When someone is living with advanced cancer, the goal shifts from curing the disease to making every day as comfortable and meaningful as possible. This is where palliative care comes in-not as a last resort, but as a vital part of treatment from the moment a serious diagnosis is made. The focus isn’t on fighting the cancer alone; it’s on managing pain, reducing suffering, and helping people live as fully as they can, even when the odds are stacked against them.
Why Pain Control Isn’t Optional in Cancer Care
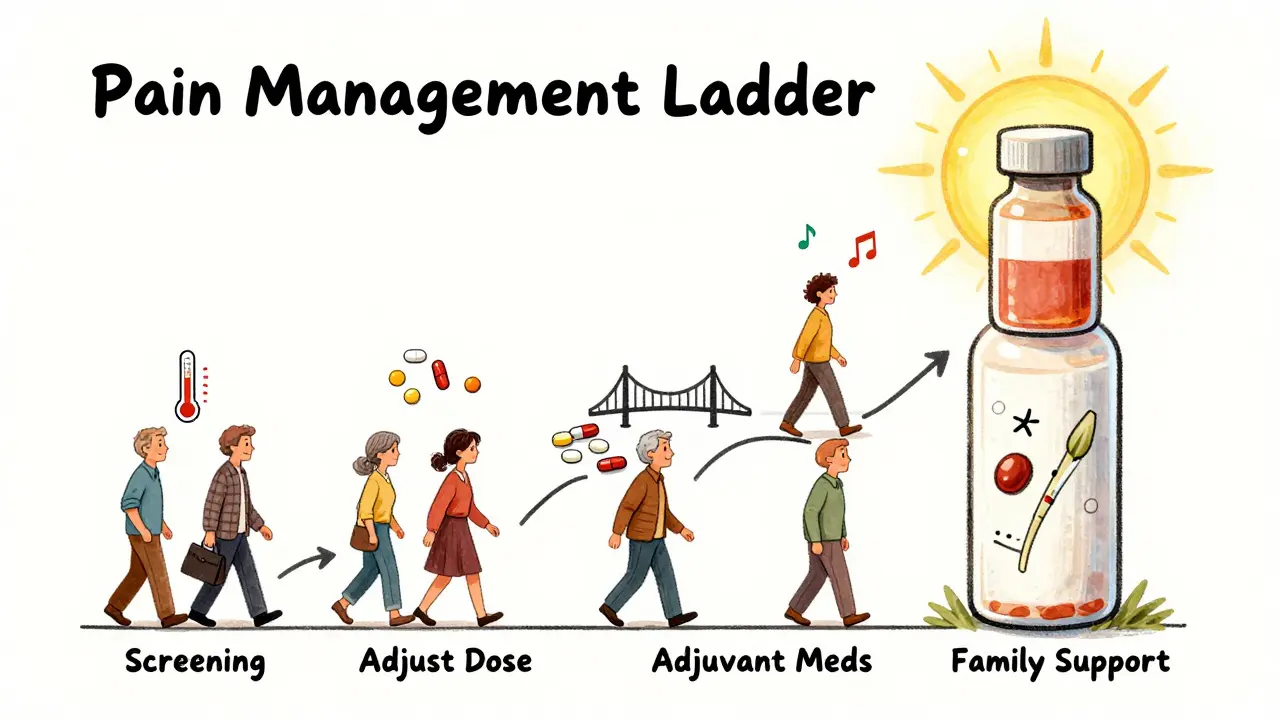
Up to 90% of people with advanced cancer will experience pain at some point. Yet, far too many still suffer needlessly. Why? Because pain is often under-treated-not because the tools don’t exist, but because of misunderstandings, fear, or systemic gaps in care. Pain in cancer isn’t just a symptom. It’s a medical emergency that needs immediate attention. The National Comprehensive Cancer Network (NCCN) requires that every cancer patient be screened for pain during their first visit and then regularly after that. No exceptions. Pain scores are measured on a simple 0 to 10 scale: 0 means no pain, 10 means the worst pain imaginable. If someone rates their pain at 7 or higher, action must be taken within an hour. This isn’t just about comfort. Uncontrolled pain leads to sleeplessness, depression, loss of appetite, and even faster disease progression. It traps people in a cycle of physical and emotional decline. The good news? Between 80% and 90% of cancer pain can be controlled effectively with current methods-if they’re used correctly.The Three-Step Pain Management Ladder
The foundation of cancer pain control has been around since 1986, when the World Health Organization (WHO) introduced its three-step analgesic ladder. It’s simple, proven, and still the global standard.- Step 1 (Mild pain): Start with non-opioid medications like acetaminophen (up to 4,000 mg per day) or NSAIDs like ibuprofen (400-800 mg three times daily). These work well for bone aches or mild inflammation.
- Step 2 (Moderate pain): Add a weak opioid like codeine (30-60 mg every 4 hours) on top of the non-opioid. This step is often skipped in practice, but it’s a critical bridge for many patients.
- Step 3 (Severe pain): Use strong opioids like morphine. The starting dose is typically 5-15 mg every 4 hours by mouth. Breakthrough pain-sudden spikes between scheduled doses-is managed with extra doses of 10-15% of the total daily amount.
When Opioids Aren’t Enough-or Too Much
Opioids are powerful, but they’re not the only tool. Sometimes, they don’t work well on their own. Or they cause too many side effects: constipation, drowsiness, nausea, or even confusion. That’s where adjuvant medications come in. These aren’t painkillers by default, but they’re highly effective for specific types of cancer pain:- Gabapentin or pregabalin for nerve pain (neuropathy) caused by tumors pressing on nerves or chemotherapy damage. Doses range from 100 to 1,200 mg three times a day.
- Duloxetine, an antidepressant, helps with both nerve pain and the depression that often comes with chronic illness. A daily dose of 30-60 mg can make a real difference.
- Dexamethasone, a steroid, reduces swelling around tumors-especially helpful for bone metastases. A daily dose of 4-16 mg can ease pressure and pain quickly.

Targeting Bone Pain and Metastases
Bone metastases are one of the most common and painful complications of cancer. When cancer spreads to the bones, it doesn’t just hurt-it can fracture, crush nerves, or cause spinal cord compression. The WHO and NCCN both recommend combining two approaches:- Bisphosphonates like zoledronic acid (4 mg IV every 3-4 weeks) slow bone breakdown and reduce pain.
- Radiotherapy delivers targeted radiation to the affected bone. A single 8 Gy dose often gives rapid relief. For more widespread pain, a course of 20-30 Gy over several sessions may be needed.
Quality of Life Isn’t Just About Pain
Palliative care isn’t a painkiller. It’s a whole-person approach. The ASCO and ESMO guidelines both stress that pain is just one part of the picture. Other factors matter just as much:- Emotional distress: A score of 4 or higher on the distress thermometer means the patient needs support from a counselor, social worker, or psychiatrist.
- Family support: Who’s helping at home? Are caregivers overwhelmed? Are cultural beliefs preventing honest conversations about pain or end-of-life wishes?
- Symptom burden: Nausea, fatigue, shortness of breath, loss of appetite-all these must be addressed too. Treating pain in isolation doesn’t work.
Barriers That Keep People Suffering
Despite all the guidelines, pain still goes untreated. Why?- Provider knowledge gaps: A 2017 study found 40% of oncology nurses weren’t certified in current pain management practices. Many still think opioids are dangerous for cancer patients, when the real danger is leaving pain uncontrolled.
- Patient fears: 65% of cancer patients worry about addiction. But addiction is rare in people with cancer who take opioids for pain. The bigger risk is withdrawal or undertreated pain.
- Cultural silence: In many Asian and Hispanic communities, stoicism is valued. Patients may hide their pain to avoid being a burden. That’s why screening tools must be culturally sensitive and repeated regularly.
- Insurance gaps: Non-drug therapies like physical therapy, acupuncture, or counseling are often not covered-despite evidence they help.
What’s New in Cancer Pain Management
The field is evolving. In 2023, the ESMO guidelines added specific advice for managing pain caused by newer cancer treatments like immunotherapy and targeted drugs-conditions like immune-related arthritis or nerve inflammation that weren’t common a decade ago. The CDC also updated its opioid guidelines in 2022 to include a clear exception for cancer pain. It now recognizes that the rules for chronic back pain don’t apply to someone with metastatic breast cancer. That’s a big deal. New tools are emerging too:- Smartphone apps that let patients log pain levels in real time. One 2021 study showed they improved documentation accuracy by 22%.
- Genetic testing for CYP450 enzymes, which tell doctors how fast a person metabolizes opioids. This helps avoid under- or overdosing.
- AI models that predict how a patient’s pain will change over time based on their tumor type, treatment, and history.
What You Can Do
If you or someone you love has cancer:- Ask for a pain assessment at every appointment. Don’t wait until it’s unbearable.
- Use the 0-10 scale honestly. Saying “it’s okay” when it’s an 8 only delays help.
- Ask if adjuvant meds or radiation could help-especially if bones are involved.
- Request a palliative care consultation early. You don’t have to wait until the end.
- Speak up about side effects. There’s almost always another option.
Is palliative care the same as hospice?
No. Hospice is for people who are no longer receiving curative treatment and are expected to live six months or less. Palliative care can start at diagnosis and continue alongside treatments like chemotherapy or surgery. It’s about improving quality of life at any stage of illness-not just at the end.
Will opioids make me addicted if I take them for cancer pain?
Addiction is rare in cancer patients using opioids for pain. Physical dependence-needing the drug to avoid withdrawal-is common, but that’s not the same as addiction. Addiction involves compulsive use despite harm, which is extremely uncommon when opioids are used as prescribed for cancer. The greater risk is undertreated pain, which harms your body and mind far more.
What if my doctor won’t prescribe enough pain medication?
Ask for a referral to a palliative care specialist or pain management clinic. Many hospitals have teams dedicated to cancer pain who work with oncologists to adjust treatment plans. You have a right to pain control. If your current provider is hesitant, seek a second opinion. The NCCN guidelines say all cancer centers must offer palliative care consultation-use that right.
Can non-drug therapies really help with cancer pain?
Yes. Acupuncture, massage, physical therapy, mindfulness, and even music therapy have been shown to reduce pain and anxiety in cancer patients. They work best when combined with medication-not instead of it. Many insurance plans don’t cover them, but hospitals often offer them for free as part of palliative care programs.
How do I know if my pain management plan is working?
Track your pain daily using the 0-10 scale. If your average pain stays above 3 after a week of treatment, the plan needs adjustment. Also ask yourself: Can I sleep? Eat? Talk with loved ones? Do simple things like shower or sit outside? If the answer is no, pain is still controlling your life-and it shouldn’t be.
Is palliative care only for older people?
No. Palliative care is for anyone with a serious illness, regardless of age. Young adults with metastatic cancer benefit just as much as older patients. In fact, younger people often face unique challenges-like caring for children or maintaining a career-and palliative care teams help with those too.


Lydia H.
January 18, 2026 AT 16:17Just wanted to say this post hit different. I’ve seen my aunt go through this, and the fact that pain is treated like an afterthought still breaks my heart. It’s not about being brave-it’s about being human. No one should have to suffer in silence just because someone’s afraid of opioids.
And honestly? The 0-10 scale is genius. Simple, measurable, and it gives patients back a voice. Why don’t we use this for every chronic illness?
Josh Kenna
January 20, 2026 AT 04:06im reading this at 3am because my dad’s on morphine and i just cried reading the part about breakthrough doses. they told us to wait 4 hours but he was screaming at hour 2 and we were too scared to give more. turns out we were right to push. the palliative team said we did the right thing. thank you for writing this.
also pls tell doctors to stop acting like giving pain meds is a crime. its 2024. we have science. use it.
Phil Hillson
January 20, 2026 AT 22:12okay but why is everyone acting like this is new info? i read this in med school in 2010. the WHO ladder? the adjuvants? the bone mets stuff? been standard for decades. why are we treating this like a revelation?
also why does every article about cancer care now sound like a TED Talk? just tell me what to do not how to feel about it
Lewis Yeaple
January 21, 2026 AT 21:50While the clinical guidelines referenced herein are indeed evidence-based and widely endorsed, one must not overlook the structural impediments to implementation. The disparity between guideline adherence and real-world practice remains profound, particularly in under-resourced settings where access to bisphosphonates, radiotherapy, or even basic opioids is restricted by bureaucratic inertia or supply-chain failure.
Furthermore, the assertion that addiction is rare in cancer patients requires qualification: while true in aggregate, individual pharmacokinetic variance, psychiatric comorbidity, and prior substance use disorder history necessitate individualized risk stratification. The CDC’s 2022 clarification is welcome, but insufficient without institutional policy reform.
sujit paul
January 23, 2026 AT 03:15Let me tell you something, my friend. In India, we have a saying: 'Pain is God's way of testing you.' And guess what? Millions of people suffer silently because they believe it's spiritual. They don't ask for morphine because they think it's 'sinful' to escape suffering. The doctors? They're scared to prescribe. The nurses? They don't know the doses. The system? Broken. This post is beautiful, but it's written for people who live in places where the system still works. For the rest of us? We pray the pain stops before the body does.
And yes, I know this sounds dramatic. But if you've seen a grandmother with bone metastases trying to walk to the toilet because no one gave her the right dose of gabapentin-you won't laugh at drama anymore.
Tracy Howard
January 24, 2026 AT 15:55Wow. Just wow. I'm Canadian and I have to say, this is exactly why I'm so proud of our healthcare system. In the U.S., you're lucky if your oncologist even knows what a bisphosphonate is. Here? We have palliative care teams on standby from day one. No waiting. No paperwork. No guilt. You want relief? You get it. No drama.
And yes, I'm saying this because I'm sick of Americans acting like their system is superior. It's not. We do pain management right. Period.
Astha Jain
January 26, 2026 AT 02:20so like… if u have cancer and ur pain is at 8 and ur doc says ‘try ibuprofen first’… u just… leave? no? u ask again? or do u just suffer? i had a friend who waited 3 weeks for a morphine script bc the doc was ‘worried about tolerance’ and she ended up in ER with a broken hip from a fall. this is not medicine. this is negligence.
Jake Rudin
January 27, 2026 AT 10:37It’s fascinating how we’ve reduced human suffering to a scale of 0 to 10… and yet, we still treat it like a math problem. Pain isn’t just a number-it’s the silence between breaths, the way a hand trembles reaching for water, the look in someone’s eyes when they think no one’s watching. The medications help, yes. But what heals is being held, being heard, being allowed to be afraid without being fixed.
The WHO ladder is brilliant. But the real cure? Is dignity. And dignity doesn’t come from a prescription.
…I hope someone reads this and remembers that.
Malikah Rajap
January 29, 2026 AT 04:30Can we talk about how the word 'palliative' sounds like 'palliative care' is a euphemism for 'give up'? Like, why can't we just say 'comfort care' or 'living well with illness'? The term itself makes people think it's the end… when it's actually the most active, intentional, and loving kind of care there is.
Also, why do we keep saying 'no one should suffer' like it's a moral imperative, but then insurance denies acupuncture because it's 'alternative'? Hypocrisy much?
Jackson Doughart
January 30, 2026 AT 18:16I’ve sat with patients who refused opioids because they didn’t want to be ‘a burden.’ One woman told me, ‘If I’m not in pain, they’ll think I’m getting better.’
We’ve taught people that pain is something to endure, not something to treat. That’s not strength. That’s trauma.
Thank you for writing this. Not because it’s new-but because someone still needs to hear it.
Jackson Doughart
February 1, 2026 AT 07:32Thank you for this. My sister’s oncologist told her palliative care was ‘for people who are dying.’ She cried for three days. We got her a referral the next week. She’s been on gabapentin and low-dose morphine for six months. She’s painting again. She takes walks with her dog. She’s not dying. She’s living.
Palliative care didn’t give up on her. She didn’t give up on herself.
And that’s the real miracle.