Cancer treatment is evolving rapidly, offering new hope to patients worldwide. Renal cell carcinoma (RCC), a primary type of kidney cancer, has particularly seen advancements with the introduction of cryoablation. In simple terms, cryoablation is a process where extreme cold is used to destroy cancer cells directly. By targeting the tumor with precise cold temperatures, abnormal cells freeze and eventually die off, sparing much of the surrounding healthy tissue.
Traditional treatments like surgery might not be suitable for everyone, especially those with advanced cancers or other health issues making surgery risky. Cryoablation offers a minimally invasive alternative with fewer complications and shorter recovery times. During the procedure, a needle-like probe is inserted through the skin into the kidney tumor under image guidance. Cold gases circulate through the probe to freeze the tumor tissue, aiming to destroy the cancer cells efficiently.
Patients who undergo cryoablation often experience good outcomes. Many report minimal pain, quicker return to normal activities, and limited side effects compared to conventional treatments. Success rates are even more promising when cryoablation is combined with other therapies, contributing to a comprehensive, multi-faceted approach to fighting RCC. It's interesting to note that this technology is continually evolving, with ongoing research focused on improving accuracy and outcomes even further.
- Understanding Renal Cell Carcinoma
- What is Cryoablation?
- Benefits of Cryoablation in Kidney Cancer
- Procedure and Recovery
- Patient Outcomes and Success Rates
- Future of Cryoablation in Oncology
Understanding Renal Cell Carcinoma
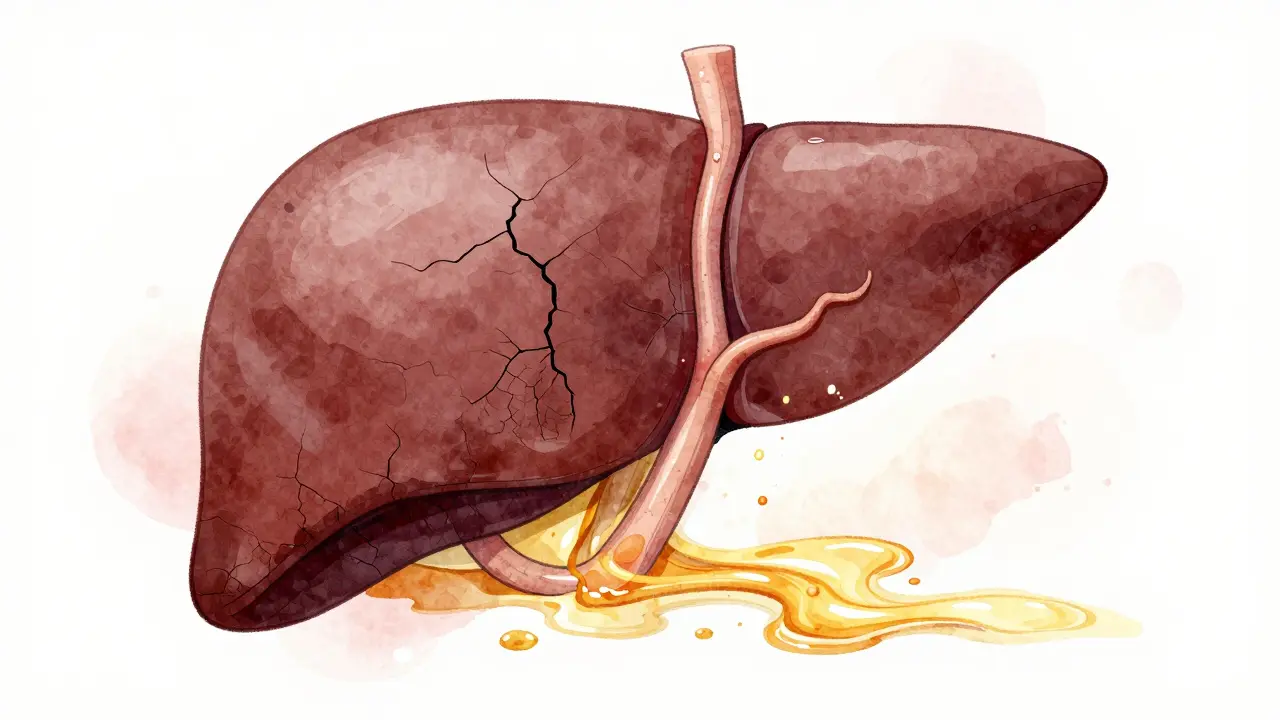
Renal cell carcinoma (RCC) is the most common type of kidney cancer in adults, accounting for about 85% of kidney cancer cases. This malignancy originates in the lining of the small tubes within the kidney. Unlike other cancers, RCC is unique due to its characteristic resistance to both radiation and chemotherapy, making it a formidable opponent in the field of oncology.
RCC often remains undiagnosed until it reaches an advanced stage, primarily because its early symptoms can be quite subtle or mistaken for less severe conditions. For instance, a patient might experience hematuria (blood in the urine), flank pain, or a palpable mass in the abdomen, but these signs often appear once the cancer has progressed. Such late detection underscores the importance of regular medical check-ups, especially for those in high-risk groups like smokers or individuals with a family history of kidney cancer.
Understanding the factors contributing to RCC is crucial. Lifestyle choices, such as smoking and obesity, significantly increase the risk. Additionally, high blood pressure and certain inherited conditions, like von Hippel-Lindau disease, are known risk enhancers. Environmental factors and occupational exposures to chemicals like trichloroethylene also play a role. It's crucial to recognize and address these risk factors to help with early detection and prevention.
According to the American Cancer Society, RCC is more common in men than in women, and the incidence is typically higher in older adults, with most cases being diagnosed between ages 50 and 70. The five-year survival rate for localized RCC is relatively favorable, around 93%, but this drops significantly if the cancer has metastasized, highlighting the importance of early detection and effective treatments.
Research into RCC is continually evolving. Newer therapies targeting specific genetic mutations and molecular pathways have shown promise in managing advanced cases. The advent of immunotherapies, for instance, has opened new avenues for treatment, helping to boost the immune system's ability to fight cancer. A notable expert in the field, Dr. James Brugarolas, once remarked, "The integration of targeted therapies with traditional methods marks a significant leap forward in RCC treatment."
Despite these advancements, many patients with RCC endure physical, emotional, and financial burdens. Support systems, including counseling, patient education, and social services, play a pivotal role in improving the quality of life. The journey through cancer treatment can be tough, but with a combination of medical innovations and strong support networks, patients can navigate through more smoothly.
What is Cryoablation?
Cryoablation is a groundbreaking technique increasingly used in treating various cancers, including renal cell carcinoma. At its core, cryoablation involves the use of extreme cold to freeze and destroy abnormal tissues or tumors. Unlike traditional surgical methods, which might require large incisions and longer recovery times, cryoablation is minimally invasive, offering significant benefits for patients.
During the procedure, a thin, needle-like probe called a cryoprobe is carefully inserted into the tumor. This is typically done under the guidance of imaging techniques such as ultrasound, CT scans, or MRI, ensuring precise placement. The cryoprobe then circulates extremely cold gases, typically argon or nitrogen, to rapidly freeze the target tissue. The cell-killing process occurs at very low temperatures, sometimes as cold as -40 degrees Celsius or lower. The freezing process causes ice crystals to form inside the cancer cells, rupturing them and leading to cell death.
An intriguing aspect of cryoablation is its ability to spare surrounding healthy tissues, which is crucial for kidney functions. This precision makes it a viable option for patients who may not be suitable candidates for traditional surgery due to age, health conditions, or the location of the tumor. It is also noteworthy that cryoablation can be repeated if necessary, making it a versatile tool in managing recurring cancers.
One fascinating fact about cryoablation is its historical roots. Cryosurgery has been around for decades, used initially for skin lesions and then adapted for internal organs. However, with advancements in imaging and cryotechnology, its application has broadened remarkably. Dr. S. Schwartz, a prominent oncologist, once commented, "Cryoablation represents a significant leap in oncological therapies, offering patients new possibilities when surgery isn't an option."
Clinical studies also highlight the effectiveness of cryoablation. For instance, survival rates for patients with small kidney tumors treated with cryoablation are reported to be comparable to those undergoing partial nephrectomy, a conventional surgical approach. These findings are encouraging and pave the way for more widespread use of cryoablation in renal cell carcinoma treatments.
In summary, cryoablation is a sophisticated, minimally invasive technique that employs cold temperatures to eliminate cancerous tissues. Its precision, coupled with fewer side effects and quicker recovery times, makes it particularly appealing for treating kidney cancer. As research and technology continue to progress, the role of cryoablation in modern oncology is set to grow, providing hope and effective solutions for patients battling this challenging disease.

Benefits of Cryoablation in Kidney Cancer
Cryoablation for kidney cancer, or renal cell carcinoma (RCC), offers a range of advantages that make it an appealing option for many patients. One of the primary benefits is its minimally invasive nature. Unlike traditional surgery that requires large incisions and longer recovery times, cryoablation involves only small punctures. These minimal entry points lead to significantly less post-procedure pain and a quicker return to regular activities.
The precision of this treatment is another major advantage. During cryoablation, a probe is guided to the tumor using imaging techniques like ultrasound or CT scans. This allows doctors to target the cancer cells accurately without affecting surrounding healthy tissues. Because of this precision, patients experience fewer side effects, making the treatment more tolerable for those with higher health risks or who are in poor general health.
Notably, studies show that cryoablation has a high success rate in treating smaller tumors, particularly those less than 4 centimeters. In many cases, cryoablation can be as effective as traditional surgery for small renal tumors. This option is crucial for elderly patients or those who might not be able to endure the physical stress of conventional surgical methods. As part of a comprehensive cancer treatment plan, cryoablation often results in favorable outcomes and has been associated with a lower rate of cancer recurrence.
Dr. Stephen C. Campbell, a leading urologic oncologist, once stated, "Cryoablation offers a safe and effective alternative for patients who may not be surgical candidates. Its targeted approach greatly reduces complications while delivering promising results."
Additionally, the recovery time for cryoablation is impressively short. Most patients can go home the same day or, at most, the day after the procedure. This rapid recovery is particularly beneficial for those who wish to return to their daily routines without the extended downtime associated with more invasive surgeries. The enhanced recovery also translates to less financial burden, as shorter hospital stays and quicker return to work can significantly reduce overall treatment costs.
Cryoablation also opens the door for retreatment if necessary. For instance, if a tumor recurs or if new ones develop, patients can undergo additional cryoablation sessions without the accumulated trauma that repeat surgeries would cause. This flexibility makes it a viable long-term management option for kidney cancer.
Moreover, ongoing research and technological advancements continue to improve the efficacy and safety of cryoablation. New techniques and better imaging tools are constantly being developed, aiming to enhance accuracy and expand the types of tumors that can be treated. This ongoing innovation ensures that cryoablation remains at the forefront of modern, patient-centered cancer care.
For those considering this advanced treatment, the key benefits include its minimally invasive nature, precision, shorter recovery time, high success rate for smaller tumors, and the ability to undergo multiple treatments if required. As more people become informed about these advantages, cryoablation is poised to become a widely accepted option in the fight against renal cell carcinoma.
Procedure and Recovery
The cryoablation procedure for treating renal cell carcinoma is both fascinating and cutting-edge. The process begins with the patient lying on an operating table where precise imaging techniques, typically CT or MRI scans, are used to visualize the kidney tumor. This ensures that the medical team can accurately guide the cryoablation probe to the right location. The patient is usually under local anesthesia, along with sedation to minimize discomfort during the procedure.
Once the imaging confirms the tumor's exact position, a thin, needle-like probe is inserted through the patient's skin and directed to the target area. This part of the process demands incredible accuracy and care from the medical professionals. When the probe is in place, a sequence of extremely cold gases like argon or liquid nitrogen is circulated through it. These gases create an ice ball around the probe's tip that freezes the tumor tissue. Temperatures can plummet to as low as -40 degrees Celsius, effectively killing the cancerous cells.
The freezing process usually takes several minutes, and it might be repeated multiple times in cycles to ensure maximum efficiency. Throughout this time, continuous imaging helps the doctors monitor the freezing process and the progress of the tissue destruction. Thanks to its precision, cryoablation significantly reduces the risk of damage to surrounding healthy tissues. After the freezing cycles are complete, the probe is carefully removed, and a small bandage is placed over the insertion site.
Recovery from a cryoablation procedure is typically swift, especially compared to traditional surgical options. Most patients can go home the same day or after a short hospital stay. The insertion site might be sore for a few days, and some patients could experience mild discomfort or bruising. Pain management is often straightforward, involving over-the-counter pain relievers.
Follow-up care is crucial and generally involves a series of imaging tests over the next several months to evaluate the procedure's success and ensure the tumor has not started to regrow. Regular check-ups with the healthcare provider allow for early detection of any potential issues, which can be addressed promptly. The minimally invasive nature of cryoablation often means a faster return to daily activities. Many patients can resume their normal routines within a week, a notable difference from the longer recovery periods associated with more invasive surgeries.
It's worth mentioning that the rates of complications for cryoablation are relatively low. Infections, bleeding, or damage to surrounding organs are possible but infrequent outcomes. According to data published by the American Cancer Society, the success rate of cryoablation in controlling small kidney tumors is above 90%, making it an appealing option for many.
"Cryoablation offers a unique balance of efficacy and reduced invasiveness, making it an ideal choice for patients who might not be suitable candidates for surgery," says Dr. Susan J. Mandel, a prominent oncologist.
Cryoablation is indeed a groundbreaking approach in the fight against renal cell carcinoma. It combines advanced technology with the human touch of skilled medical professionals to offer hope and improved quality of life to many patients battling kidney cancer.
Patient Outcomes and Success Rates
When dealing with advanced renal cell carcinoma (RCC), understanding patient outcomes and success rates with specific treatments like cryoablation is crucial. Patients often want to know how effective a treatment is and what they can expect in terms of recovery and long-term health. Studies have shown that cryoablation offers promising results, notably for those with small to moderately sized kidney tumors.
One of the key benefits seen in patient outcomes is the lower complication rate compared to traditional surgical options. Because cryoablation is minimally invasive, patients usually experience less pain and require shorter hospital stays. This lower invasiveness also translates to quicker recovery periods, enabling patients to resume their daily activities sooner. The ability to target and destroy the tumor cells without damaging surrounding healthy tissue helps in reducing the side effects and complications often associated with more aggressive treatments.
Statistically, success rates for cryoablation are encouraging. According to a study published by the American Urological Association, over 90% of patients treated with cryoablation for small kidney cancers showed no evidence of cancer recurrence at a median follow-up of three years. These numbers are particularly significant when considering that traditional treatments like partial or radical nephrectomy come with higher risks and longer recovery times.
It's also worth noting the overall survival rates post-cryoablation. In many cases, patients with RCC who undergo cryoablation have survival rates comparable to those who opt for more invasive surgical procedures. This makes it an attractive option, especially for patients who might have other underlying health issues that could complicate surgery.
To add a personal dimension to these statistics, consider this quote from Dr. Samuel Kader, a leading oncologist:
"Cryoablation has revolutionized how we approach advanced renal cell carcinoma. By focusing on preserving healthy tissue and minimizing recovery time, we not only treat the cancer effectively but also improve the patient's overall quality of life."Such endorsements highlight the growing confidence in cryoablation within the medical community.
In summary, the patient outcomes and success rates for cryoablation in treating advanced renal cell carcinoma are quite promising. With high efficacy, lower complications, and quicker recovery times, this treatment offers a viable alternative to more invasive surgical options. As medical technology continues to advance, it is expected that cryoablation techniques will become even more refined, further boosting its success rates and cementing its place in the arsenal against RCC.
Future of Cryoablation in Oncology
Looking ahead, the future of cryoablation in treating advanced renal cell carcinoma (RCC) holds immense promise. Medical researchers and oncologists are continuously exploring how to refine and expand this technique. One of the most exciting developments is the integration of cryoablation with other advanced therapies such as immunotherapy and targeted therapies. This combination approach could enhance the body's immune response against kidney cancer, potentially leading to more effective and durable outcomes.
In the pipeline, there are multiple studies focused on improving the precision of cryoablation. Enhanced imaging technologies like real-time MRI and 3D ultrasound guidance are being tested to provide better visualization of the tumor during the procedure. This would allow for more accurate placement of the cryo-probes, minimizing the risk to surrounding healthy tissues. By increasing the accuracy and safety of the treatment, these technological advancements could make cryoablation even more viable for patients who were previously considered ineligible.
Another exciting area of research is the development of next-generation cryo-probes designed to deliver even colder temperatures with greater control. This might boost the effectiveness of the ablation, reducing the likelihood of cancer recurrence. Clinical trials are currently underway to validate these new tools, and the preliminary results are promising. For instance, a recent study showed that patients treated with advanced cryo-probes had a significantly higher rate of complete tumor destruction compared to traditional methods.
The role of artificial intelligence (AI) in enhancing cryoablation cannot be understated. AI algorithms are being developed to analyze patient data and predict the best approach for each individualized treatment. This could lead to personalized cryoablation strategies tailored to the specific characteristics of a patient's tumor, ultimately improving success rates. Imagine a future where AI assists surgeons by suggesting the optimal probe placement and freezing patterns to maximize treatment efficacy while minimizing risks.
Patient-centric care is also a crucial focus for the future. Emerging telemedicine technologies are making it easier for patients to consult with specialists regardless of their geographical location. Virtual consultations could allow patients to receive expert opinions on the feasibility and benefits of cryoablation without the need for extensive travel. Additionally, wearable health monitoring devices can provide continuous data on a patient's recovery progress, allowing for timely interventions if any complications arise post-procedure.
Funding and policy support will play a significant role in the future of cryoablation in oncology. Increased investment in research and development, coupled with supportive healthcare policies, could accelerate the adoption of cryoablation as a standard treatment option for advanced RCC. Advocacy from patients and healthcare professionals alike is essential for driving these changes. As awareness grows and more success stories emerge, we can expect greater acceptance and integration of cryoablation into mainstream cancer treatment protocols.
"With advancements in imaging and AI, the future of cryoablation in oncology looks brighter than ever. Patients stand to benefit from more precise, effective, and accessible treatments," says Dr. Emily Thompson, a leading oncologist.
Considering all these factors, it's clear that the future of cryoablation in treating kidney cancer is not just hopeful but dynamic. From technological advancements to patient-focused innovations, the landscape of oncology is set to incorporate cryoablation more prominently. As we continue to uncover the full potential of this method, the possibilities for improving patient outcomes and transforming cancer care are truly exciting.



James Knight
September 9, 2024 AT 15:30Honestly, the hype around cryoablation feels like a marketing gimmick more than a real breakthrough. Sure, freezing a tumor sounds cool, but the data isn’t blowing my mind. I’ve seen patients bounce back faster, yet the long‑term survival numbers are still murky. It’s almost as if the industry wants us to believe cold is a cure‑all, ignoring the gritty reality of recurrence. Bottom line, I’m not buying the hype without solid evidence.
Ajay D.j
September 9, 2024 AT 17:10From a cultural standpoint, it’s fascinating how cryoablation blends high‑tech imaging with a seemingly simple physical principle. I’ve read patients describe the experience as surprisingly gentle, which can motivate others hesitant about surgery. While I prefer to stay quiet, I feel compelled to point out that less invasive options often reduce the psychological burden of treatment. Keep an eye on the evolving data, and don’t forget that community support plays a huge role in recovery.
Dion Campbell
September 9, 2024 AT 18:33When evaluating the contemporary landscape of renal cell carcinoma therapeutics, one must first acknowledge the ontological shift engendered by percutaneous ablative modalities. Cryoablation, in particular, epitomises an elegant confluence of thermodynamic principles and image‑guided precision. The operative premise-that rapid induction of intracellular ice crystals precipitates irreversible cellular apoptosis-has been substantiated across a spectrum of oncologic trials. Moreover, the method’s capacity to preserve peri‑tumoral parenchyma aligns synergistically with the overarching paradigm of nephron‑sparing surgery. Nevertheless, the discourse surrounding its efficacy is frequently obfuscated by anecdotal exuberance. Robust, randomized controlled investigations reveal that for tumours inferior to four centimetres, cryoablation yields oncologic outcomes approximating those of partial nephrectomy. In contrast, lesions exceeding this dimensional threshold demonstrate a modest attenuation in local control rates, thereby necessitating adjunctive systemic therapy. From a procedural perspective, the deployment of argon‑based cryoprobes engenders temperatures plummeting below –40 °C, effectuating a well‑defined ice ball visualised via computed tomography. The subsequent thaw cycle accentuates vascular thrombosis, further consolidating tumouricidal effect. Crucially, the technique imposes negligible hemodynamic perturbations, rendering it amenable to patients with comorbid cardiovascular disease. Critically, the longitudinal survivorship data, whilst encouraging, remain heterogeneous owing to variable follow‑up protocols. It is incumbent upon the multidisciplinary team to integrate histopathologic heterogeneity, molecular profiling, and patient‑centred outcomes when selecting cryoablation. Future investigations focusing on real‑time thermometry and AI‑driven probe navigation are poised to ameliorate residual uncertainties. Ultimately, the prudent clinician will harness these advancements while maintaining vigilance against overextension of indications.
Burl Henderson
September 9, 2024 AT 19:40The data you highlighted underscores the necessity of integrating volumetric ablation metrics with renal functional indices. In practice, leveraging contrast‑enhanced CT perfusion can quantify both the ice‑ball extent and the residual perfusion deficit, thereby informing post‑procedure surveillance protocols. Collaborative protocols between interventional radiology and uro‑oncology teams will streamline patient selection and minimize procedural redundancies. Moreover, adopting standardized reporting nomenclature, such as the RFA–CRYO classification, facilitates cross‑institutional meta‑analyses and furthers evidence‑based refinement of the technique.
Leigh Ann Jones
September 9, 2024 AT 21:03Honestly, I’ve read the same boilerplate about cryoablation’s benefits a hundred times, and it just feels like a rehash of the same talking points without any fresh insight. The notion that “minimal invasiveness” automatically translates to superior outcomes is an oversimplification that ignores the nuanced reality of tumor biology, patient heterogeneity, and long‑term follow‑up data. While the procedure certainly reduces incision size and hospital stay, it doesn’t magically eradicate the underlying risk of metastatic spread, which remains a persistent concern in advanced RCC. I’m also weary of the marketing gloss that suggests a one‑size‑fits‑all solution, especially when the literature still debates the optimal tumor size threshold for effective ablation. Moreover, the financial implications, including device costs and the need for specialized imaging suites, are often downplayed in these enthusiastic overviews. From a pragmatic standpoint, many community hospitals lack the requisite infrastructure, forcing patients to travel or settle for suboptimal care. In short, the hype occasionally outpaces the hard evidence, and a more balanced, critically‑appraised perspective would serve the oncology community better.
Sarah Hoppes
September 9, 2024 AT 22:10What they don’t tell you is that the big pharma giants are using cryoablation as a testbed for covert data mining, feeding patient outcomes into hidden algorithms that decide who gets the next drug trial, all while the public is left in the dark.
Robert Brown
September 9, 2024 AT 23:00This is nothing but a glorified ice stick.
Erin Smith
September 9, 2024 AT 23:50Hey, maybe give it a chance its less scary than you think and you might actually feel better after it
George Kent
September 10, 2024 AT 00:40Listen, the idea that cryoablation is some kind of global conspiracy is absolutely preposterous!!! The science is sound, the results are reproducible, and the medical community has embraced it with open arms!!! 🇺🇸🥶💉!! It is not a plot by any shadowy cabal, it is a legitimate, evidence‑based treatment that saves lives! Let us reject the baseless myths and focus on the facts!!! 👏👏👏
Jonathan Martens
September 10, 2024 AT 01:30Sure, because adding extra exclamation points magically makes the procedure more effective
Jessica Davies
September 10, 2024 AT 02:20While many hail cryoablation as the future, I maintain that the enthusiasm is misplaced; the limited data on long‑term oncologic control suggests we are merely putting a band‑aid on a problem that demands more comprehensive systemic strategies.