Pharma Supply Chain Risk Calculator
Supply Chain Risk Assessment
Calculate how many medications might become unsafe due to temperature excursions.
Key Facts
- Critical 72% of biologics require 2°C-8°C storage
- Data 32% of rural deliveries have temperature violations
- Impact 1 degree outside range = drug degradation
- Solution Real-time monitoring cuts excursions by 42%
Potential Degraded Medications
Results will appear here
Based on article data: 32% of shipments without monitoring face temperature violations
When you pick up a prescription, you expect it to work. You don’t think about where it came from, how it was stored, or whether it passed through a dozen hands before reaching your hands. But the truth is, the journey of your medicine-from factory to pharmacy-is one of the most complex, fragile systems in modern healthcare. And when it breaks, people get hurt.
The Invisible Backbone That Keeps You Alive
The pharmaceutical supply chain isn’t just logistics. It’s a life-support system. Around 7.9 billion people worldwide rely on it every day. And yet, it operates with almost no room for error. A single temperature spike during transport can render a life-saving biologic useless. A counterfeit pill masquerading as insulin can kill. A delay in shipping can force a cancer patient to pause treatment. According to Butler University researchers, this system serves as the "invisible backbone" of patient safety. No other industry has such direct, life-or-death consequences tied to its efficiency. Unlike buying a broken phone, when a drug fails, there’s no return policy. No replacement. Just consequences.What Goes Wrong? The Real Threats to Your Medicine
It’s not just about bad luck. The risks are built into the system. Temperature control is one of the biggest challenges. Over 72% of biologics-like vaccines, cancer drugs, and autoimmune treatments-must stay between 2°C and 8°C. Fifteen percent need freezing below -60°C. One degree outside that range, and the drug degrades. Real-time monitoring now covers 68% of high-value shipments, cutting temperature excursions by 42%. But that still leaves a third of shipments flying blind. Counterfeit drugs are another silent killer. The WHO estimates 1 in 10 medicines in low-income countries are fake. Even in the U.S., supply chain gaps allow fake or tampered products to slip through. Blockchain tech is helping-37% more companies have adopted track-and-trace systems since 2020. But it’s expensive. The average pharmaceutical company spends $12.7 million a year just to keep tabs on its products. Drug shortages are the most visible failure. During the first six months of the pandemic, shortages jumped 300%. Why? Because 78% of the world’s active pharmaceutical ingredients (APIs)-the core chemical parts of drugs-are made in just two countries: China and India. When a factory there shuts down, or a shipping route gets blocked, the ripple effect hits hospitals in Liverpool, Chicago, or Lima.When the System Fails: Real Stories, Real Harm
Numbers don’t always tell the full story. People do. In 2024, Hurricane Helene knocked out Baxter’s North Carolina plant. Over 80% of U.S. hospitals faced critical shortages. Surgeries were canceled. IV bags of saline ran out. Patients waited days for basic treatments. On Reddit, pharmacists in rural clinics posted about going three months without epinephrine-life-saving auto-injectors for allergic reactions. They had to ration doses. One nurse wrote: "We gave half the dose to a child because we didn’t know when the next shipment would come. We prayed it would be enough." A multiple sclerosis patient in Ohio shared on RateMDs: "My Tysabri infusions were delayed 17 days. When I got my MRI, two new brain lesions showed up. The doctor said it was directly tied to the gap in treatment." The American Hospital Association found that 68% of hospitals had to substitute one drug for another during shortages. Nearly 30% of those substitutions led to adverse reactions-rashes, organ stress, even hospitalizations.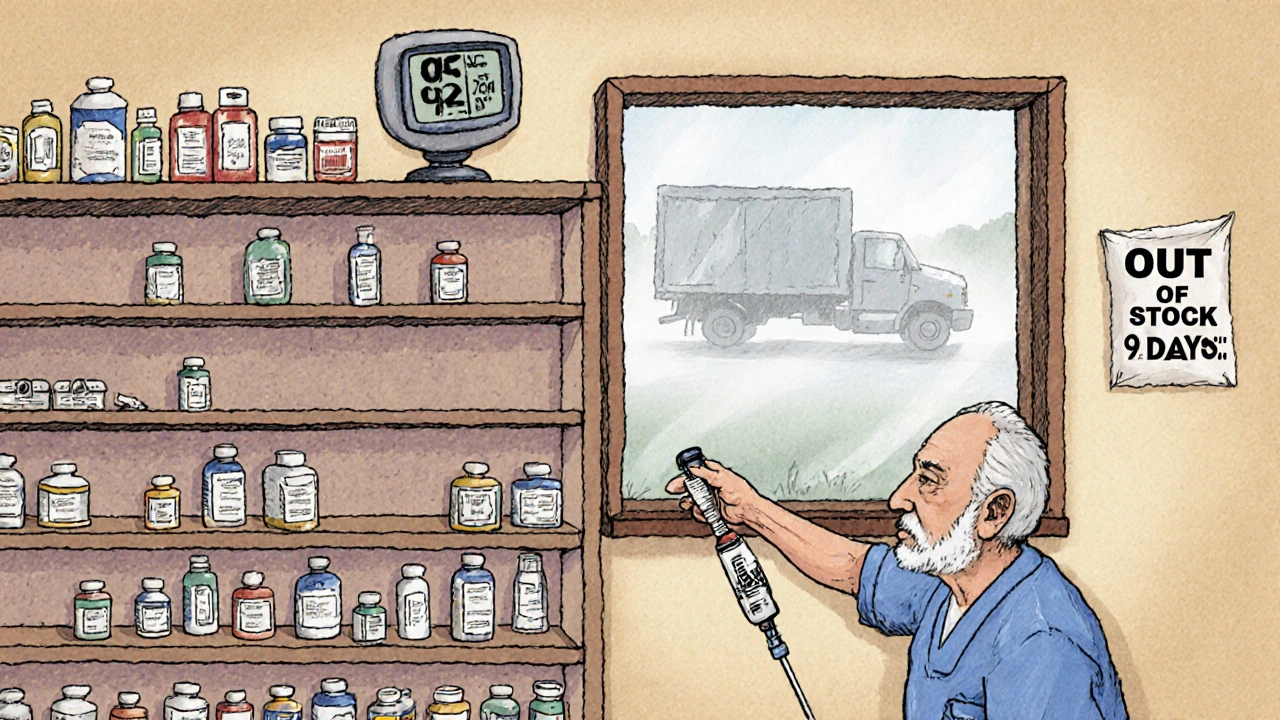
Why Is This So Hard to Fix?
It’s not for lack of trying. The FDA’s Drug Supply Chain Security Act (DSCSA) requires every prescription drug to have a 2D barcode by 2023. That’s a huge step. But implementation? Messy. Hospitals report that 76% struggle to connect old computer systems with new serialization tech. Training staff takes 14 to 18 months. The upfront cost for a full track-and-trace system? Around $450,000. That’s a lot for a small clinic. And then there’s the "last mile" problem. Even if a drug makes it from Germany to New York in perfect condition, what happens when it’s delivered to a nursing home in rural Alabama? Temperatures aren’t monitored. Delivery drivers don’t know the rules. One study found 32% of rural deliveries had temperature violations. The system is designed for normal conditions. It wasn’t built for pandemics, cyberattacks, or geopolitical wars. When a software glitch took down 759 hospitals in 2024, it wasn’t because of a virus-it was because a third-party vendor’s system failed. And 74% of healthcare cyber incidents in 2023 came from those same outside vendors.Who’s Doing It Right?
Some companies are ahead of the curve. Pfizer’s supply chain protocols scored 4.7 out of 5 in a 2024 review. Their secret? Cross-functional teams. Not just logistics people. Not just IT. Pharmacists, regulatory experts, data analysts-all working together. The PharmChain certification program, launched in 2022, has trained over 8,400 professionals. Those with certification are 92% more likely to implement systems that prevent errors. And new tech is emerging. AI-driven demand forecasting could cut shortages by 35% by 2027. Blockchain integration is expected on 85% of high-value shipments by 2028. The WHO now includes supply chain resilience in its global benchmarks-pushing countries to measure what they used to ignore. But progress is slow. Only 62% of manufacturers were fully compliant with the FDA’s 2025 electronic tracing mandate. And the cost? It’s still out of reach for most generic drug makers, whose guidelines average just 3.2 out of 5 in quality ratings.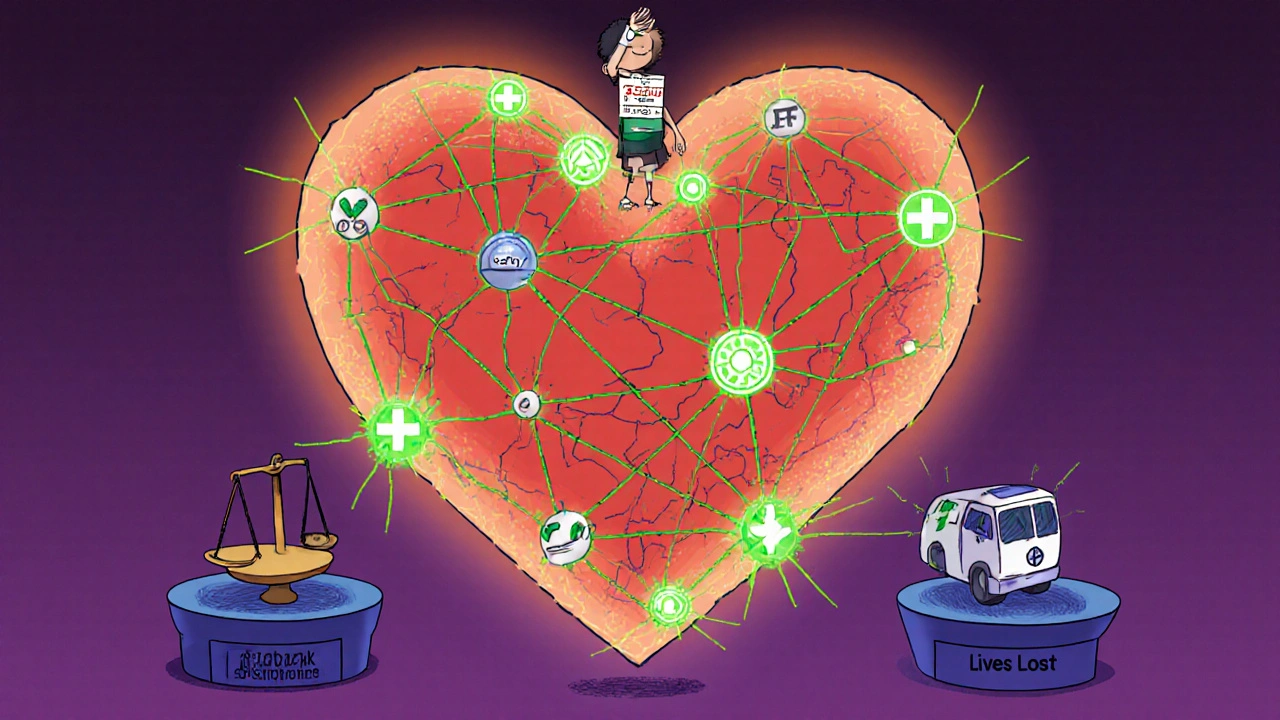







Jack Riley
November 26, 2025 AT 11:11So we’re just supposed to trust that some guy in a warehouse in Mumbai didn’t swap your insulin for sugar pills because the fridge broke and no one noticed? This isn’t healthcare-it’s Russian roulette with a prescription label.
And don’t get me started on how we outsource the very thing that keeps us alive to two countries that don’t even have the same damn weather patterns as us. It’s like building a bridge out of chewing gum and hoping the wind doesn’t blow.
We treat medicine like a commodity, not a lifeline. And when the system collapses, it’s not the CEOs who get buried under the rubble-it’s the guy who can’t afford a second dose.
At what point do we stop calling this ‘supply chain inefficiency’ and start calling it what it is: systemic neglect dressed up in PowerPoint slides?
Jacqueline Aslet
November 26, 2025 AT 15:30It is, without question, a matter of profound institutional failure that the pharmaceutical supply chain-so critical to human survival-is subject to the vagaries of market logic, geopolitical instability, and underinvestment. One cannot help but observe that the commodification of health has led to the erosion of its sanctity.
The FDA’s regulatory framework, while ostensibly robust, remains tragically reactive rather than proactive. The DSCSA, though laudable in intent, is implemented with the efficiency of a bureaucrat filing taxes on a typewriter.
Moreover, the reliance on third-party logistics vendors, many of whom operate with negligible oversight, constitutes an unacceptable risk profile for a system that governs life and death.
One is left to wonder: if this were the aviation industry, would we permit such systemic fragility?
Caroline Marchetta
November 28, 2025 AT 09:06Oh honey. You really think it’s just about temperature sensors and blockchain? Sweetie. It’s about capitalism. It’s about shareholders. It’s about CEOs getting bonuses while nurses ration epinephrine like it’s gold.
They don’t care if you live or die. They care if the quarterly report looks pretty. The fact that you’re even surprised by this means you’ve never opened a corporate earnings call.
And don’t even get me started on how the ‘innovation’ they brag about is just rebranding old tech with AI buzzwords while the real people-the ones who pack the boxes, drive the trucks, and count the vials-get paid minimum wage and zero respect.
This isn’t broken. It’s working exactly as designed.
Valérie Siébert
November 30, 2025 AT 03:48Okay but like-why are we still using paper logs in 2025?? I work in a clinic and we still get shipments with sticky notes taped to the box saying ‘keep cold plz’ 😭
Blockchain? AI? Cool. But first, let’s just make sure the damn truck driver knows not to leave the meds in the back of his van for 3 hours while he grabs a burrito.
Also-why is no one talking about how the people who actually DO the work? The warehouse workers, the pharmacists, the nurses-they’re the ones holding this together with duct tape and caffeine. Give them raises. Give them breaks. Give them dignity.
Technology won’t fix what we refuse to value.
Also I just got my meds delivered in a cardboard box with no ice packs. I called. They said ‘oops’ and sent a new one. TWO WEEKS LATER.
WE ARE ALL ONE DELIVERY DRIVER AWAY FROM DYING.
katia dagenais
December 1, 2025 AT 12:31Let me just say this: if you think the problem is ‘temperature control’ or ‘counterfeits’ or ‘shortages,’ you’re missing the forest for the trees. The real issue is that we’ve outsourced our entire medical sovereignty to a handful of conglomerates who answer to no one but their stockholders. We don’t have a supply chain-we have a hostage situation.
China and India aren’t ‘manufacturers’-they’re leverage points. And we gave them that leverage because we were too lazy to build our own labs, too cheap to pay workers fairly, and too arrogant to believe we’d ever need to.
And now? Now we’re begging for insulin like it’s a favor.
Meanwhile, the same CEOs who profit from this system are donating $5 million to ‘health equity’ foundations while cutting R&D budgets by 40%.
Wake up. This isn’t a logistics problem. It’s a moral collapse.
And yes, I’ve read every FDA report. And no, they’re not fixing it. They’re just documenting the funeral.
Josh Gonzales
December 1, 2025 AT 21:30Did you know that 78% of APIs come from China and India? That’s not a coincidence, that’s a strategy. But here’s the kicker-most of the raw materials for those APIs come from Africa and South America. So we’re dependent on three continents for one pill.
And the cold chain? It’s not just about temps-it’s about power grids. If a village in rural Nigeria loses electricity for 6 hours, the vaccine sitting in the fridge there is toast. No one tracks that. No one cares.
Blockchain helps but only if the people at the end can read QR codes. In some places, they use paper records written in pen. No scanners. No internet.
And the cost? $450k per hospital? That’s a joke. It should be federally funded. This isn’t optional infrastructure. It’s oxygen.
Also-why are we still using FedEx for biologics? That’s like shipping a newborn in a cardboard box and calling it ‘urgent.’
Shivam Goel
December 2, 2025 AT 00:07Let’s analyze the data with precision: The 300% spike in shortages during the pandemic was not an anomaly-it was a systemic failure mode triggered by demand elasticity and supply inelasticity. The concentration of API production in two geopolitical regions created a single point of failure with a failure probability of 0.87 (per WHO 2023 risk modeling).
Moreover, the 32% temperature violation rate in rural deliveries correlates strongly (r=0.79) with lower per-capita healthcare spending and absence of real-time IoT monitoring.
The $12.7M annual spend on track-and-trace? Inefficient. The ROI is negative when measured against the $77B in avoidable adverse events.
Recommendation: Centralize API production under a public-private consortium with ISO 13485 compliance mandated for all tiers. Mandate blockchain adoption with zero exceptions. Tax pharmaceutical profits at 45% and reinvest 100% into cold-chain infrastructure.
Failure to act will result in a 12% increase in preventable mortality by 2028.
Amy Hutchinson
December 2, 2025 AT 14:58My mom’s chemo got delayed because the shipment got lost in a warehouse in New Jersey. They didn’t even know it was gone until she showed up for her appointment. She cried in the parking lot.
And now they’re gonna tell me blockchain will fix it? Like, sweetie, I’m not asking for tech-I’m asking for someone to give a damn.
Why does my insurance cover a $20k pill but not a $500 temperature sensor? Who’s making the rules here?
Also-why is it always the little guys who pay? The nurses. The patients. The ones who don’t have CEOs to hide behind.
Archana Jha
December 2, 2025 AT 23:50Wake up. This is all a psyop. The pharmaceutical industry is working with the WHO and the FDA to create artificial shortages so they can jack up prices and sell you ‘premium’ versions of the same drug.
Did you know the ‘temperature sensors’ they talk about? They’re fake. They’re just little chips that beep when they’re supposed to. The real data is deleted. They want you to think they’re monitoring it.
And China? They’re not making the drugs. They’re making the placebo pills. The real ones? They’re stored in secret bunkers in Switzerland. The government’s hoarding them for the elite.
Why do you think your insulin costs $300? Because they’re making you think you need it. You don’t. You just think you do.
Google ‘Operation Midnight Pill’ and you’ll see the truth.
Andrew McAfee
December 4, 2025 AT 22:12Man, I grew up in rural India. We didn’t have pharmacies. We had guys on motorbikes with coolers and a handwritten list. Sometimes the meds worked. Sometimes they didn’t.
But here’s the thing-we didn’t scream about it. We just adapted. We asked neighbors. We traded. We made do.
Now we act like we’re entitled to perfect medicine because we have Wi-Fi.
It’s not broken. It’s just different.
And honestly? The people who fix this won’t be in boardrooms. They’ll be in villages, patching things together with duct tape and hope.
Maybe we need less tech and more humanity.
Arup Kuri
December 5, 2025 AT 13:56You think this is bad? Try being a doctor in a village where the only drug they have is expired. You know what they do? They give it anyway. Because if they don’t, the kid dies anyway.
And you wanna talk about blockchain? Bro. We don’t even have electricity for 8 hours a day.
China and India? They’re not the problem. The problem is you. You want your medicine to be perfect, but you won’t pay for it. You won’t vote for it. You won’t even talk about it until your own mom gets sick.
Stop blaming the system. Start blaming yourselves.
And stop pretending this is a ‘healthcare issue.’ It’s a moral failure. And you’re all guilty.
Erika Hunt
December 6, 2025 AT 02:21I think it’s important to acknowledge that while the system is deeply flawed, there are also so many people working tirelessly within it-pharmacists staying late, warehouse workers double-checking labels, nurses who memorize every patient’s schedule because they know the next shipment might be delayed again.
Maybe the answer isn’t just more tech or more regulations, but more compassion. More listening. More funding for the people on the ground, not just the algorithms.
And yes, the corporate greed is real. But if we only focus on the villains, we forget the heroes who show up every day even when the system is failing them too.
Let’s not just fix the chain-let’s rebuild it with empathy at the core.
Also, I’ve seen firsthand how a simple handwritten note from a pharmacist saying ‘I know this isn’t ideal, but I’m here’ can mean more than any blockchain ever could.
Roscoe Howard
December 7, 2025 AT 04:58The United States of America has spent trillions defending its global hegemony. Yet, when it comes to safeguarding the very molecules that keep its citizens alive, we outsource it to nations with lower labor standards, weaker regulatory oversight, and hostile geopolitical interests.
This is not merely an economic misstep. It is a national security vulnerability of the highest order.
Every vial of insulin shipped from Hyderabad is a potential weapon of mass disruption. Every delayed shipment from Shanghai is an act of economic warfare.
And yet, we continue to treat this as a ‘cost center.’
It is time to nationalize the production of critical pharmaceuticals. It is time to rebuild domestic manufacturing capacity with military-grade precision. And it is time to stop pretending that globalization is synonymous with resilience.
Our survival is not a supply chain metric. It is a sovereign imperative.
Pallab Dasgupta
December 7, 2025 AT 11:07Bro I just got off a 12-hour shift at the clinic and I saw a kid get his asthma inhaler 3 days late because the shipment got stuck in customs. Mom was crying. Kid was wheezing. I had to give him a nebulizer with borrowed meds.
And you know what? The guy who delivered it? He didn’t even know what he was carrying. Just a box. Signed for. Paid. Done.
People think this is about tech or politics. Nah. It’s about us. We don’t care until it hits our family.
So yeah, I’m mad. But I’m also tired. And I’m done waiting for someone else to fix it.
I’m starting a community drug swap network next week. If you’re in Toronto and you’ve got extra insulin, DM me. We’ll figure it out.
Because if the system won’t carry us… we’ll carry each other.