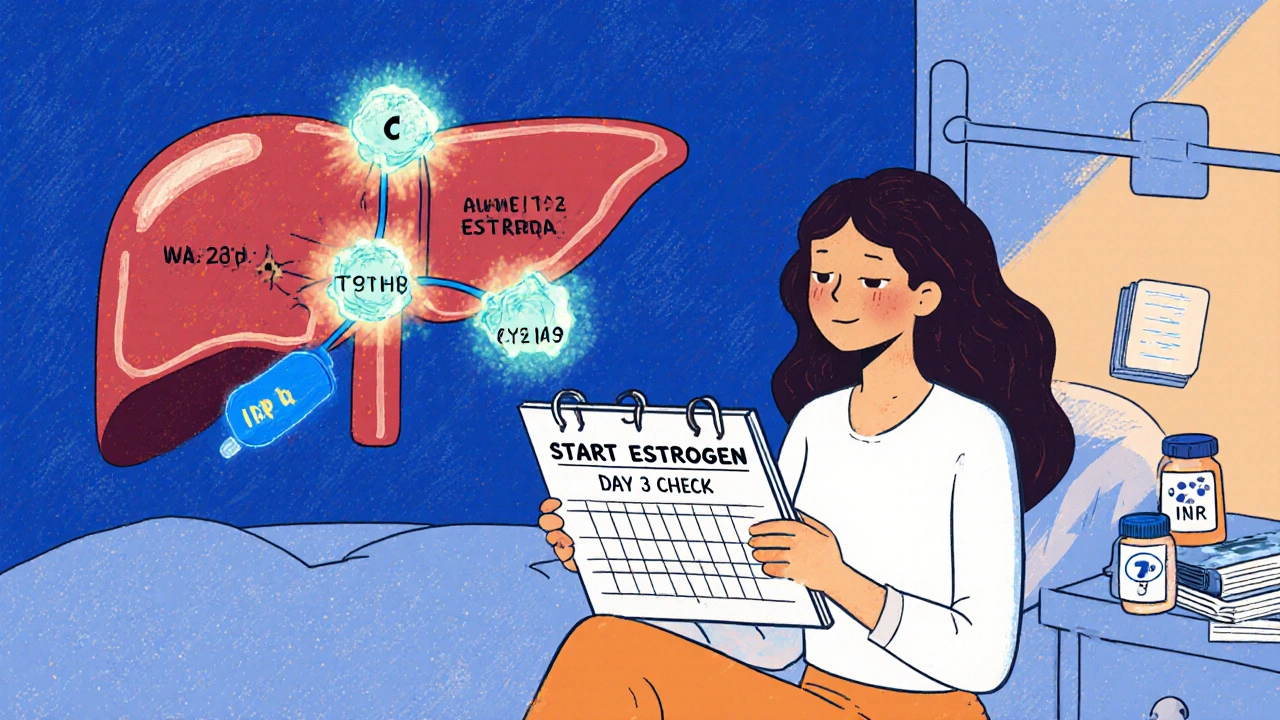
Estrogen Interactions with Warfarin: What You Need to Know About Blood Thinners and Hormones
Estrogen can alter how warfarin works in your body, causing dangerous INR swings. Learn how birth control, HRT, and genetics affect your blood thinner, and what steps to take to stay safe.





