How to compare medicines for better health decisions
When working with compare, the act of weighing two or more medicines against each other to see which one fits a specific condition best. Also known as comparison, it guides patients and clinicians toward smarter choices.
One of the core medication, any drug prescribed or bought to treat an illness is its efficacy, how well it reduces symptoms or cures a disease. A drug with high efficacy but severe side effects, unwanted reactions that can range from mild nausea to serious organ damage might lose out in a head‑to‑head compare because safety matters just as much as results. Cost, dosage convenience, and drug‑drug interactions also join the equation, forming a multi‑dimensional matrix that any thorough comparison needs.
Why medication comparisons matter
Comparison involves evaluating efficacy, safety, and cost—all three are linked. Comparison influences treatment selection, improves patient adherence, and can lower overall healthcare spending. When you compare, you create a clear picture of which drug offers the best balance for your unique health profile, you empower yourself to ask better questions at the doctor’s office.
Take heart medications as an example. Lanoxin (digoxin) sits alongside beta‑blockers, ACE inhibitors, and calcium‑channel blockers. Each class changes heart rhythm in its own way, carries distinct side‑effect profiles, and varies in dosing frequency. By comparing, you see that digoxin may suit patients with atrial fibrillation but could pose toxicity risks for those with kidney problems. That insight directs clinicians toward a safer, more effective plan.
Antidepressants illustrate another angle. Celexa (citalopram) is often measured against other SSRIs and newer agents like escitalopram. While they share similar mechanisms, differences in half‑life, weight‑gain potential, and drug interactions shift the balance. A clear comparison, that highlights these nuances, helps patients avoid unwanted side effects such as sexual dysfunction or insomnia. The result is a treatment that feels less like a guess and more like a tailored fit.
Antibiotics bring a third perspective. Himcolin versus other broad‑spectrum options forces a look at bacterial resistance patterns, dosing schedules, and cost. A thorough comparison, reveals that while Himcolin may be cheaper, it could be less effective against resistant strains, leading to treatment failure. Knowing this before you start therapy can prevent a whole cascade of extra doctor visits and hospital stays.
Beyond individual drugs, comparing treatment pathways—like motion‑sickness relief with Antivert versus dimenhydrinate—shows how speed of action, sedation level, and suitability for long trips influence the best choice. Each article in this collection follows the same blueprint: list the key players, rank them on efficacy, safety, and cost, then offer actionable tips for real‑world use.
Below you’ll find a curated set of comparison guides covering heart meds, antidepressants, antibiotics, motion‑sickness solutions, and more. Whether you’re a patient looking for the right pill or a caregiver hunting the safest option, these pieces break down the science into plain language and give you the tools to make an informed decision. Dive in and see how a solid compare can change the outcome of your health journey.
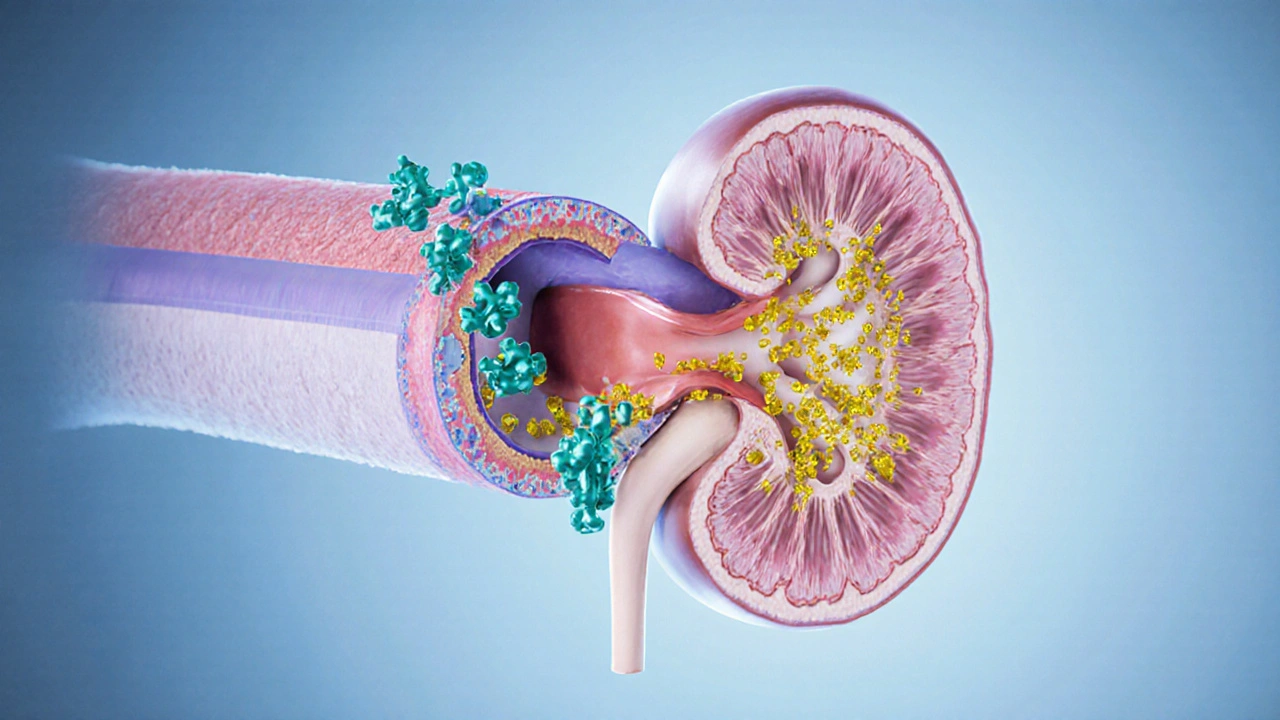
Benemid (Probenecid) vs Other Uric Acid Medications - Comparison Guide
A detailed comparison of Benemid (Probenecid) with gout alternatives, covering mechanism, safety, dosing, and when each drug fits best.





