When you’re struggling with severe obesity, losing weight isn’t just about willpower-it’s about biology. Your body fights to hold onto fat, no matter how hard you diet or exercise. That’s where bariatric surgery comes in. Two procedures dominate the field: gastric bypass and sleeve gastrectomy. Both help people lose weight, but they work in very different ways. And choosing the right one isn’t just about which one loses more weight-it’s about your health, your lifestyle, and what you’re willing to live with long-term.
How These Surgeries Actually Work
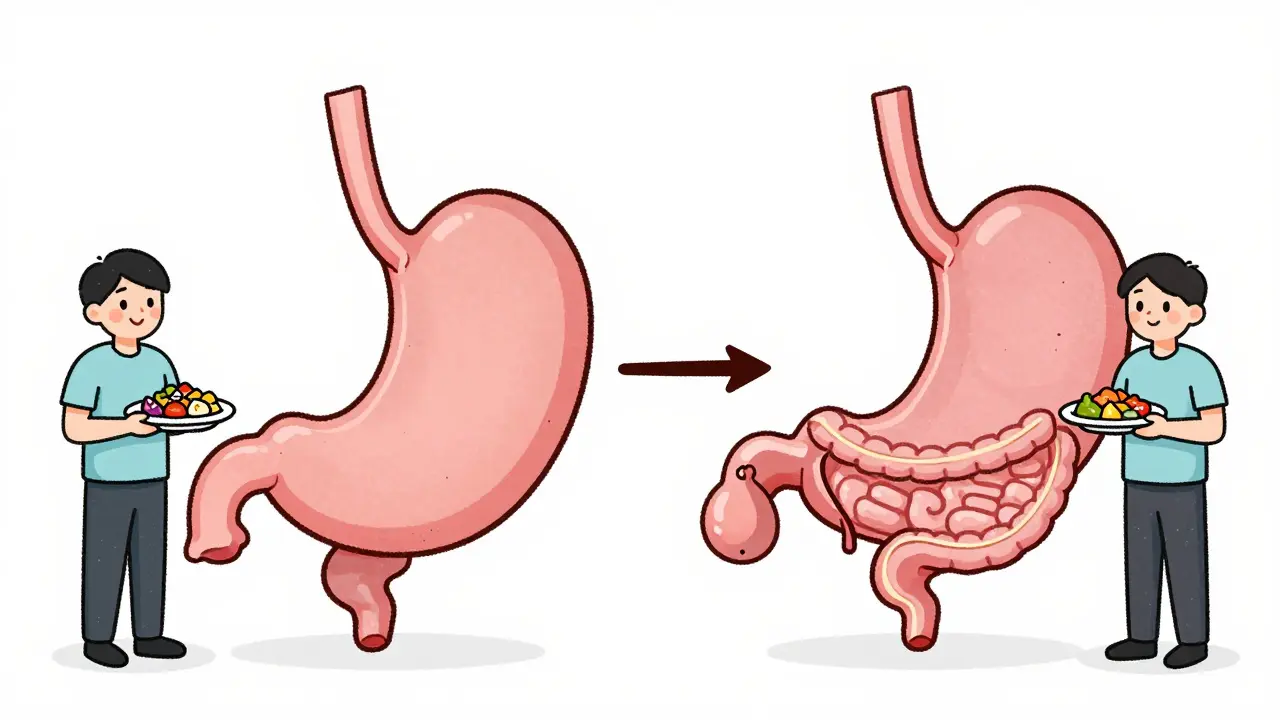
Gastric bypass, also called Roux-en-Y gastric bypass, changes how your body digests food. Surgeons make a tiny stomach pouch-about the size of a golf ball-and connect it directly to the middle part of your small intestine. This skips most of your stomach and the first section of your intestine. Food doesn’t go through the usual path. That means fewer calories get absorbed. It’s not just about eating less-it’s about your body absorbing less. Sleeve gastrectomy is simpler. About 80% of your stomach is removed, leaving a narrow tube, like a banana. This new stomach holds only 2 to 5 ounces. You feel full faster, and your body produces less of the hunger hormone ghrelin. No rerouting of the intestines. No bypassing. Just a smaller stomach. The surgery time reflects the difference. Sleeve gastrectomy takes about 47 minutes on average. Gastric bypass takes closer to 68 minutes. Both are done laparoscopically-small cuts, not one big incision. Most people go home the next day.Weight Loss: Which One Wins?
If your main goal is to lose the most weight, gastric bypass usually comes out ahead. Studies show that five years after surgery, gastric bypass patients lose about 57% of their excess weight. Sleeve gastrectomy patients lose around 49%. That’s a noticeable gap. UPMC data shows gastric bypass patients often lose 60-80% of excess weight within the first year to 18 months. Sleeve patients lose 60-70%, but it tends to be slower and steadier. For some people, that slower pace feels more manageable. For others, the faster drop with bypass is motivating. But weight loss isn’t the whole story. Some people lose weight quickly with sleeve, then hit a plateau. Others find they start regaining after three or four years. Gastric bypass tends to hold onto results longer. That’s why some doctors still recommend it for patients who need the most dramatic, lasting change.Health Improvements: Diabetes, Blood Pressure, and More
Both surgeries improve or even reverse obesity-related conditions. Type 2 diabetes, high blood pressure, sleep apnea, and joint pain often get better-or disappear-after either procedure. But gastric bypass has an edge when it comes to metabolic health. The malabsorptive part of bypass changes gut hormones in ways that improve insulin sensitivity. Studies show better diabetes resolution rates with bypass compared to sleeve. One 2024 JAMA Network Open study found hypertension improved more often in the bypass group. If you have type 2 diabetes, especially if it’s hard to control with medication, bypass might give you a better shot at remission. Sleeve gastrectomy still helps a lot. Many patients stop taking diabetes meds within months. But if you’re hoping for the strongest possible metabolic reset, bypass has more science behind it.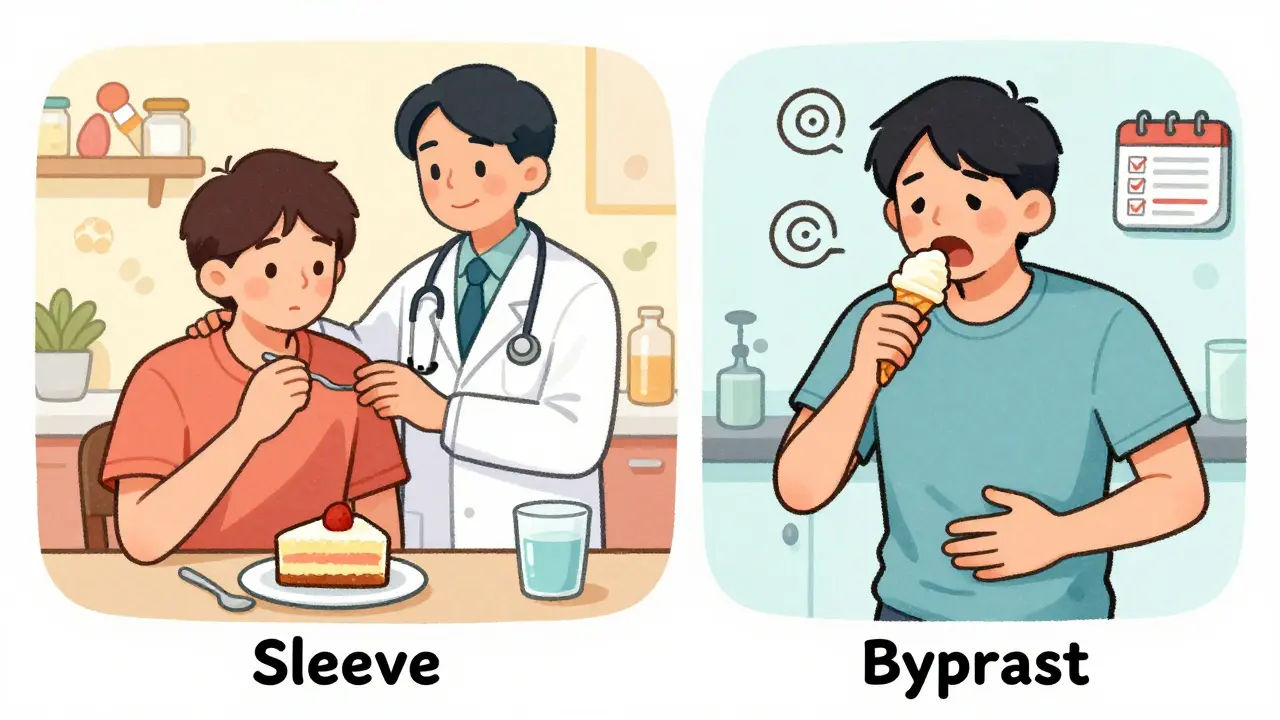
Risks and Complications: What Could Go Wrong?
No surgery is risk-free. But the risks are different for each. Gastric bypass has a higher chance of serious complications. A 2022 study of over 95,000 Medicare patients found the 5-year mortality rate was 5.67% for bypass versus 4.27% for sleeve. That’s a 32.8% lower risk of death with sleeve. Bypass patients are more likely to develop vitamin and mineral deficiencies. Because food skips parts of the intestine, your body can’t absorb enough B12, iron, calcium, or folate. Lifelong supplements are mandatory. Blood tests every six months are standard. Sleeve patients have fewer nutrient issues, but they face other problems. About 1 in 10 sleeve patients develop worsening acid reflux or GERD. And while bypass patients get dumping syndrome (nausea, sweating, dizziness after eating sugar), sleeve patients rarely do. Here’s the twist: sleeve patients are more likely to need a second surgery. The same 2022 study found 3.2 percentage points more sleeve patients needed revision surgery within five years. Why? Weight regain. The stomach can stretch over time. Some patients start eating more, and the sleeve doesn’t hold up.Recovery and Daily Life
Recovery time is similar-two to four weeks off work for both. But daily life after surgery is where things diverge. Gastric bypass patients must avoid sugar and high-fat foods. Eating them triggers dumping syndrome. That means no soda, no candy, no ice cream. Some people adapt. Others find it frustrating. The dietary rules are strict, and they never go away. Sleeve patients don’t get dumping syndrome, so they can eat sweets without consequences. But they still have to eat slowly, chew well, and stop when full. The smaller stomach makes that easier. Many say the recovery feels less restrictive. On Reddit’s r/bariatrics, people who had sleeve often say: “I can eat normal food again.” Those who had bypass say: “I lost more weight, but I have to be careful every single day.”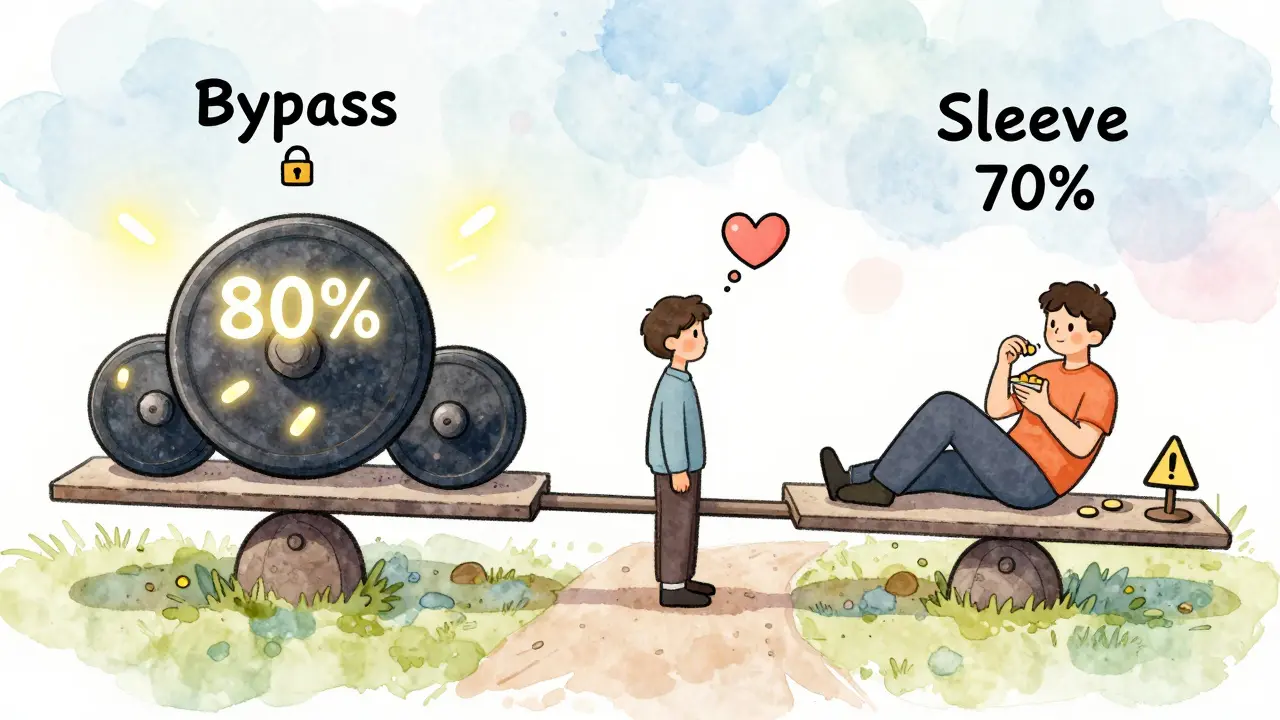
Cost and Insurance
Cost matters. Sleeve gastrectomy is typically 25% cheaper than gastric bypass. In 2024, the average out-of-pocket cost was $14,500 for sleeve and $19,300 for bypass-assuming insurance covers 80%. Most insurers follow NIH guidelines: BMI of 40 or higher, or BMI of 35 with a related condition like diabetes or high blood pressure. But some insurers, like UnitedHealthcare, now require a BMI of 45 or higher as of January 2024. You’ll also need six months of documented weight loss attempts, a psychological evaluation, and medical clearance-same for both procedures.Which One Should You Choose?
There’s no one-size-fits-all answer. But here’s how to think about it:- Choose gastric bypass if: You have type 2 diabetes you want to reverse, you need the most weight loss possible, you’re willing to take lifelong supplements, and you can commit to strict dietary rules.
- Choose sleeve gastrectomy if: You want a simpler surgery with fewer nutrient risks, you’re okay with a slightly slower weight loss, you’re worried about long-term complications, and you want fewer dietary restrictions.
The Bigger Picture
Sleeve gastrectomy is now the most common bariatric surgery in the U.S., making up over 60% of procedures. Gastric bypass has dropped to about 30%. Why? It’s simpler, safer in the short term, and patients like the idea of not having to worry about malabsorption. But the long-term data tells a different story. Gastric bypass holds up better over time. More weight stays off. More diabetes stays in remission. The trade-off is higher risk and more responsibility. New research is looking at hybrid procedures-like a mini-bypass combined with a sleeve-to get the best of both. But those are still experimental. Right now, the choice comes down to this: Do you want the biggest possible result, even if it comes with more rules and risks? Or do you want a safer, simpler path-even if it might not be as powerful? Both surgeries change lives. But only you can decide which change is right for you.Which surgery leads to more weight loss: gastric bypass or sleeve gastrectomy?
Gastric bypass typically leads to more weight loss. On average, patients lose 57% of their excess weight five years after bypass surgery, compared to about 49% with sleeve gastrectomy. Gastric bypass also tends to produce faster initial results, with many patients losing 60-80% of excess weight within 18 months. Sleeve patients lose 60-70% over the same period, but often at a steadier pace.
Is gastric bypass safer than sleeve gastrectomy?
No, gastric bypass carries higher risks. A 2022 study of over 95,000 patients found the 5-year mortality rate was 5.67% for bypass versus 4.27% for sleeve-a 32.8% lower risk with sleeve. Bypass also has a higher chance of complications like vitamin deficiencies, internal hernias, and bowel obstructions. Sleeve gastrectomy is technically simpler and has fewer immediate risks, but it has a higher rate of long-term revision surgeries due to weight regain.
Do I need to take vitamins forever after bariatric surgery?
Yes, but the need is greater after gastric bypass. Because bypass reroutes digestion, your body absorbs fewer nutrients. Lifelong supplements for B12, iron, calcium, and folate are required. Blood tests every six months are standard. Sleeve gastrectomy patients still need supplements, but usually only once a year for monitoring. Deficiencies are far less common with sleeve.
Can I eat sugar after bariatric surgery?
After sleeve gastrectomy, you can eat sugar without major side effects. After gastric bypass, eating sugar or fatty foods can trigger dumping syndrome-nausea, sweating, dizziness, and diarrhea. This happens in 50-70% of bypass patients. Most surgeons recommend avoiding sugary foods and drinks for life to prevent this. Sleeve patients don’t have this restriction, which many find easier to live with.
Which surgery has a higher chance of needing a second operation?
Sleeve gastrectomy has a higher revision rate. Studies show 3.2 percentage points more sleeve patients need follow-up surgery within five years, mostly due to weight regain or worsening reflux. The stomach can stretch over time, reducing the procedure’s effectiveness. Gastric bypass patients are less likely to need revision, as the anatomical changes are more permanent.
How much does bariatric surgery cost out of pocket?
As of 2024, the average out-of-pocket cost for sleeve gastrectomy is about $14,500, and for gastric bypass, it’s around $19,300-assuming insurance covers 80% of the total cost. Sleeve is typically 25% cheaper because it’s a simpler, shorter procedure. Costs vary by region and hospital, but the price gap is consistent across most U.S. providers.
Do both surgeries help with type 2 diabetes?
Yes, both surgeries significantly improve or even resolve type 2 diabetes. But gastric bypass is more effective at achieving full remission. The malabsorptive component changes gut hormones that regulate blood sugar, leading to better insulin sensitivity. Studies show higher diabetes resolution rates with bypass compared to sleeve, especially in patients with longer-standing or more severe diabetes.
Can I get pregnant after bariatric surgery?
Yes, many women get pregnant after bariatric surgery, and pregnancy is often safer after weight loss. But doctors recommend waiting 12 to 18 months after surgery to allow your body to stabilize and your nutrient levels to adjust. This is especially important after gastric bypass, where nutrient absorption is reduced. Close monitoring by your OB-GYN and a dietitian is essential to ensure you and your baby get enough vitamins and protein.



Todd Nickel
January 1, 2026 AT 08:40I’ve been following the bariatric space for years, and what strikes me is how much of the data gets oversimplified. The 57% vs 49% weight loss numbers? They’re averages, not guarantees. Some people lose 80% on sleeve, others lose 30% on bypass. The real differentiator isn’t the surgery-it’s adherence to follow-up care, nutritional discipline, and psychological support. Most studies don’t control for those variables, yet we treat the numbers like gospel. Also, the ‘faster weight loss’ narrative is misleading. Rapid loss often leads to loose skin, muscle wasting, and rebound eating. Steady is sustainable. I’ve seen both. Sleeve patients who stick to protein goals and therapy often outperform bypass patients who think the surgery did all the work.
Austin Mac-Anabraba
January 2, 2026 AT 13:01Let’s cut through the marketing fluff. Sleeve is the lazy person’s surgery. It’s cheaper, easier, and lets you eat a Twinkie without consequences-so naturally, it’s the default. Bypass is the adult choice: it forces accountability. You don’t get to be a sugar addict anymore. You either adapt or you fail. And guess what? The people who fail after bypass? They were the ones who didn’t want to change-they just wanted a magic button. The 32.8% lower mortality with sleeve? That’s because the surgery is less invasive, not because it’s better. The body doesn’t evolve with a sleeve. It just shrinks. With bypass, your entire metabolic pathway rewires. That’s not luck. That’s science. Stop romanticizing the easy path.
Phoebe McKenzie
January 2, 2026 AT 13:41THIS IS WHY AMERICA IS DYING. People think they can just cut their stomach and keep eating pizza like nothing happened. Sleeve is a trap. It’s a scam sold by greedy hospitals and insurance companies who don’t care if you end up back at 400 pounds in five years. And don’t even get me started on the vitamin thing-do you know how many people just stop taking them? They think they’re ‘fixed.’ They’re not. They’re ticking time bombs. I’ve seen women who had sleeve, got pregnant, and their babies were born with deformities because they didn’t take B12. It’s not a choice-it’s a moral failure. If you’re not willing to take lifelong supplements and never eat sugar again, you shouldn’t get the surgery at all. You’re not sick-you’re selfish.
gerard najera
January 2, 2026 AT 22:30Bypass for diabetes. Sleeve for simplicity.
Stephen Gikuma
January 4, 2026 AT 03:51Who’s really behind this? Big Pharma. They make billions off diabetes meds, and if you reverse it with bypass, they lose customers. That’s why sleeve is pushed-it’s profitable for hospitals but keeps you on meds. Also, the FDA approves these procedures too fast. They don’t track you for 10 years. They care about the 18-month results. And the insurance companies? They only care about the upfront cost. Sleeve is cheaper, so they push it. But they don’t pay for the revision surgeries, the ER visits, or the kidney failure later. The system is rigged. Don’t trust the ‘studies.’ They’re paid for.
Bobby Collins
January 4, 2026 AT 19:03ok but like… i had sleeve and i still crave donuts every day?? like i dont get sick but i just feel guilty?? is that normal?? 😅
Layla Anna
January 5, 2026 AT 00:11My cousin had bypass and she’s been diabetes-free for 7 years now 🥹 I cried when she told me she stopped her meds. But she also takes 12 pills a day and never goes out for ice cream… I don’t know if I could do that. Sleeve feels more like ‘me’ but I’m scared I’ll gain it back. I just want to feel normal again, you know? Not like I’m always fighting my body.
Heather Josey
January 5, 2026 AT 18:59It’s important to recognize that both procedures are life-altering and require lifelong commitment. The decision should be made in close collaboration with a multidisciplinary team-including dietitians, psychologists, and surgeons-rather than based on online anecdotes or cost alone. The data supports bypass for metabolic resilience and sleeve for lower procedural risk. Neither is ‘better’ universally. The right choice is the one aligned with your health goals, psychological readiness, and ability to adhere to follow-up protocols. This isn’t a quick fix. It’s a lifelong partnership with your health.
Olukayode Oguntulu
January 7, 2026 AT 16:43One must interrogate the epistemological foundations of the ‘weight loss’ paradigm itself. Is the body merely a vessel to be sculpted? Or is obesity a systemic dysregulation of metabolic signaling, sociopolitical alienation, and neurochemical reward architecture? The surgical reduction of gastric volume is a technocratic illusion-a reductive intervention that ignores the ontological weight of trauma, food insecurity, and capitalist commodification of appetite. Sleeve gastrectomy, in its neoliberal simplicity, mirrors the ideology of individual responsibility: shrink the stomach, not the system. Bypass, with its malabsorptive violence, is the medical-industrial complex’s ultimate expression: we will reroute your biology to fit the norm. Neither liberates. Both commodify. The real question: who benefits when we turn human suffering into a surgical product?