When you’re handed a prescription, do you feel like you’re making a choice-or just accepting an order? For too many people, medication decisions feel like something done to them, not with them. But a quiet revolution is happening in clinics, pharmacies, and patient homes: the return of control. Medication autonomy isn’t just a buzzword. It’s the right to say yes, no, or show me another option-based on your life, your values, and your body.
Why Your Body, Your Call
The idea that patients should have final say over what goes into their bodies isn’t new. It came out of the Nuremberg Trials after World War II, when the world realized doctors couldn’t just decide what was best. The legal foundation was solidified in 1972 with the Canterbury v. Spence case, which ruled: doctors must tell you everything that matters before you agree to treatment. That includes side effects, alternatives, costs, and even what happens if you do nothing. Today, that means if your doctor prescribes an SSRI for depression, you’re not just supposed to nod and take it. You’re entitled to know it works for about half of users, but up to 30% experience sexual side effects. You’re allowed to ask: Is there a cheaper version? A non-pill option? A therapy that might help instead? That’s not being difficult. That’s being human.What Autonomy Actually Looks Like in Practice
Autonomy doesn’t mean patients get to pick any drug they want. It means they get to make an informed decision among real options. Here’s how it works in a real clinic:- A patient with type 2 diabetes is offered Ozempic. They’re worried about nausea. Instead of pushing it, the doctor pulls up a decision aid showing three alternatives: metformin (cheaper, GI issues), SGLT2 inhibitors (weight loss benefit, higher UTI risk), and lifestyle coaching with a dietitian.
- A veteran with chronic pain refuses opioids due to religious beliefs. The team doesn’t argue. They adjust the plan: physical therapy, acupuncture, and a non-opioid nerve pain med-adjusted for frequency so it fits her schedule.
- A woman on Medicare sees a $600 monthly bill for a biologic. She didn’t know a biosimilar exists for $3,500 a year. Her pharmacist flagged it during a medication therapy check-up. She switched-and saved $3,000.
The Hidden Barriers: Why Autonomy Often Fails
You’d think this would be easy. But it’s not. Here’s why it often falls apart:- Time crunch: Most doctor visits last 15 minutes. Talking through four drug options, side effects, costs, and personal values? Impossible. A 2023 survey found 63% of patients felt rushed during med discussions.
- System gaps: Only 38% of hospitals using Epic EHR systems have fields to record patient preferences. If it’s not documented, it doesn’t count.
- Cost blind spots: Doctors don’t always know what a drug costs. Patients often find out at the pharmacy-too late. In 2023, 32% of Medicare users changed or skipped meds because of price.
- Cultural silence: One in three immigrant patients say they don’t question doctors because they fear being seen as disrespectful. Autonomy isn’t just about information-it’s about power.
- Marketing noise: Direct-to-consumer ads influence 28% of medication requests. A patient asks for a brand-name drug because they saw it on TV, not because it’s right for them.

What Works: Tools That Actually Help
Change isn’t happening by accident. It’s being built-with tools, training, and policy.- Decision aids: The Mayo Clinic and others offer free, visual tools that compare drugs side-by-side with icons for side effects, cost, and dosing. One study showed these cut patient decision-making stress by 42%.
- Pharmacy-led support: Medication Therapy Management (MTM) services-led by pharmacists-have increased patient autonomy by 31%. Pharmacists have time to talk. They check for interactions, costs, and whether the patient even likes swallowing pills.
- Pre-visit prep: Some clinics now send patients a short questionnaire before the appointment: “What matters most to you in a medication? Cost? Fewest side effects? Once-a-day dosing?” That gives the doctor a roadmap.
- Shared decision-making training: Clinicians who go through 12-18 months of simulation training with standardized patients become much better at uncovering values. One study found they were 50% more likely to offer alternatives.
The Digital Divide: Tech Helps-Unless You’re Over 65
New apps promise to help patients compare meds, track side effects, and set reminders. But here’s the catch: 37% of adults over 65 say they find these apps confusing or too hard to use. That’s not progress-it’s exclusion. Autonomy isn’t about having the fanciest app. It’s about having access to clear, simple, human-centered information. A printed one-pager with big fonts and plain language? That’s still better than a glitchy app for many. The future may include pharmacogenomic testing-blood tests that show how your body processes drugs. The cost has dropped from $1,200 in 2020 to $249 in 2024. That could mean truly personalized meds. But if only wealthier patients get access, autonomy becomes another privilege, not a right.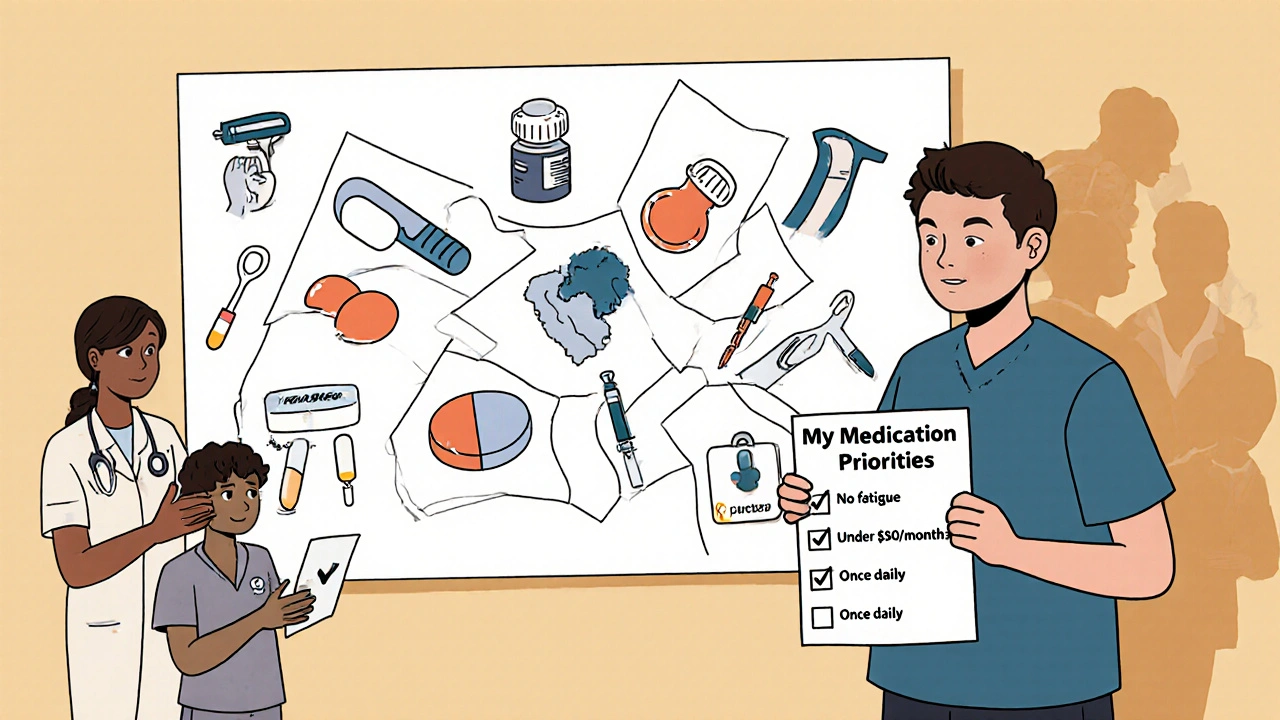
What You Can Do Right Now
You don’t need a perfect system to take back control. Here’s how to start today:- Ask: “What are my options besides this?” Don’t settle for “This is the best one.”
- Ask again: “What happens if I don’t take this?” “What are the most common side effects?” “Is there a generic?”
- Ask about cost: “Can you check if this is covered? Is there a cheaper alternative?” Pharmacists can help-ask them.
- Ask about lifestyle: “Can this be taken once a day?” “Is there a liquid form?” “Will it interfere with my work or sleep?”
- Bring a list: Write down your priorities before your appointment: “I need something that doesn’t make me tired,” or “I can’t afford more than $50 a month.”
The Bigger Picture: Autonomy Is the Future
The American Society of Health-System Pharmacists launched its Medication Autonomy Framework in January 2024. The FDA now requires drugmakers to collect patient preference data. Medicare will require documentation of patient choices by 2025. This isn’t just ethics. It’s efficiency. When patients choose meds they can live with, hospitalizations drop. Adherence rises. Costs fall. The goal isn’t to make every patient a pharmacologist. It’s to make every patient feel like a partner. Because in the end, you’re the one who has to swallow the pill, live with the side effects, and pay the bill. You’re the one who knows your body best. The system isn’t perfect. But it’s changing. And you have more power than you think.Can I refuse a medication my doctor recommends?
Yes. If you have decision-making capacity, you have the legal and ethical right to refuse any medication-even if your doctor believes it’s the best option. Doctors are required to explain the risks of refusing, but they cannot force treatment. This applies to everything from antibiotics to insulin. Your values, beliefs, and life circumstances matter.
What if I can’t afford my prescribed medication?
You’re not alone. In 2023, 32% of Medicare Part D users changed or skipped doses because of cost. Talk to your pharmacist about generic alternatives, patient assistance programs, or biosimilars. Some drugmakers offer coupons. Your doctor can also write a letter of medical necessity to your insurer. Never stop taking a med without talking to your provider-but do ask for help finding a more affordable option.
Are there tools to help me compare medications?
Yes. The Mayo Clinic and other trusted health organizations offer free, visual decision aids that compare drugs by effectiveness, side effects, cost, and dosing. These tools use plain language and icons-not medical jargon. Ask your doctor or pharmacist for them. You can also check the NIH’s MedlinePlus or the Patient-Centered Outcomes Research Institute (PCORI) website for reliable comparisons.
Why do some doctors seem unwilling to discuss alternatives?
Some providers feel pressured by time, lack training in shared decision-making, or hold unconscious biases-like assuming you won’t understand or can’t afford alternatives. Others may believe they’re saving you time by recommending what they think is best. But research shows patients who get more options actually feel more confident and stick with their treatment longer. If you feel dismissed, it’s okay to ask again or seek a second opinion.
Does medication autonomy apply to mental health drugs?
Absolutely-and it’s especially important here. Psychiatric medications often come with side effects that deeply affect daily life: weight gain, emotional numbness, sexual dysfunction. Many patients feel pressured to take them because “everyone does.” But autonomy means you can say no, try a different drug, combine it with therapy, or explore non-drug options like CBT or exercise. Psychiatrists are now among the most likely to use shared decision-making tools, because they know mental health isn’t just about symptoms-it’s about living well.







saurabh lamba
November 18, 2025 AT 04:11So we’re just supposed to trust the system now? Funny how autonomy is only real when it doesn’t interfere with profit margins. Big Pharma loves this talk-until you ask why the cheapest option isn’t always the first one offered.
Elia DOnald Maluleke
November 18, 2025 AT 18:35The architecture of medical authority has not been dismantled-it has merely been repackaged. Autonomy, as currently framed, is a performative gesture wrapped in the velvet of informed consent. True agency requires dismantling the economic scaffolding that turns bodies into actuarial tables.
Kathryn Ware
November 20, 2025 AT 04:54I’ve been using the Mayo Clinic decision aids for my mom’s diabetes meds-game changer. She’s 72, hates apps, but the printed chart with smiley/frowny faces for side effects? She actually understood it. We went from her just nodding to saying, ‘No, I don’t want that one, it makes me dizzy.’ And guess what? The pharmacist didn’t blink. She just pulled up the alternative. That’s what real care looks like. No jargon, no rush, just human stuff.
Joseph Townsend
November 21, 2025 AT 23:56Oh wow, another feel-good article about ‘patient empowerment’ while the system is still rigged. I’ve had doctors laugh when I asked about generics. I’ve had pharmacies tell me ‘the insurance won’t cover it’-then later find out the drug costs $12 at Walmart. This isn’t autonomy. It’s a magic trick where the patient is the rabbit and the bill is the hat.
kora ortiz
November 22, 2025 AT 09:09You got this. Asking questions isn’t being difficult-it’s being smart. Every time you say ‘What else?’ you’re rewriting the script. Keep pushing. Your body, your rules.
Leslie Douglas-Churchwell
November 23, 2025 AT 23:23Let’s be real-this ‘autonomy’ push is just Phase 2 of the pharmaceutical surveillance state. They want you to ‘choose’ so they can track your choices, feed them to AI, and then price-discriminate based on your ‘preferences.’ You think you’re in control? You’re just another data point in a predictive model designed to maximize shareholder value. They even have emojis now. 🤖💊
Deb McLachlin
November 24, 2025 AT 16:48The data supporting shared decision-making is robust, but implementation remains inconsistent. A 2023 JAMA study found that even in institutions with formal decision aids, clinician bias-particularly toward older and non-English-speaking patients-still results in significantly fewer options being presented. Structural change requires more than tools; it demands accountability mechanisms and mandatory training audits.
satya pradeep
November 25, 2025 AT 08:38Real talk: in India, most people don’t even get to ask. Doctors hand you a script like it’s a temple offering. I had to beg my doc to explain why my dad got the expensive insulin instead of the biosimilar. He said ‘it’s better.’ I asked ‘better for whom?’ He shut up. So I went to the pharmacy, showed them the price difference, and they told me the biosimilar is identical. We switched. Saved 70%. If you’re reading this and you’re in a country where doctors act like gods-ask anyway. Even if they get mad. You’re not being rude. You’re being alive.
Eric Healy
November 26, 2025 AT 14:28why do people think doctors are the enemy? theyre overworked and underpaid. the system is broken not the people. also if you dont take your meds youll end up in the er and then tax payers pay for it. just saying
Jeremy Hernandez
November 28, 2025 AT 01:45lol so now we’re supposed to believe the system wants us to have power? bro the same people who wrote this article probably got a bonus for pushing ‘patient-centered care’ while their hospital raised prices 20% last year. autonomy? nah. it’s just a marketing campaign with a fancy flowchart.
Kiran Mandavkar
November 30, 2025 AT 00:01Autonomy is a bourgeois fantasy. When your body is a site of capitalist extraction, your ‘choice’ is a cage lined with co-payments and formularies. The only real autonomy is refusing to participate in a system that commodifies pain. But you won’t do that, will you? You’ll just click ‘I consent’ and take the pill.
Kelsey Robertson
November 30, 2025 AT 14:21...and yet, no one ever mentions that 78% of patients who ‘choose’ their meds still end up discontinuing them within 6 months. So what’s the point? Are we just pretending to empower people so we don’t have to fix the real problem: that medicine is still a blunt instrument applied to complex biological systems? This isn’t autonomy-it’s therapeutic theater.
shubham seth
December 2, 2025 AT 07:48Let me break this down like a drug rep at a dinner party: they want you to feel like you’re choosing so you won’t notice you’re being upsold. That ‘decision aid’? Made by a company that sells the drugs on it. The pharmacist who ‘flags’ the biosimilar? Gets a kickback from the manufacturer. Autonomy is just the new placebo. And the real drug? Profit.
Tarryne Rolle
December 2, 2025 AT 16:21And what about the people who don’t want to be ‘involved’? Who just want the doctor to tell them what to do? Are they less human? Less worthy? This obsession with ‘choice’ feels like another way to blame patients for a system that fails them. Maybe some people just want to be told what to take-not be forced into a 45-minute philosophical debate about their life choices.