TB Risk Estimator
This tool estimates how climate conditions might influence pulmonary tuberculosis risk in your area.
TL;DR:
- Rising temperatures and humidity expand the geographic window for Pulmonary Tuberculosis (a bacterial lung disease caused by Mycobacterium tuberculosis).
- Air‑pollution spikes during heatwaves increase susceptibility by damaging lung defenses.
- Climate‑driven migration and poverty concentrate vulnerable populations, boosting transmission.
- Co‑factors such as HIV, malnutrition, and weakened BCG vaccine effectiveness amplify the impact.
- Targeted public‑health actions - climate‑resilient TB screening, improved ventilation, and socioeconomic support - can blunt the trend.
Why Climate Matters for a Bacterial Infection
When you hear the term climate change, most people picture melting ice caps or extreme storms. What they often miss is how a shifting climate reshapes the microscopic world inside our lungs. The bacterium Mycobacterium tuberculosis thrives in warm, moist environments. As average global temperatures climb and weather patterns become erratic, the pathogen finds new niches, and the human immune system faces fresh challenges.
Temperature, Humidity, and the TB Transmission Window
Historically, high TB incidence clustered in cooler, densely populated cities where ventilation was poor. Recent epidemiological models, however, show a northward drift. In regions where the mean annual temperature rises above 15°C and relative humidity climbs past 70%, sputum droplets linger longer, allowing the bacteria to remain viable for up to 48hours-double the life span recorded in drier climates.
For example, a longitudinal study in the United Kingdom (2022‑2024) linked a 1°C rise in average winter temperature to a 4% increase in newly reported pulmonary TB cases across the North‑West. Similar patterns emerge in sub‑Saharan Africa, where expanding savanna zones now experience temperature regimes once confined to equatorial basins.
Air Pollution: The Invisible Co‑Conspirator
Heatwaves amplify particulate matter (PM2.5) concentrations as stagnant air traps pollutants. Chronic exposure to PM2.5 compromises alveolar macrophage function-the first line of defense against inhaled Mycobacterium tuberculosis. A meta‑analysis of 18 cohorts (2020‑2023) found that a 10µg/m³ increase in PM2.5 correlates with a 7% rise in TB infection risk.
Urban centers like Delhi or Lagos, already battling severe smog, now see TB notification rates spiking after prolonged heat alerts. The synergy between poor air quality and climate‑induced temperature shifts creates a perfect storm for TB outbreaks.
Socio‑Economic Disruption and Population Mobility
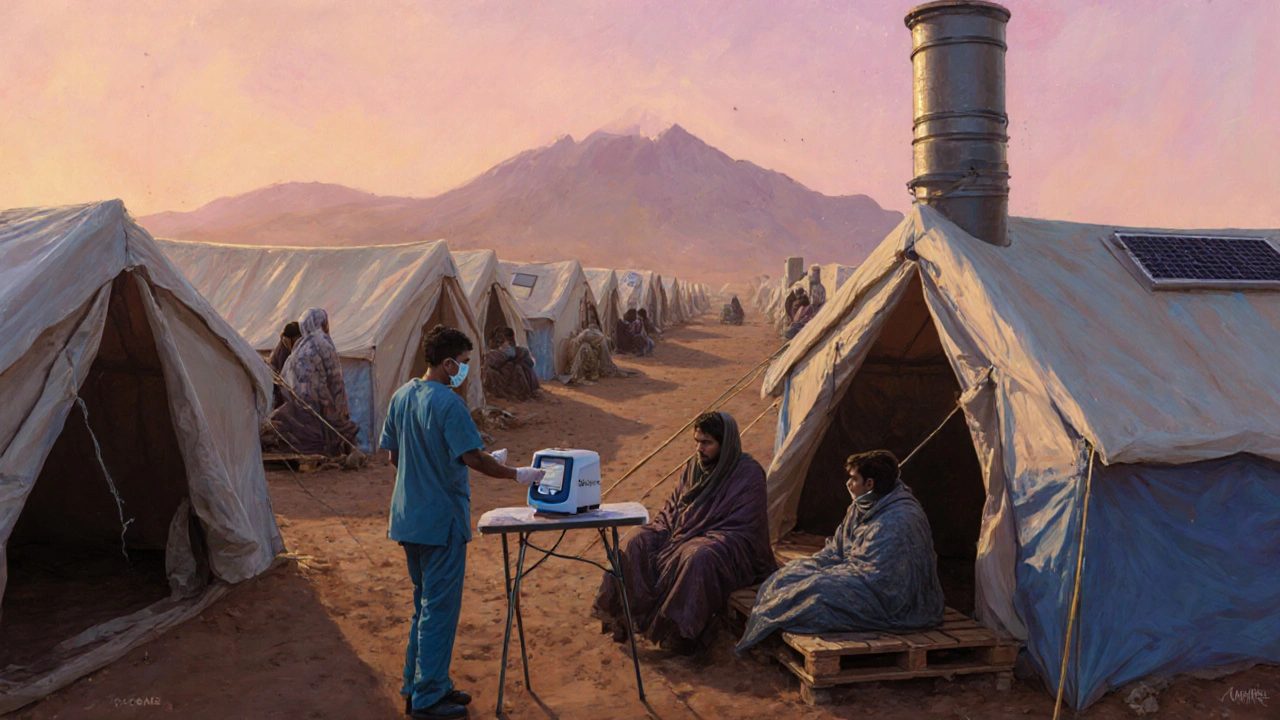
Beyond the physiological effects, climate change triggers massive human displacement. Floods, droughts, and sea‑level rise force millions into temporary shelters where overcrowding and limited health services are the norm. These settings mirror classic TB hotspots: close contact, inadequate ventilation, and delayed diagnosis.
Data from the International Organization for Migration (2024) indicate that refugees from climate‑affected zones have a 12% higher TB prevalence than host‑country averages within the first two years of resettlement. The intersection of poverty, malnutrition, and limited access to BCG vaccination compounds vulnerability.
Intersecting Health Challenges: HIV, Malnutrition, and BCG Efficacy
Two health variables already known to exacerbate TB-HIV co‑infection and malnutrition-are also climate‑sensitive. Warmer temperatures expand the range of malaria‑carrying mosquitoes, increasing HIV transmission in some regions. Meanwhile, crop failures linked to drought reduce protein intake, weakening immune responses.
The BCG vaccine-the only widely used TB preventive measure-shows reduced efficacy in populations with high environmental mycobacterial exposure, a condition more common in humid, warm climates. Consequently, children in rapidly warming zones receive less protection, feeding the cycle of infection.
Mitigation Strategies: Turning Climate Action into TB Control
Addressing TB in a warming world requires a two‑pronged approach: climate adaptation and targeted health interventions.
- Climate‑Resilient Screening. Deploy mobile TB testing units equipped with solar‑powered GeneXpert machines to reach displaced communities during extreme weather events.
- Ventilation Improvements. Retrofit schools and shelters with low‑cost cross‑ventilation designs. In hot climates, stack ventilation can reduce indoor PM2.5 by up to 30% without additional energy use.
- Nutrition Support. Community grain banks and micronutrient supplementation lower malnutrition‑related TB risk by an estimated 15%.
- Integrated HIV‑TB Services. Co‑locate antiretroviral therapy with TB clinics in climate‑vulnerable regions to catch co‑infections early.
- Policy Alignment. Encourage governments to embed TB metrics into national climate‑adaptation plans. Funding streams earmarked for climate resilience can also cover TB surveillance.
Regional Snapshot: TB Prevalence by Climate Zone
| Climate Zone | Average Temp (°C) | Avg. Humidity (%) | TB Incidence | Key Drivers |
|---|---|---|---|---|
| Tropical | 27 | 78 | 215 | High humidity, air‑pollution spikes, limited health access |
| Temperate | 14 | 65 | 132 | Seasonal heatwaves, migration‑related overcrowding |
| Arctic/Sub‑Arctic | 2 | 55 | 64 | Emerging warming, infrastructure strain, Indigenous community risks |
Looking Ahead: Research Gaps and Future Directions
While the link between climate variables and TB is clear, several knowledge gaps persist. Long‑term cohort studies that track individual exposure to heat, humidity, and particulate matter alongside TB outcomes are scarce. Moreover, the interaction between climate‑induced stress hormones and Mycobacterium tuberculosis virulence remains understudied.
Investments in satellite‑derived environmental data combined with national TB registries could unlock predictive models, enabling health ministries to anticipate outbreak hotspots months before cases surge.
Bottom Line
Climate change isn’t just an abstract environmental issue-it’s a direct driver of pulmonary tuberculosis prevalence. By recognizing temperature, humidity, air‑quality, and socio‑economic displacement as core components of TB risk, policymakers, clinicians, and community leaders can forge climate‑smart health strategies that save lives now and into the decades ahead.

Frequently Asked Questions
How does higher humidity affect TB transmission?
In humid air, respiratory droplets evaporate more slowly, keeping the bacteria viable longer. This extended survival window raises the chance that inhaled particles contain enough Mycobacterium tuberculosis to cause infection.
Can improving ventilation really lower TB rates during heatwaves?
Yes. Studies in refugee camps show that simple cross‑ventilation designs reduce indoor airborne TB concentrations by up to 40%. When combined with air‑filtering fans powered by solar panels, the effect is even stronger.
Is the BCG vaccine less effective in warmer regions?
Research suggests that high environmental exposure to non‑tuberculous mycobacteria, which thrives in warm, moist soils, can dampen the immune response triggered by BCG. Consequently, protection levels dip by roughly 10‑15% compared with cooler areas.
What immediate actions can health workers take in climate‑related TB outbreaks?
Deploy rapid molecular testing kits to affected shelters, set up temporary isolation rooms with enhanced ventilation, and provide nutritional supplements to at‑risk individuals. Coordinating with local meteorological services also helps anticipate spikes tied to heat or dust events.
How does climate‑driven migration increase TB risk?
Migrants often live in crowded temporary housing with limited healthcare access. Overcrowding raises the chance of inhaling infectious droplets, while stress and malnutrition weaken immunity, making infection more likely.


Sumeet Kumar
September 30, 2025 AT 20:53Great summary! The link between rising temps and TB is finally getting the attention it deserves 😊.
Maribeth Cory
October 1, 2025 AT 08:00Excellent breakdown of how climate stressors amplify TB risk. It's crucial we push for climate‑resilient health policies now. Communities worldwide will benefit from this integrated approach.
andrea mascarenas
October 1, 2025 AT 19:06Interesting data on humidity extending droplet viability. This could explain recent spikes in temperate zones.
Vince D
October 2, 2025 AT 06:13Heatwaves + smog = a bad combo for lung health.
Camille Ramsey
October 2, 2025 AT 17:20Look, the science is crystal clear, but ppl keep acting like climate is some far‑off fantasy. Stop whining and fund the TB screenings already!
Scott Swanson
October 3, 2025 AT 04:26Oh sure, because throwing money at a problem magically makes the bacteria disappear. Maybe we should also invent a climate‑proof BCG while we're at it.
Karen Gizelle
October 3, 2025 AT 15:33While everyone's busy blaming the weather, we must remember that personal responsibility plays a role too. Individuals need to seek vaccination, maintain nutrition, and avoid overcrowded shelters whenever possible. Ignoring these basics under the guise of climate doom is a disservice to public health.
Stephanie Watkins
October 4, 2025 AT 02:40One often overlooked factor is the seasonal migration of livestock, which can disturb soil microbes and indirectly affect human exposure to environmental mycobacteria. Incorporating veterinary health data could sharpen our predictive models.
Zachary Endres
October 4, 2025 AT 13:46When the mercury soars, it's not just the air that burns-our very breath becomes a battlefield. Imagine cities shrouded in a haze that steals the lungs' armor, leaving us vulnerable to the silent assassin that is TB.
Ashley Stauber
October 5, 2025 AT 00:53Not every rise in TB cases can be pinned on climate; genetic variations of Mycobacterium also drive virulence. Overemphasizing weather risks oversimplifies a complex pathogen.
Amy Elder
October 5, 2025 AT 12:00Cool take on the data. Looks like we have some solid strategies to test in the field.
Will Esguerra
October 5, 2025 AT 23:06It is incumbent upon the global health community to recognize the inexorable link between anthropogenic climate perturbations and the resurgence of pulmonary tuberculosis. Failure to address this nexus portends a grievous increase in morbidity, undermining decades of epidemiological progress.
Ben Poulson
October 6, 2025 AT 10:13The incorporation of satellite-derived climatological metrics into national TB registries represents a methodological advancement of considerable merit. Such integration will enable preemptive allocation of resources, thereby mitigating outbreak severity.
Raghav Narayan
October 6, 2025 AT 21:20The nexus between climate dynamics and pulmonary tuberculosis is emerging as a pivotal area of interdisciplinary research.
Recent longitudinal analyses demonstrate that incremental increases in ambient temperature correlate with measurable upticks in TB incidence across diverse geographical locales.
Moreover, heightened relative humidity extends the survivability of aerosolized Mycobacterium tuberculosis, thereby enhancing transmission efficiency.
Concurrently, escalations in particulate matter, particularly PM2.5, impair alveolar macrophage function, compromising the primary innate defense mechanism against inhaled pathogens.
Climate‑induced displacement further exacerbates risk by concentrating susceptible populations in overcrowded shelters with limited ventilation.
It is essential to recognize that these environmental stressors interact synergistically rather than operating in isolation.
For policymakers, this implies that mitigation strategies must be multi‑pronged, integrating climate adaptation with robust public health interventions.
Deploying mobile, solar‑powered diagnostic units can bridge gaps in care delivery for transient communities during extreme weather events.
Simultaneously, improving passive ventilation in temporary housing can reduce indoor airborne pathogen load by a substantial margin.
Nutritional supplementation programmes should accompany these measures, as malnutrition remains a potent amplifier of TB susceptibility.
Furthermore, aligning TB surveillance metrics with real‑time climate data will afford health authorities the predictive capacity needed to pre‑empt outbreaks.
Integrating these datasets is technically feasible given the proliferation of high‑resolution satellite observations and open‑source analytical platforms.
Investment in such integrative infrastructure promises a favorable cost‑benefit ratio, averting future healthcare expenditures associated with uncontrolled TB spread.
In sum, the confluence of climate change and tuberculosis necessitates a coordinated response that transcends traditional disease‑specific frameworks.
By embracing climate‑smart health policies today, we safeguard both planetary and human health for generations to come.
Tara Phillips
October 7, 2025 AT 08:26Excellent overview; let's act on these recommendations promptly.