Hepatitis B to Liver Cancer Risk Calculator
Risk Assessment Factors
Select the factors that apply to your situation to estimate your risk of developing hepatocellular carcinoma (HCC).
Your Estimated Risk Level
Why this matters
Every year millions of people discover they have chronic hepatitis B and wonder what it means for their future. The biggest fear? Liver cancer, specifically hepatocellular carcinoma (HCC). This article breaks down the biology, the numbers, and the steps you can take to lower your risk.
Understanding chronic hepatitis B
Chronic hepatitis B is a long‑lasting infection caused by the hepatitis B virus (HBV). The virus attacks liver cells and can remain in the body for decades. In Australia, the World Health Organization estimates that about 1.5% of adults are chronically infected.
The disease has three phases: immune‑tolerant, immune‑active, and inactive carrier. Blood tests like HBV DNA level, alanine aminotransferase (ALT), and hepatitis B e‑antigen (HBeAg) help doctors decide which phase a patient is in.
How HBV turns into liver cancer
The link isn’t magic; it’s a cascade of damage.
- Viral integration: HBV DNA can insert itself into the host genome, disrupting normal cell controls.
- Chronic inflammation: The immune system’s constant attack on infected cells leads to scar tissue, or cirrhosis, which is a fertile ground for cancer.
- Genetic mutations: Over time, mutations accumulate in genes that regulate cell growth, such as TP53 and CTNNB1.
Studies from the Centers for Disease Control and Prevention show that people with chronic HBV have a 20‑fold higher chance of developing HCC compared with the general population.
Who is at greatest risk?
Not every chronic HBV carrier will get liver cancer, but certain factors raise the odds dramatically:
- High viral load (HBV DNA >200,000IU/mL)
- Male gender - men are about 2‑3 times more likely than women.
- Family history of HCC.
- Co‑infection with hepatitis C or HIV.
- Heavy alcohol use or non‑alcoholic fatty liver disease.
- Age - risk climbs after 40years.
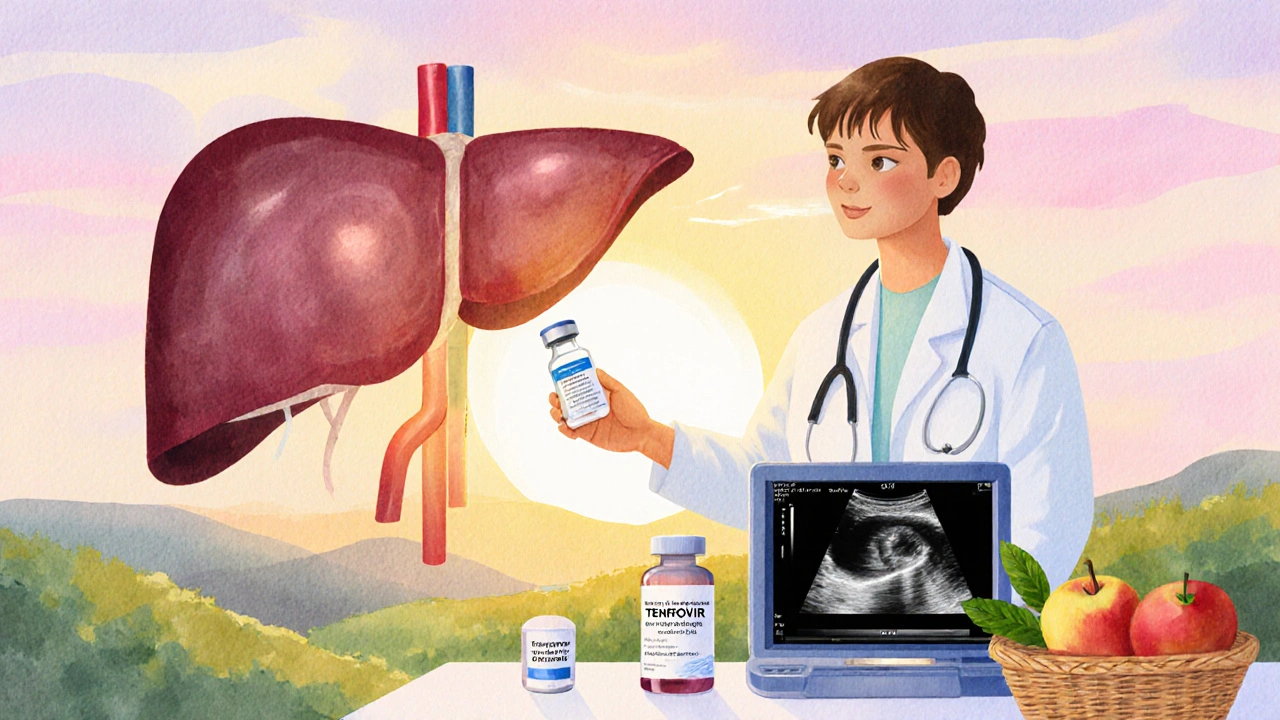
Screening - catching cancer early
Early detection saves lives. Guidelines from the American Association for the Study of Liver Diseases recommend that chronic HBV patients at elevated risk undergo:
- Ultrasound every six months.
- Serum alpha‑fetoprotein (AFP) testing alongside imaging.
- Optional magnetic resonance imaging (MRI) if ultrasound is inconclusive.
When a lesion is found, the typical next step is a biopsy or contrast‑enhanced imaging to confirm HCC.
Prevention through treatment
Antiviral therapy can shrink the risk gap.
| Treatment | Annual HCC Incidence (per 100,000) | Relative Risk Reduction |
|---|---|---|
| Tenofovir or Entecavir (first‑line) | 15 | ≈70% |
| No antiviral therapy | 55 | - |
| Interferon‑based regimens | 20 | ≈60% |
Both tenofovir and entecavir are high‑barrierto‑resistance nucleos(t)ide analogues. Starting treatment early-especially before cirrhosis develops-offers the greatest protection.
Vaccination and public health
The most effective way to curb the HBV‑HCC pipeline is prevention. Universal newborn vaccination, which Australia introduced in 1990, has cut chronic infections in children by over 80%.
Adults at risk (e.g., healthcare workers, people with multiple sex partners, or those traveling to high‑prevalence regions) should get a three‑dose series and a booster if antibody levels fall below 10mIU/mL.
Living with chronic hepatitis B
Beyond medicine, lifestyle choices matter:
- Limit alcohol to less than two drinks per day for men, one for women.
- Maintain a healthy weight; obesity fuels fatty liver disease.
- Stay up‑to‑date with regular liver ultrasound and blood work.
- Avoid smoking, which compounds cancer risk.
Support groups and counseling can help manage the emotional burden of a lifelong infection.
Key Takeaways
- Chronic HBV increases liver cancer risk up to 20times.
- High viral load, cirrhosis, male gender, and family history are major risk amplifiers.
- Six‑monthly ultrasound with AFP is the standard screening method.
- Effective antiviral drugs like tenofovir reduce HCC incidence by about 70%.
- Vaccination remains the cornerstone of long‑term prevention.
Frequently Asked Questions
Can chronic hepatitis B be cured?
Currently there is no definitive cure, but modern antiviral therapy can suppress the virus to undetectable levels, halt liver damage, and dramatically lower cancer risk.
How often should I get screened for liver cancer?
If you have cirrhosis or a high HBV DNA load, a six‑month ultrasound combined with AFP testing is recommended. People without these risk factors may be screened less frequently, based on doctor advice.
Does a healthy diet lower my HCC risk?
A balanced diet rich in fruits, vegetables, and lean protein supports liver health. Reducing sugary drinks and processed foods helps prevent fatty liver disease, which can compound HBV‑related cancer risk.
Is alcohol completely forbidden?
Alcohol isn’t strictly banned, but limiting intake is crucial. Even moderate drinking accelerates fibrosis in HBV‑infected livers.
Should my family members get tested?
Yes. HBV spreads through blood and body fluids, so household contacts should be screened and vaccinated if they’re not already immune.







Laurie Princiotto
October 6, 2025 AT 17:36Just another fancy calculator pretending to care about real lives 😒
Justin Atkins
October 7, 2025 AT 21:23The pathophysiology of HBV‑induced hepatocarcinogenesis is rooted in persistent viral replication, which perpetuates chronic inflammation and genomic instability. Moreover, quantitative PCR data consistently reveal a correlation between high viral titers and elevated oncogenic risk. Clinicians should therefore prioritize nucleos(t)ide analogue therapy to achieve undetectable loads. Finally, regular surveillance aligns with evidence‑based guidelines to catch neoplastic lesions before they metastasize.
June Wx
October 9, 2025 AT 01:10Honestly, this calculator feels like a gimmick that pretends to care about our health while spitting out numbers. It glosses over the lived reality of people battling hepatitis B for years. The risk factors are simplified to check‑boxes, ignoring the nuance of individual immune responses. I’ve seen friends suffer despite low viral loads, so this tool can’t capture everything. Still, if someone wants a quick glance, it might spark a conversation with a doctor. But don’t let a webpage replace professional guidance.
kristina b
October 10, 2025 AT 04:56The relationship between chronic hepatitis B infection and hepatocellular carcinoma is a tapestry woven from virology, immunology, and the inexorable march of time. From the moment the hepatitis B virus integrates into the hepatocyte genome, a latent threat is inscribed upon the liver's cellular script. This viral imprint can persist for decades, silently influencing cellular proliferation and apoptosis pathways. When the host’s immune system fails to eradicate infected cells, a chronic inflammatory milieu emerges, characterized by cytokine storms and oxidative stress. Such an environment foments DNA damage, gene methylation aberrations, and the activation of oncogenic signaling cascades. Moreover, high viral load amplifies these deleterious processes, acting as a relentless catalyst for malignant transformation. The presence of cirrhosis, often a sequel to long‑standing hepatitis B, further distorts the hepatic architecture, creating nodules of regenerative hyperplasia that are fertile ground for cancerous clones. Age compounds the risk, for the cumulative exposure to viral antigens and inflammatory insults accrues with each passing year. Alcohol consumption, while not a direct cause, synergizes with viral pathology to exacerbate oxidative injury and fibrotic progression. Familial predisposition may hint at shared genetic susceptibilities that modulate both viral clearance and tumor suppressor function. Consequently, a stratified risk assessment that incorporates gender, viral load, cirrhosis status, age, alcohol intake, and family history becomes indispensable for clinicians. Early detection through semi‑annual ultrasound and alpha‑fetoprotein measurement offers the best hope of intercepting malignancy at a curable stage. Prophylactic antiviral therapy, particularly with agents that achieve deep viral suppression, can dramatically diminish the oncogenic potential of hepatitis B. Yet, the most profound intervention remains public health education, vaccination, and the destigmatization of testing. In sum, understanding the multifactorial trajectory from chronic hepatitis B to liver cancer empowers both patients and providers to navigate a path toward prevention and early intervention.
Ida Sakina
October 11, 2025 AT 08:43It is incumbent upon us to recognize that chronic hepatitis B is not merely a laboratory value but a profound existential threat. The calculus of risk must be approached with reverence and precision. By integrating epidemiological data with individual metrics, we honor both science and humanity. Therefore, adherence to screening protocols is a moral imperative.
Amreesh Tyagi
October 12, 2025 AT 12:30i think this tool is overhyped i mean it gives numbers but life is messy
Brianna Valido
October 13, 2025 AT 16:16Love the idea of getting proactive about health 🌟 regular ultrasounds can really catch things early 😊 keep it up!
Caitlin Downing
October 14, 2025 AT 20:03Umm, i totally get u tho the calculator is kinda neat but dont forget to talk 2 ur doc bc it’s not a magic 8 ball.
Poorni Joth
October 15, 2025 AT 23:50Honestly the whole risk model is oversimplified and it doesnt take into account the myriad of genetic factorz that can influense outcomes.
Yareli Gonzalez
October 17, 2025 AT 03:36While tools like this can raise awareness, it’s essential to pair them with personalized medical advice to ensure the best outcomes for each individual.
Julia Odom
October 18, 2025 AT 07:23The integration of quantitative viral load assessment with demographic variables exemplifies a commendable stride toward precision medicine in hepatology.
Danielle Knox
October 19, 2025 AT 11:10Oh great, another calculator that thinks a few check‑boxes can replace a hepatologist’s expertise. 🙄